Heart Block
Clinical History
The patient is a 13-month-old African American female child delivered at 38 4/7 weeks gestation to a 22 year old G3 P0020 mom, who was blood group A positive with a negative maternal blood antibody screen, syphilis screen nonreactive, Hepatitis B screen negative, HIV screen negative, rubella screen immune, and Group B Streptococcus culture status unknown. The mother's medications during pregnancy included prenatal vitamins, hydralazine, Procardia, calcium and betamethasone given three months prior to delivery for threatened preterm labor. The pregnancy was complicated by chronic hypertension, trichomonas infection and systemic lupus erythematosus with a positive ANA screen, detectable anti-RO/SS-A, and anti-LA/SS-B antibodies along with a weak anti-RNP antibody screen. The patient was diagnosed with fetal heart block in utero at approximately 20 weeks gestation following routine ultrasound, which demonstrated fetal bradycardia. At birth, the infant was 2530 grams, with APGARS of 8 and 8. She was cyanotic, crying, and her heart rate was 50 to 60 beats per minute. She was admitted to the neonatal intensive care unit (NICU) due to congenital heart block with ventricular bradycardia. In the NICU, her oxygen saturation was 80% on room air and she demonstrated tachypnea and her physical exam was positive for bradycardia without murmur. A chest x-ray demonstrated cardiomegaly, and increased interstitial markings, consistent with retained fetal lung fluid. An electrocardiogram revealed an atrial rate of 130 beats per minute with a ventricular rate of 41 beats per minute. It was determined that although the baby’s capillary refill and effusion were normal, her extreme bradycardia warranted cardiac pacing. As a result, the patient underwent epicardial DDD pacemaker placement at 3 days of life.
During her life, the patient's growth and development remained appropriate for age. She developed no cardiovascular symptoms. However, she was diagnosed with retinal detachment at approximately 7 months of age, and glaucoma and microphthalmia of the left eye status post diode cyclophotocoagulation at approximately 11 months. Her pacemaker continually demonstrated good function and thresholds and arrangements for transtelephonic monitoring were made.
The patient was in her usual state of health until three days prior to admission when she developed a cough and congestion, becoming increasingly distressed with alternating lethargy. She developed a temperature of 101.5 and attempts to treat her at home were unsuccessful. A visit to her pediatrician resulted in her transport to the emergency department, where she was treated with Ibuprofen and Ceftriaxone. Unfortunately, her condition continued to deteriorate and she became unresponsive. Despite extensive resuscitation efforts, the patient was pronounced dead.
Gross Description
At the time of autopsy, a cardiac pacemaker was identified with leads attached to the right atrial and ventricular walls externally. The heart was globular and enlarged and the epicardial surface, underlying the pacer leads, was irregular and firm (Figure 1). There was left ventricular hypertrophy with left ventricular dilatation. The coronary arteries demonstrated right dominance with no plaques or obstructions. The endocardial surfaces were without lesion. The foramen ovale was closed and no valvular abnormalities were identified.
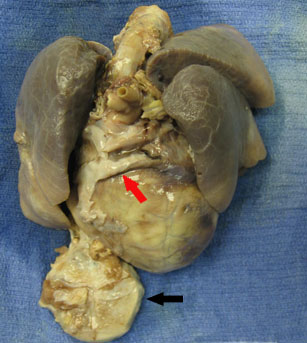
Figure 1: Heart and lung block demonstrating enlarged, globular heart and pacer (black arrow) encased in fibrous tissue. White fibrous tissue is also present overlying the pacer leads (red arrow).
Histologic Description
The epicardial surface demonstrated moderate interstitial fibrosis, particularly in the areas underlying the pacer leads. Mild to moderate interstitial fibrosis was identified in the right myocardium while 40 to 50% of the left ventricular myocardium demonstrated moderate interstitial fibrosis. There was enlargement of the left ventricular cardiac myocytes. No significant inflammatory infiltrate was identified.
Discussion
Initially reported in 1901 (1), congenital complete heart block is identified in approximately 1 of every 20,000 live born infants (2). This condition may occur in the presence or absence of structural heart disease and is associated with a high morbidity and mortality. Diagnosis, as in our case, usually occurs between 16 and 24 weeks gestation and requires a high index of suspicion. The condition is typically identified when routine obstetrical ultrasound for fetal heart sounds detects bradycardia (3).
Hull et al. reported a probable association between congenital complete heart block and maternal connective tissue disease, particularly systemic lupus erythematosus in 1966, hypothesizing that the condition could be due to the transplacental transmission of maternal autoantibodies (4), a pathogenetic mechanism now widely accepted, although the exact causation is not completely understood. In fact, anti-Ro/SS-A and anti-La/SS-B antibodies have been detected in both the mothers and children with complete congenital heart block and have been shown to be efficiently transported across the placenta. Myocarditis, hemorrhage and necrosis are possible in the presence of these antibodies, which may result in fibrosis and even calcification of the conduction system (5,6).
Boutjdir et al. have also demonstrated that anti-Ro/SS-A and anti-La/SS-B antibodies are arrhythmogenic in the human fetal heart acting through the inhibition of L-type calcium channels. This mechanism was supported by the induction of atrioventricular block in the Langendorff-perfused heart indirectly and by patch-clamp experiments in isolated myocytes directly. The antibodies are also thought to be capable of internalization and degradation of the channel, cell death, and ultimately fibrosis (7).
Morbidity and mortality data indicates that complete congenital heart block is fatal in approximately 16 - 19% of cases, with 27% dying in utero, 45% within the first three months following delivery and 73% within the first year of life. Intrauterine hydrops, low fetal and neonatal heart rates, low birth weight, male gender and neonatal problems attributable to prematurity or neonatal lupus were associated with poor outcomes. Complications of this disease include fetal hydrops, dilated cardiomyopathy and cardiac failure in the absence of hydrops. Early pacemaker placement has been associated with reduced mortality and approximately 63% of live-born children undergo the procedure, one third of which occur within the first nine days of life (3,8).
Numerous studies have investigated the role of prenatal steroid therapy in antibody positive mothers both prior to and following fetal diagnosis. The therapy is thought to reduce inflammation, and hydrops, among other conditions. However, oligohydramnios and hypertension remain possible maternal side effects. Other therapies considered include prophylactic plasmapheresis and fetal pacing with early delivery if compromised ventricular function and/or fetal distress is identified. Postnatal treatment involves management cardiac failure and fetal bradycardia. The heart rate may be temporarily increased by beta agonists like isoprenaline. However, pacemaker placement remains the therapy of choice in symptomatic children (9).
Congenital complete heart block is the most serious manifestation of neonatal lupus erythematous (NLE), which is seen in approximately 2% of infants born to mothers with anti-Ro/SSA and anti-La/SSB antibodies (9). Other conditions associated with NLE include the characteristic annular-polycyclic erythematous plaques, particularly on the face and head, hematological abnormalities such as thrombocytopenia and hepatobiliary findings including hepatomegaly and elevated transaminase levels (10). Most symptoms, except for the complications associated with the cardiac manifestations, usually resolve within the first year of life.
Although, anti-Ro/SSA and anti-La/SSB serology tests were not performed on our patient, the clinical presentation in this case is highly suggestive of congenital complete heart block as a result of neonatal lupus erythematosus. The left ventricular dilatation identified grossly and the diffuse moderate interstitial fibrosis present histologically were also consistent with this diagnosis, despite the absence of myocarditis. Since the patient was 13 months old at the time of her death, additional manifestations were not anticipated and none were identified at the time of autopsy. The acute bronchopulmonary pneumonia, which resulted in her death, was most likely unrelated to her history of NLE.
Nadia Granger, M.D., December 2009
References
-
Morquio L. Sur une maladie infantile et familiale characterisee par des modifications permanentes du pouls des attaques syncopales et eptileptiformes et la mort subite. Arch Med Inf 1901;4:467-9.
-
Michaelsson M, Engle MA. Congenital complete heart block: an international study of natural history. Cardiovas Clin 1972;4:85-98.
-
Waltuck J, Buyon JP. Autoantibody associated complete heart block: outcome in mothers and children. Ann Intern Med. 1994;120:544-551.
-
Hull D, Binns BAO, Joyce D. Congenital heart block and widespread fibrosis due to maternal erythematosus. Arch Dis Child 1966;41:688-90.
-
Buyon JP. Neonatal lupus. Curr Opin Rheumatol 1996;8:485-90.
-
Michaelsson M. Congenital complete atrioventricular block. Prog Pediatr Cardiol 1995;4:1-7.
-
Boutjdir M, Chen L, et al. Arrhythmogenecity of IgG and anti-52-kD SSA/Ro affinity-purified antibodies from mothers of children with congenital heart block. Circ Res 1997;80:354-62.
-
Eronen M, Siren MK, Ekblad H, et al. Short-and long-term outcome of children with congenital complete heart block diagnosed in utero or as a newborn. Pediatrics 2000; 106:86-91.
-
Jayaprasad N, Johnson F, Venugopal K. Congenital complete heart block and maternal connective tissue disease. Int J Cardiol. 2006 Sep 20;112(2):153-8.
-
Kobayashi R, Mii S, Nakano T, Harada H, Eto H. Neonatal lupus erythematosis in Japan: A review of the literature. Autoimmun Rev. 2009 May;8(6):462-6.