Bell Palsy
What is Bell palsy?
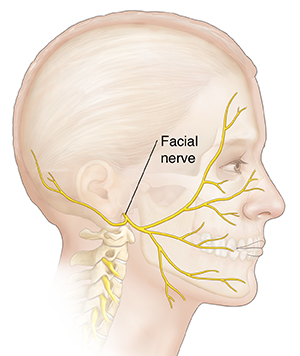
Bell palsy is an unexplained episode of facial muscle weakness or paralysis. It begins
suddenly and can get worse over 48 hours. This condition results from damage to the
facial nerve (the 7th cranial nerve). Pain and discomfort usually occur on one side
of the face or head.
Bell palsy can affect anyone at any age. It occurs most often in pregnant women, and
in people who have diabetes, influenza, a cold, or another upper respiratory ailment.
Bell palsy affects men and woman equally. It's less common before age 15 or after
age 60.
Bell palsy is not considered permanent. But in rare cases, it doesn't disappear. Currently,
there's no known cure for Bell palsy. But recovery usually begins 2 weeks to 6 months
from the start of the symptoms. Most people with Bell palsy recover full facial strength
and expression.
What causes Bell palsy?
The cause of Bell palsy is not known. It's thought that it may be due to inflammation
that is directed by the body's immune system against the nerve controlling movement
of the face. Bell palsy is sometimes linked to the following:
What are the symptoms of Bell palsy?
These are the most common symptoms of Bell palsy:
-
Disordered movement of the muscles that control facial expressions, such as smiling,
squinting, blinking, or closing the eyelid
-
Headache
-
Tearing
-
Drooling
-
Loss of the sense of taste on the front 2/3 of the tongue
-
Hypersensitivity to sound in the affected ear (hyperacusis)
-
Inability to close the eye on the affected side of the face
The symptoms of Bell palsy may look like other health problems, such as Guillain-Barre
syndrome, myasthenia, and multiple sclerosis. Always see your healthcare provider
for a diagnosis.
How is Bell palsy diagnosed?
Your healthcare provider can usually diagnose Bell palsy by looking at your symptoms.
There are no specific tests used to diagnose Bell palsy. But your healthcare provider
may order tests to rule out other conditions that can cause similar symptoms and to
determine the extent of nerve involvement or damage. These tests may include:
-
Electromyography to determine the extent of the nerve involvement
-
Blood tests to determine if another condition, such as diabetes or Lyme disease, is
present
-
MRI or CT scan to find out if there is a structural cause for your symptoms
How is Bell palsy treated?
If a specific cause for Bell palsy is identified, such as infection, that cause will
be treated. Otherwise, the symptoms are treated as needed.
One treatment usually advised is protecting the eye from drying at night or while
working at a computer. Eye care may include eye drops during the day, ointment at
bedtime, or a moisture chamber at night. This helps protect the cornea from being
scratched. This is very important to manage Bell palsy.
Your healthcare provider will prescribe other treatment for your condition based on
the severity of your symptoms and your health history. Other treatment choices include:
-
Steroids to reduce inflammation
-
Antiviral medicine, such as acyclovir
-
Analgesics or moist heat to relieve pain
-
Physical therapy to stimulate the facial nerve
Some people may choose to use alternative therapies in the treatment of Bell palsy,
but there is no proof they make a difference in recovery. Such treatment may include:
What are possible complications of Bell palsy?
Bell palsy usually resolves in time and causes no long-term complications. But during
the illness, most people are unable to close their eye on the affected side of their
face. So it's important to protect the eye from drying at night or while working at
a computer. Eye care may include eye drops during the day, ointment at bedtime, or
a moisture chamber at night. This helps protect the cornea from being scratched.
A small number of people continue to have some weakness of the face. They may need
surgery if the weakness greatly affects the eyelids. Others may have abnormal uncontrolled
movements of the face (spasms) because of abnormal nerve repair.
Living with Bell palsy
Bell palsy usually resolves in time and causes no long-term complications. But it's
important to take medicines as directed. It's also crucial that you protect the affected
eye from drying. Use of eye drops during the day and ointment at bedtime can protect
the cornea from scratching.
When should I call my healthcare provider?
Bell palsy usually starts to improve in 2 weeks. But it may take 3 to 6 months to
return to normal. Call your healthcare provider if you don't get better, you have
new symptoms, or your symptoms get worse.
Key points about Bell palsy
-
Bell palsy is an unexplained episode of facial muscle weakness or paralysis that usually
goes away on its own and causes no complications.
-
The cause of Bell palsy is unknown. But it's thought to be caused by inflammation
affecting the body’s immune system. It's linked to other conditions, such as diabetes.
-
Symptoms of facial weakness or paralysis get worse over the first few days and start
to improve in about 2 weeks.
-
It can take 3 to 6 months to fully go away.
-
Medicine and eye care are important in treating Bell palsy.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells
you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments,
or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also
know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that
visit.
-
Know how you can contact your healthcare provider if you have questions, especially
after office hours or on weekends.