News
20242023202220202019
New Imaging Method Illuminates Oxygen's Journey in the Brain
Thursday, March 28, 2024
The human brain consumes vast amounts of energy, which is almost exclusively generated from a form of metabolism that requires oxygen. While the efficient and timely delivery of oxygen is known to be critical to healthy brain function, the precise mechanics of this process have largely remained hidden from scientists.
A new bioluminescence imaging technique, described today in the journal Science, has created highly detailed, and visually striking, images of the movement of oxygen in the brains of mice. The method, which can be easily replicated by other labs, will enable researchers to more precisely study forms of hypoxia in the brain, such as the denial of oxygen to the brain that occurs during a stroke or heart attack. The new research tool is already providing insight into why a sedentary lifestyle may increase risk for diseases like Alzheimer’s.
“This research demonstrates that we can monitor changes in oxygen concentration continuously and in a wide area of the brain,” said Maiken Nedergaard, co-director of the Center for Translational Neuromedicine (CTN), which is based at both the University of Rochester and the University of Copenhagen. “This provides us a with a more detailed picture of what is occurring in the brain in real time, allowing us to identify previously undetected areas of temporary hypoxia, which reflect changes in blood flow that can trigger neurological deficits.”
Read More: New Imaging Method Illuminates Oxygen's Journey in the BrainNedergaard Recognized with Nakasone Award for Pioneering Research
Tuesday, March 26, 2024
Maiken Nedergaard, MD, DMSc, has been recognized by the International Human Frontier Science Program Organization (HFSPO) with its 2024 Nakasone Award for her “groundbreaking discovery and exploration” of the glymphatic system, the brain’s unique waste removal system, and the role that sleep plays in its function.
“Dr. Nedergaard forever changed the way we understand sleep as an essential biological function that promotes brain health and plays a crucial role in preventing diseases, such as Alzheimer’s, Parkinson’s, and Huntington’s diseases,” said HFSPO secretary-general Pavel Kabat. “It is a fundamental discovery worthy of being honored with the 2024 HFSPO Nakasone Award.”
Nedergaard is co-director for the Center for Translational Neuromedicine, which maintains research facilities at the University of Rochester Medical Center and the University of Copenhagen. In 2012, her lab first described the glymphatic system, a previously unknown network of channels that piggybacks on blood vessels. The system is used to transport cerebrospinal fluid deep into brain tissue and flush away toxic waste, including beta amyloid and tau, two proteins associated with Alzheimer’s disease.
Read More: Nedergaard Recognized with Nakasone Award for Pioneering ResearchPulling the Plug on Brain Injury
Wednesday, November 15, 2023
Manipulating Fluid Flows Could Save Lives, Improve Recovery Post-TBI
Cerebral edema, the dangerous brain swelling that occurs after traumatic brain injury (TBI), can increase risk of death tenfold and significantly worsen prospects for recovery in brain function. In extreme cases, surgeons will remove a portion of the skull to relieve pressure, but this has significant risks and is not viable for the vast majority of TBI cases. Physicians have very few tools at their disposal that are effective in treating cerebral edema, which is one of the leading causes of in-hospital deaths and is associated with long-term neurological disability.
New research appearing today in the journal Nature could change all that, showing that a cocktail of drugs already approved to treat high blood pressure quickly reduces brain swelling and improves outcomes in animal models of brain injury.
“Our research shows that cerebral edema is the consequence of impaired fluid flow through the glymphatic system and its associated lymphatic drainage,” said Maiken Nedergaard, MD, DMSc, co-director of the University of Rochester Center for Translational Neuromedicine and senior author of the study. “This impairment is under adrenergic control, and can therefore be rescued pharmacologically by broadly inhibiting adrenergic receptors. Because these drugs are already being used clinically and have observed neurological benefits, there is the potential to move quickly to clinical studies to confirm these findings.”
The glymphatic system holds key to relieving brain pressure
The glymphatic system was first described by Nedergaard’s lab in 2012 as the brain’s unique waste removal process. Since then, a growing understanding of the mechanics of the system–aided by advanced imaging technologies and AI-driven models of fluid dynamics—has allowed researchers to better predict and manipulate the movement of cerebrospinal fluid (CSF) in the central nervous system. This research has opened new possibilities to treat Alzheimer’s and other neurological disorders and more effectively deliver and distribute drugs in the central and peripheral nervous system, including the inner ear.
The new study points to the potential to repurpose the glymphatic system to act as an emergency pressure release valve. Cerebral edema is a common consequence of moderate and severe cases of TBI. “In other parts of the body, edema helps with tissue repair, but because of the skull, the brain has limited capacity for expansion. As a result, pressure increases, blood supply decreases, and debris and toxic proteins are trapped at the injury site, compounding the damage and impairing recovery,” said Rashad Hussain, PhD, an assistant professor in the Center for Translational Neuromedicine and first author of the study.
Read More: Pulling the Plug on Brain InjuryTrading Sickness for Health: Swapping Brain Cells Points to New Huntington's Therapies
Monday, July 17, 2023
New research appearing in the journal Nature Biotechnology answers important questions about the viability of treatments that seek to replace diseased and aged cells in the central nervous system with healthy ones. Its findings have implications for a number of neurological and psychiatric disorders—including Huntington’s disease, amyotrophic lateral sclerosis (ALS), and schizophrenia—that have been linked to glia, a population of cells that support brain health and function.
“A broad variety of disorders we associate with neuronal loss now appear to be caused by dysfunctional glial cells,” said Steve Goldman, MD, PhD, co-director of the Center for Translational Neuromedicine at the University of Rochester lead author of the new study. “This makes these diseases attractive targets for stem and progenitor cell-based therapies.”
The new study describes the ability of human glial progenitor cells–precursor cells that can give rise to both astrocytes and oligodendrocytes, the two major types of glia—to compete with one another in the adult brain, and the competitive advantage of young and healthy cells over aged and diseased cells.
Read More: Trading Sickness for Health: Swapping Brain Cells Points to New Huntington's TherapiesAn Unexpected Doorway into the Ear Opens New Possibilities for Hearing Restoration
Wednesday, June 28, 2023
An international team of researchers led by the co-director of the Center for Translational Neuromedicine developed a new method to deliver drugs into the inner ear. It harnesses the natural flow of fluids in the brain and employs a little-understood back door into the cochlea.
Read More: An Unexpected Doorway into the Ear Opens New Possibilities for Hearing RestorationImages capture unseen details of the synapse
Wednesday, June 14, 2023
Scientists have created one of the most detailed 3D images of the synapse, the important juncture where neurons communicate with each other through an exchange of chemical signals. These nanometer scale models will help scientists better understand and study neurodegenerative diseases such as Huntington’s disease and schizophrenia.
The new study appears in the journal PNAS and was authored by a team led by Steve Goldman, MD, PhD, co-director of the Center for Translational Neuromedicine at the University of Rochester and the University of Copenhagen. The findings represent a significant technical achievement that allows researchers to study the different cells that converge at individual synapses at a level of detail not previously achievable.
“It is one thing to understand the structure of the synapse from the literature, but it is another to see the precise geometry of interactions between individual cells with your own eyes,” said Abdellatif Benraiss, PhD, a research associate professor in the Center for Translational Neuromedicine and co-author of the study. “The ability to measure these extremely small environments is a young field, and holds the potential to advance our understanding of a number of neurodegenerative and neuropsychiatric diseases in which synaptic function is disturbed.”
Read More: Images capture unseen details of the synapseAnders Jahre Main Award for Medical Research given to Maiken Nedergaard
Tuesday, June 13, 2023
The professor of Neurology and co-director of the Center for Translational Neuromedicine at the University of Rochester and University of Copenhagen received the award from the University of Oslo. Nedergaard was recognized for her research on astrocytes and the glymphatic system, which "has far-reaching implications both for understanding how the brain normally works and what goes wrong when the brain is affected by disease."
Read More: Anders Jahre Main Award for Medical Research given to Maiken NedergaardMaiken Nedergaard's lab just discovered a new part of the brain's waste disposal system
Thursday, January 5, 2023
New Scientist, January 5
The new structure is a fourth membrane, lying on top of the innermost membrane, called the subarachnoid lymphatic-like membrane (SLYM). The SLYM hadn’t been noticed before, partly because the membrane disintegrates when the brain is removed from the skull in post-mortems, says Maiken Nedergaard, a professor of neurology and of neurosurgery and codirector of the Center for Translational Neuromedicine, who helped discover the structure. It is also too thin to be seen in living people via brain-scanning machines.
Read More: Maiken Nedergaard's lab just discovered a new part of the brain's waste disposal systemNew Grant Will Unlock Workings of Glymphatic System
Monday, August 15, 2022
A decade ago, researchers in the lab of Maiken Nedergaard, M.D., D.M.Sc., answered a basic question of biology that up to that point had eluded scientists: how is waste removed from the brain? The discovery of what is now known as the glymphatic system and subsequent research have transformed the way we study a range of neurological disorders and critical brain functions. A new $15 million grant from the National Institutes of Health (NIH) will bring together several teams of researchers to accelerate our understanding of the complex mechanics that control this system, with an eye toward the development of new therapies for diseases like Alzheimer’s.
The new research program will be led by Nedergaard, co-director of the Center for Translational Neuromedicine, and involve scientists and engineers from the University of Rochester, Penn State University, Boston University, and the University of Copenhagen. The research is being funded through The BRAIN Initiative, a massive research program supported by NIH and several other federal research agencies that aims to fill gaps in our current knowledge of the brain’s organization and function.
The glymphatic system – a network of plumbing that runs parallel to blood vessels and pumps cerebral spinal fluid (CSF) through brain tissue to wash away waste – was all but invisible to the scientific world until 2012 when it was first described in a study published in Science Translational Medicine. A paper in the journal Science a year later showed that this system operates primarily while we sleep and removes toxic proteins associated with Alzheimer’s disease. These findings fundamentally changed scientists’ understanding of the biological purpose of sleep and opened the door to potential new ways to treat neurological disorders.
Read More: New Grant Will Unlock Workings of Glymphatic SystemResearch to Treat Neurodegenerative Diseases Advances: URMC Start-up Acquired
Wednesday, November 18, 2020
Oscine Therapeutics -- a biotechnology company that is developing cell-based therapies for neurological disorders based on discoveries made at the University of Rochester Medical Center (URMC) -- has been acquired by Sana Biotechnology for undisclosed terms.
The research behind Oscine is based on decades of work in the lab of Steve Goldman, M.D., Ph.D., professor of Neurology and Neuroscience and co-director of the URMC Center for Translational Neuromedicine. Goldman's research has focused on understanding the basic biology and molecular function of the glial support cells in the central nervous system, devising new techniques to precisely manipulate and sort these cells, and studying how cell replacement could impact the course of neurological diseases. Goldman, who was Oscine's president and scientific founder, joins Sana as senior vice-president and head of Central Nervous System Therapy. He will also remain on the URMC faculty.
Sana Biotechnology, which has operations in Washington, Massachusetts, and California, was created in 2018 with a focus on developing and delivering engineered cells as medicines for patients. The company is led by a team of biotechnology industry veterans and supported by more than $700 million in investment. Last year, the company invested in Oscine's R&D in neurological disorders, in what remains the University of Rochester's largest-ever commercial spin-off.
The exclusive licenses for the portfolio of technologies and equity stake that the University of Rochester held with Oscine have been acquired by Sana. The University and Goldman may continue to receive significant licensing, milestone, and royalty payments from Sana going forward.
"The University of Rochester has been working closely with Dr. Goldman's lab and the Oscine team from its inception," said Scott Catlin, director of UR Ventures, the University's technology transfer office. "We are thrilled with the company's impressive progress and its acquisition by Sana and look forward to continue supporting the commercialization of Dr. Goldman's technologies."
Goldman's research focuses on support cells in the brain called glia. In many neurological diseases -- such as multiple sclerosis, Huntington's, and neuropsychiatric disorders -- these cells either disappear or malfunction. This ultimately leads to the motor, cognitive, and behavioral symptoms of these disorders. Goldman's lab has shown that replacing these sick cells with healthy ones can slow and even reverse disease progression in animal models of these diseases.
The Center for Translational Neuromedicine maintains labs in Rochester and at the University of Copenhagen in Denmark. Goldman's research for cell-based therapies has received relevant support from the National Institute of Neurological Disorders and Stroke, the National Institute of Mental Health, the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation, the Lundbeck Foundation, the Novo Nordisk Foundation, CHDI, and NYSTEM.
Nedergaard Honored for Alzheimer’s Research
Tuesday, September 15, 2020
Maiken Nedergaard, M.D., D.M.Sc. has been awarded the International Prize for Translational Neuroscience of the Gertrud Reemtsma Foundation for her research in the glymphatic system, the brain's unique waste removal process.
Nedergaard's research was recognized by the Foundation for findings that "offer new approaches for treatments and preventive measures for Alzheimer's and other neurodegenerative diseases."
First discovered by researchers in the URMC Center for Translational Neuromedicine in 2012, the glymphatic system piggybacks on blood vessels and pumps cerebrospinal fluid, washing waste from the brain. The accumulation of toxic proteins like beta amyloid are linked neurological disorders, including Alzheimer's disease. Nedergaard's lab has since gone on to show how sleep disruption, age, and injury can impair the brain's ability to effectively remove waste.
Nedergaard was presented the award at a ceremony at the Max Plank Society in Cologne, Germany on September 10.
Circadian Rhythms Help Guide Waste from Brain
Wednesday, September 2, 2020
New research details how the complex set of molecular and fluid dynamics that comprise the glymphatic system -- the brain's unique process of waste removal -- are synchronized with the master internal clock that regulates the sleep-wake cycle. These findings suggest that people who rely on sleeping during daytime hours are at greater risk for developing neurological disorders.
"These findings show that glymphatic system function is not solely based on sleep or wakefulness, but by the daily rhythms dictated by our biological clock," said neuroscientist Maiken Nedergaard, M.D., D.M.Sc., co-director of the Center for Translational Neuromedicine at the University of Rochester Medical Center (URMC) and senior author of the study, which appears in the journal Nature Communications.
The findings add to a growing understanding of the operation and function of glymphatic system, the brain's self-contained waste removal process which was first discovered in 2012 by researchers in the Nedergaard's lab. The system consists of a network of plumbing that follows the path of blood vessels and pumps cerebrospinal fluid (CSF) through brain tissue, washing away waste. Research a few years later showed that the glymphatic system primarily functions while we sleep.
Since those initial discoveries, Nedergaard's lab and others have shown the role that blood pressure, heart rate, circadian timing, and depth of sleep play in the glymphatic system's function and the chemical signaling that occurs in the brain to turn the system on and off. They have also shown how disrupted sleep or trauma can cause the system to break down and allow toxic proteins to accumulate in the brain, potentially giving rise to a number of neurodegenerative diseases, such as Alzheimer's.
Read More: Circadian Rhythms Help Guide Waste from Brain‘A Rinsing of the Brain.’ New Research Shows How Sleep Could Ward Off Alzheimer's Disease
Thursday, August 6, 2020
Each of us carts around a 3-lb. universe that orchestrates everything we do: directing our conscious actions of moving, thinking and sensing, while also managing body functions we take for granted, like breathing, keeping our hearts beating and digesting our food. It makes sense that such a bustling world of activity would need rest. Which is what, for decades, doctors thought sleep was all about. Slumber was when all the intricate connections and signals involved in the business of shuttling critical brain chemicals around went off duty, taking time to recharge. We're all familiar with this restorative role of sleep for the brain--pulling an all-nighter or staying awake during a red-eye flight can not only change our mood, but also affect our ability to think clearly until, at some point, it practically shuts down on its own. When we don't get enough sleep, we're simply not ourselves.
Yet exactly what goes on in the sleeping brain has been a biological black box. Do neurons stop functioning altogether, putting up the cellular equivalent of a Do Not Disturb sign? And what if a sleeping brain is not just taking some well-deserved time off but also using the downtime to make sense of the world, by storing away memories and captured emotions? And how, precisely, is it doing that?
A year later, a biological explanation for why poor sleep might be linked to Alzheimer's emerged. Dr. Maiken Nedergaard, co-director of the Center for Translational Neuromedicine at the University of Rochester, identified a previously ignored army of cells that is called to duty during sleep in the brains of mice and acts as a massive pump for sloshing fluid into and out of the brain. This plumbing system, which she dubbed the "glymphatic system" (it works in parallel to the lymph system that drains fluid from other tissues in the body), seemed to perform a neural rinsing of the brain, swishing out the toxic proteins generated by active neurons (including those amyloid fragments) and clearing the way for another busy daily cycle of connecting and networking.
Taken together with Holtzman's discovery that levels of amyloid spiked during the day and dropped during sleep, Nedergaard's findings gave further credence to the theory that sleep might perform a housekeeping function critical for warding off diseases like Alzheimer's. "These results very much support the notion that one of the roles of sleep is to actually accelerate the clearance of beta amyloid from the brain," says Nora Volkow, director of the U.S. National Institute on Drug Abuse.
Animal Study Shows Human Brain Cells Repair Damage in Multiple Sclerosis
Tuesday, May 19, 2020
A new study shows that when specific human brain cells are transplanted into animal models of multiple sclerosis and other white matter diseases, the cells repair damage and restore function. The study provides one of the final pieces of scientific evidence necessary to advance this treatment strategy to clinical trials.
"These findings demonstrate that through the transplantation of human glial cells, we can effectively achieve remyelination in the adult brain, " Steve Goldman, M.D., Ph.D., professor of Neurology and Neuroscience at the University of Rochester Medical Center (URMC), co-director of the Center for Translational Neuromedicine, and lead author of the study. "These findings have significant therapeutics implications and represent a proof-of-concept for future clinical trials for multiple sclerosis and potential other neurodegenerative diseases."
The findings, which appear in the journal Cell Reports, are the culmination of more than 15 years of research at URMC understanding support cells found in the brain called glia, how the cells develop and function, and their role in neurological disorders.
Goldman's lab has developed techniques to manipulate the chemical signaling of embryonic and induced pluripotent stem cells to create glia. A subtype of these, called glial progenitor cells, gives rise to the brain's main support cells, astrocytes and oligodendrocytes, which play important roles in the health and signaling function of nerve cells.
Maiken Nedergaard honored by American Stroke Association for dedication to stroke research
Monday, February 24, 2020
Maiken Nedergaard, M.D., D.M.Sc., co-director of the Center for Translational Neuromedicine, professor in the Departments of Neurology, Neuroscience and Neurosurgery, received the Thomas Willis Lecture Award from the American Stroke Association. The award honors Nedergaard's career of significant contributions to the basic science of stroke research.
The Nedergaard lab is dedicated to deciphering the role of neuroglia, cell types that constitute half of the entire cell population of the brain and spinal cord.
Last month, the lab published research showing that during a stroke the glymphatic system goes awry, triggers edema and drowns brain cells. In 2012, Nedergaard and her colleagues first described the glymphatic system, a network that piggybacks on the brain's blood circulation system and is comprised of layers of plumbing, with the inner blood vessel encased by a 'tube' that transports cerebrospinal fluid (CSF). The system pumps CSF through brain tissue, primarily while we sleep, washing away toxic proteins and other waste.
The Thomas Willis Award honors the prominent British physician credited with providing the first detailed description of the brain stem, the cerebellum and the ventricles, with extensive hypothesis about the functions of these brain parts. The award recognizes contributions to the investigation and management of stroke basic science.
Nedergaard was one of eleven leading scientists honored for their work by the American Stroke Association. The awards were given during the American Stroke Association's International Stroke Conference in Los Angeles.
New Funding Boosts URMC Biotech Start-Up for Neurological Disorders
Monday, June 10, 2019
Oscine Therapeutics, a new biotechnology company based on discoveries made and developed at the University of Rochester Medical Center (URMC) has received a significant multi-year investment to support both research and development of cell-based therapies for neurological disorders. The funding represents the largest-ever investment in a URMC start-up company.
The new venture is based on decades of research in the lab of Steve Goldman, M.D., Ph.D., co-director of the URMC Center for Translational Neuromedicine. Goldman's work has focused on understanding the basic biology and molecular function of support cells in the central nervous system, devising new techniques to precisely manipulate and sort these cells, and studying how cell replacement could impact the course of neurological diseases.
Goldman has developed techniques to manipulate the chemical signaling of embryonic and induced pluripotent stem cells to create the brain's support cells, called glia. A subtype of these, called glial progenitor cells, gives rise to the brain's main support cells, astrocytes and oligodendrocytes, which play important roles in the health and signaling function of nerve cells.
"Neurological disorders are complex diseases, but in many instances it appears that faulty support cells of the brain are driving the disease process," said Goldman, the URMC Distinguished Professor of Neuroscience and Neurology. "These diseases represent promising targets for cell-replacement therapies because we know a great deal about the role these cells play, how to create them, and how to get them to the areas of the brain where they are needed."
The investment in Oscine is being made by Sana Biotechnology, a new company focused on creating and delivering engineered cells as medicines for patients. The company is led by a team of biotechnology industry veterans with extensive experience in cell therapy, gene therapy, and gene editing. The company is backed by visionary investors including Arch Venture Partners, Flagship Pioneering, and F-Prime Capital Partners.
Mouse Study: Deep Sleep Helps the Brain Wash Away Toxic Proteins
Friday, March 1, 2019
Deep sleep allows the brain to wash away waste and toxic proteins more efficiently, according to a new mouse study published in the journal Science Advances. The new findings shed light on previous evidence linking Alzheimer's disease with aging and sleep deprivation.
"Sleep is critical to the function of the brain's waste removal system and this study shows that the deeper the sleep, the better," said Maiken Nedergaard, MD, DMSc, co-director of the Center for Translational Neuromedicine at the University of Rochester Medical Center (URMC) and lead author of the study.
"These findings also add to the increasingly clear evidence that quality of sleep or sleep deprivation can predict the onset of Alzheimer's and dementia."
The study suggests that the slow and steady brain and cardiopulmonary activity linked to deep non-REM sleep are optimal for the function of the glymphatic system, the brain's waste removal system. The findings may also explain why some forms of anesthesia can result in cognitive dysfunction in older adults.
Not All Sleep is Equal When It Comes to Cleaning the Brain
Wednesday, February 27, 2019
New research shows how the depth of sleep can impact our brain's ability to efficiently wash away waste and toxic proteins. Because sleep often becomes increasingly lighter and more disrupted as we become older, the study reinforces and potentially explains the links between aging, sleep deprivation, and heightened risk for Alzheimer's disease.
"Sleep is critical to the function of the brain's waste removal system and this study shows that the deeper the sleep the better," said Maiken Nedergaard, M.D., D.M.Sc., co-director of the Center for Translational Neuromedicineat the University of Rochester Medical Center (URMC) and lead author of the study. "These findings also add to the increasingly clear evidence that quality of sleep or sleep deprivation can predict the onset of Alzheimer's and dementia."
The study, which appears in the journal Science Advances, indicates that the slow and steady brain and cardiopulmonary activity associated with deep non-REM sleep are optimal for the function of the glymphatic system, the brain's unique process of removing waste. The findings may also explain why some forms of anesthesia can lead to cognitive impairment in older adults.
Study suggests how high blood pressure might contribute to Alzheimer’s
Monday, January 28, 2019
The brain's system for removing waste is driven primarily by the pulsations of adjoining arteries, University of Rochester neuroscientists and mechanical engineers report in a new study. They also show that changes in the pulsations caused by high blood pressure slow the removal of waste, reducing its efficiency.
This might explain the association between high blood pressure and Alzheimer' disease, the researchers say. Alzheimer's, the most common cause of dementia among older adults, is characterized by abnormal clumps and tangled bundles of fibers in the brain.
The study, reported in Nature Communications, builds upon groundbreaking discoveries about the brain's waste removal system by Maiken Nedergaard, co-director of the University's Center for Translational Neuromedicine. Nedergaard and her colleagues were the first to describe how cerebrospinal fluid is pumped into brain tissue and flushes away waste. Subsequent research by her team has shown that this glymphatic waste removal system is more active while we sleep and can be damaged by stroke and trauma.
This latest research shows "in much greater depth and much greater precision than before" how the glymphatic system functions in the perivascular spaces that surround arteries in the outer brain membrane, says Douglas Kelley, an assistant professor of mechanical engineering and an expert in fluid dynamics. His lab is collaborating with Nedergaard's team as part of a $3.2 million National Institute on Aging grant.
For this study, Humberto Mestre, a PhD student in Nedergaard's lab, injected minute particles in the cerebrospinal fluid of mice, and then used two-photon microscopy to create videos showing the particles as they moved through the perivascular spaces.
How to Get Enough Sleep in 2019
Friday, January 18, 2019
What really happens when you sleep? You may be taking a break from consciousness when you snooze, but not all of your neurons are resting, Veasey says. While you rest, your brain solidifies the synapses involved in the important memories you want to keep (like the name of your new dentist) while pruning the synapses involved in less important memories (such as where you put your keys two nights ago).
Sleep also gives your brain a chance to clear out debris that accumulated during the day. In 2014, a team of scientists led by Maiken Nedergaard at the University of Rochester Medical Center published research suggesting that the brain rids itself of metabolic waste through a kind of plumbing system that works mainly while we sleep. Just as the lymphatic system clears unwanted waste from the rest of the body, what's called the glymphatic system eliminates debris and toxins from the brain and the central nervous system. Skimp on sleep, and this janitorial service can't keep up, so the rubbish starts to accumulate in your noggin.
Study Confirms Central Role of Brain’s Support Cells in Huntington’s, Points to New Therapies
Thursday, December 13, 2018
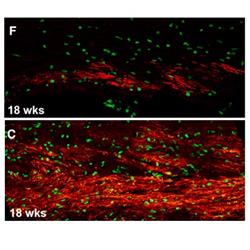 Brains of mice with human glial cells containing Huntington's disease mutation (top image) show significantly less myelin (red) than controls (bottom image).
Brains of mice with human glial cells containing Huntington's disease mutation (top image) show significantly less myelin (red) than controls (bottom image).
New research gives scientists a clearer picture of what is happening in the brains of people with Huntington's disease and lays out a potential path for treatment. The study, which appears today in the journal Cell Stem Cell, shows that support cells in the brain are key contributors to the disease.
"Huntington's is a complex disease that is characterized by the loss of multiple cell populations in the brain," said neurologist Steve Goldman, M.D., Ph.D., the lead author of the study and the co-director of the Center for Translational Neuromedicine at the University of Rochester Medical Center (URMC). "These new findings help pinpoint how the genetic flaw in Huntington's gives rise to glial cell dysfunction, which impairs the development and role of these cells, and ultimately the survival of neurons. While it has long been known that neuronal loss is responsible for the progressive behavioral, cognitive, and motor deterioration of the disease, these findings suggest that it's glial dysfunction which is actually driving much of this process."
Huntington's is a hereditary and fatal neurodegenerative disease characterized by the loss of medium spiny neurons, a nerve cell in the brain that plays a critical role in motor control. As the disease progresses over time and more of these cells die, the result is involuntary movements, problems with coordination, and cognitive decline, depression, and often psychosis. There is currently no way to slow or modify the progression of this disease.
Maiken Nedergaard Recognized for Groundbreaking Research on Glymphatic System
Tuesday, November 13, 2018
Maiken Nedergaard, M.D., D.M.Sc., has been awarded the with the 2018 Eric K. Fernstrom Foundation Grand Nordic Prize for her work that led to the discovery of the brain's unique waste removal system and its role in a number of neurological disorders. Nedergaard maintains labs at the Medical Center and the University of Copenhagen.
In 2012, Nedergaard's lab was the first to reveal the brain's unique process of removing waste, dubbed the glymphatic system, which consists of a plumbing system that piggybacks on the brain's blood vessels and pumps cerebral spinal fluid (CSF) through the brain's tissue, flushing away waste.
Nedergaard's lab has since gone on to show that the glymphatic system works primarily while we sleep, could be a key player in diseases like Alzheimer's, is disrupted after traumatic brain injury, may be enhanced by moderate alcohol consumption, and could be harnessed as a new way to deliver drugs to the brain.
The Eric K. Fernstrom Foundation annually awards the Grand Nordic Prize to a medical research from one of the Nordic Countries. The award was announced during a ceremony on November 7 at Lund University in Sweden.
Study Points to New Method to Deliver Drugs to the Brain
Thursday, October 18, 2018
Researchers at the University of Rochester Medical Center (URMC) have discovered a potentially new approach to deliver therapeutics more effectively to the brain. The research could have implications for the treatment of a wide range of diseases, including Alzheimer's, Parkinson's, ALS, and brain cancer.
"Improving the delivery of drugs to the central nervous system is a considerable clinical challenge," said Maiken Nedergaard M.D., D.M.Sc., co-director of the University of Rochester Medical Center (URMC) Center for Translational Neuromedicine and lead author of the article which appears today in the journal JCI Insight. "The findings of this study demonstrate that the brain's waste removal system could be harnessed to transport drugs quickly and efficiently into the brain."
Many promising therapies for diseases of the central nervous system have failed in clinical trials because of the difficulty in getting enough of the drugs into the brain to be effective. This is because the brain maintains its own closed environment that is protected by a complex system of molecular gateways -- called the blood-brain barrier -- that tightly control what can enter and exit the brain.
While We Sleep, Our Mind Goes on an Amazing Journey
Tuesday, July 17, 2018
A study by Maiken Nedergaard, a professor of neurosurgery, suggests that while we're awake, our neurons are packed tightly together, but when we're asleep, some brain cells deflate by 60 percent, widening the spaces between them. These intercellular spaces are dumping grounds for the cells' metabolic waste—notably a substance called beta-amyloid, which disrupts communication between neurons and is closely linked to Alzheimer's.
Raise a Glass to Your Health
Monday, May 21, 2018
Continue to raise that glass (in moderation, of course) if you want to maximize the health benefits of wine. Recent studies claim a variety of benefits can be linked to low or moderate alcohol consumption, approximately two drinks or less per day. Here are the top five takeaways.
Low levels of alcohol can decrease inflammation and help the brain clear away toxins
Published in the February 2018 issue of the journal Scientific Reports, a study conducted by the University of Rochester Medical Center demonstrated that mice exposed to low levels of alcohol showed less inflammation in the brain and a more efficient glymphatic system, which serves as the brain's waste clearance system. The research may be promising for scientists that study age-related ailments like Alzheimer's and dementia.
"Consumption of alcohol has a 'J' shape curve on health," says Dr. Maiken Nedergaard of the University of Rochester Medical Center and lead author of the study. "Small consumption is beneficial when looking at large populations, whereas high is not."
Brain Science Suggests This Is the Best Position to Sleep In
Thursday, May 17, 2018
Sleep is critical for rest and rejuvenation. A human being will actually die of sleep deprivation before starvation--it takes about two weeks to starve, but only 10 days to die if you go without sleep.
The CDC has also classified insufficient sleep as a public health concern. Those who don't get enough sleep are more likely to suffer from chronic diseases that include hypertension, diabetes, depression, obesity, and cancer.
It's thus vital to get enough shuteye, but it turns out your sleep position also has a significant impact on the quality of rest you get.
In addition to regulating one's appetite, mood, and libido, neuroscientists assert that sleep reenergizes the body's cells, aids in memory and new learning, and clears waste from the brain.
That last one is particularly important. Similar to biological functions in which your body clears waste, your brain needs to get rid of unwanted material. The more clearly it functions, the more clearly you do.
Now, a neuroscience study suggests that of all sleep positions, one is most helpful when it comes to efficiently cleaning out waste from the brain: sleeping on your side.
The study, published in the Journal of Neuroscience, used dynamic contrast-enhanced MRI to image the brain's "glymphatic pathway." This is the system by which cerebrospinal fluid filters through the brain and swaps with interstitial fluid (the fluid around all other cells in the body).
The exchange of the two fluids is what allows the brain to eliminate accumulated waste products, such as amyloid beta and tau proteins. What are such waste chemicals associated with? Among other conditions, Alzheimer's and Parkinson's.
"It is interesting that the lateral [side] sleep position is already the most popular in humans and most animals--even in the wild," said University of Rochester's Maiken Nedergaard. "It appears that we have adapted the lateral sleep position to most efficiently clear our brain of the metabolic waste products that build up while we are awake."
Drinking Alcohol Tied To Long Life In New Study
Thursday, February 22, 2018
Drinking could help you live longer—that's the good news for happy-hour enthusiasts from a study presented last week at the annual meeting of the American Association for the Advancement of Science. According to the study, people who live to 90 or older often drink moderately.
Neurologist Claudia Kawas and her team at the University of California, Irvine, have been studying the habits of people who live until their 90s since 2003. There’s a paltry amount of research on the oldest-old group, defined as 85 and older by the Social Security Administration, and Kawas wanted to delve into the lifestyle habits of those who live past 90. She began asking about dietary habits, medical history and daily activities via survey, wondering if such data could help identify trends among these who lived longest. Ultimately she gathered information on the habits of 1,700 people between the ages of 90-99.
In general, research on alcohol has shown mixed results. A recent study published in Scientific Reports showed that drinking might help clear toxins from the brain. The study was conducted on mice, who were given the human equivalent of two and a half alcoholic beverages.
Dr. Maiken Nedergaard of the University of Rochester Medical Center told Newsweek at the time that alcohol did have real health benefits. “Except for a few types of cancer, including unfortunately breast cancer, alcohol is good for almost everything,” Nedergaard said.
In Wine, There’s Health: Low Levels of Alcohol Good for the Brain
Friday, February 2, 2018
By Mark Michaud
While a couple of glasses of wine can help clear the mind after a busy day, new research shows that it may actually help clean the mind as well. The new study, which appears in the journal Scientific Reports, shows that low levels of alcohol consumption tamp down inflammation and helps the brain clear away toxins, including those associated with Alzheimer's disease.
"Prolonged intake of excessive amounts of ethanol is known to have adverse effects on the central nervous system," said Maiken Nedergaard, M.D., D.M.Sc., co-director of the Center for Translational Neuromedicine at the University of Rochester Medical Center (URMC) and lead author of the study. "However, in this study we have shown for the first time that low doses of alcohol are potentially beneficial to brain health, namely it improves the brain's ability to remove waste."
The finding adds to a growing body of research that point to the health benefits of low doses of alcohol. While excessive consumption of alcohol is a well-documented health hazard, many studies have linked lower levels of drinking with a reduced risk of cardiovascular diseases as well as a number of cancers.