Twin-Twin Transfusion Syndrome (TTFS)
Clinical History
A 36-year-old woman at 22 weeks with a twin pregnancy had an ultrasound that showed monochorionic diamnionic twins with a growth discordance of 31%. According to the ultrasound results, the estimated fetal weight of twin A was in the 80th percentile and the estimated fetal weight of twin B was in the 22nd percentile. In accordance with the parents’ wishes, the pregnancy was electively terminated for likely twin-twin transfusion syndrome.
Gross Examination
Gross examination of the first fetus (twin A) revealed an immature male fetus with a gestational age of 23 weeks based on foot length of 3.9 cm and body weight of 472 grams and a second immature male fetus (twin B) with a gestational age of 21 weeks based on foot length of 3.6 cm and body weight of 372 grams. Twin A weighed significantly more than twin B (472g vs. 372g) and the organ weights of twin A similarly weighed more than the organ weights of twin B.
The second trimester, single disc placenta of 243 grams had probable artery-vein anastomoses, but no definite anastomoses were identified. Twin A occupied 80-90% of the placental disc and twin B occupied 10-20% of the placental disc.
Microscopic Examination
Microscopic examination of the placenta showed a monochorionic diamnionic placenta (Figure 1 (a) and (b) shows the T-zone (T) and the amnion layers (A) of a monochorionic diamnionic placenta. Compare to Figure 2 that shows an example of a dichorionic diamnionic placenta.) Both twin A and twin B had meconium in the placental membranes.
Twin A’s lungs had thicker vessel walls than twin B. There were no other significant histologic findings.
Click an image to view larger format.
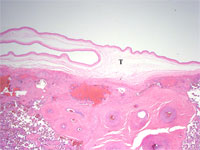
Figure 1a: The T-zone (T) of a
monochorionic diamnionic placenta

Figure 1b: The amnion layers (A) of a
monochorionic diamnionic placenta

Figure 2: An example of a dichorionic
diamnionic placenta with C=chorion and
A=amnion
Discussion
TTTS is a major complication of monochorionic pregnancy having an extremely high perinatal mortality and morbidity if left untreated. This syndrome complicates up to 20% of monochorionic diamnionic pregnancies and accounts for up to 15%-20% of perinatal mortality in all twins. TTTS is thought to be due to blood from one fetus (the donor) transfusing to the other fetus (the recipient) via placental vascular anastomoses. Although the majority of monochorionic placentas have anastomoses, the anastomoses in TTTS are most likely unidirectional arteriovenous anastomoses deep within the shared placenta that result in an imbalance of blood between the twins. The recipient of the transfusion develops hypervolemia and hypertension, which lead to polyuria and polyhydramnios. The transfusion donor develops anemia, hypovolemia, and hypotension, which can lead to oliguria, oligohydramnios, growth deprivation, and decreased movement.
In this case, twin A weighed more than twin B and the organ weights were larger in twin A than in twin B. These findings are consistent with the growth discordance found on the ultrasound and in TTTS. Grossly, the placenta did not have any identifiable anastomoses. However, it is likely that these anastomoses would be deep in the placenta and thereby difficult to identify. Additionally, twin A had 80-90% of the placental disc territory compared to twin B having only 10-20% of the placental disc territory. This large discrepancy in placenta territory is another feature of TTTS. Another gross finding found in TTTS, although not evident in this case, is that the donor twin tends to be pale and anemic while the recipient tends to be edematous and polycythemic.
Microscopically, twin A’s lungs had thicker vessel walls than twin B’s lungs consistent with twin A being the more volume overloaded recipient twin. Both twin A and twin B’s membranes had meconium, a sign that both of the twins were stressed. Although not in this case, the recipient heart weight often may be 2 to 4 times that of the donor due not only to the general growth discrepancy but also to the increased work load associated with the hypervolemia and hypertension that the recipient often develops. Also, the glomeruli are often enlarged, up to twice normal size in the recipient twin, and they are often normal or reduced in size in the donor.
Treatment for TTTS is difficult and perinatal morbidity remains high in the survivors of treated TTTS. Although the treatment of TTTS with serial amnioreduction and improvements in neonatal care have resulted in neonatal survival rates of 60-70%, the survivors still have significant risks of cardiac, renal, and neurologic complications.
Kristina Wolf Subik, Student Fellow 2005
References
-
Cincotta R, Fisk N. Current Thoughts on Twin-Twin Transfusion Syndrome. Clinical Obstetrics and Gynecology. 1997; 40(2):290-302.
-
Cotran, R, Kumar, V, Collins, T, et al. Robbins Pathologic Basis of Disease. 1999; 1081.
-
King D, Sobin L, Stocker J, Wagner B. Placental Pathology, Fascicle 3, Atlas of Nontumor Pathology, American Registry of Pathology, 2004, 261-268.