Hiatal Hernia
What is a hiatal hernia?
A hernia is when part of an organ goes through an opening in the muscle wall around
it.
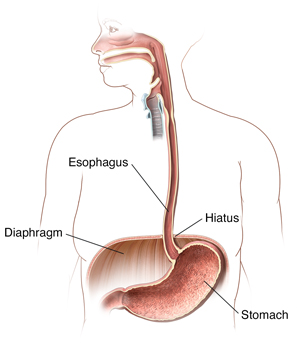
In a hiatal hernia, part of your stomach pushes up into an opening (the hiatus) in
your diaphragm. The diaphragm is the muscle between your belly (abdomen) and your
chest.
In most cases, your food pipe (esophagus) goes through the hiatus and joins your stomach.
But with a hiatal hernia, the top part of your stomach moves up through that opening
into your chest.
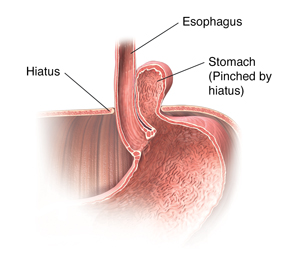
The top part of your stomach gets pinched. Stomach acid can back up (reflux) through
the opening. This may cause heartburn and other symptoms.
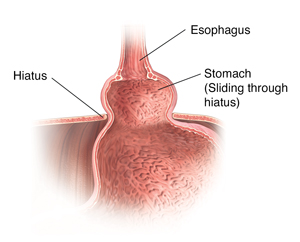
There are two types of hiatal hernias: sliding and paraesophageal.
Sliding hiatal hernia
This type of hernia:
Paraesophageal hernia
This type of hernia:
What causes a hiatal hernia?
Experts don’t know what causes hiatal hernias. Some causes may include:
Who is at risk for a hiatal hernia?
You may be at greater risk for a hiatal hernia if you:
-
Are age 50 or older
-
Are overweight or obese
-
Are pregnant
-
Smoke
What are the symptoms of a hiatal hernia?
In many cases, a hiatal hernia has no symptoms.
Some people do have symptoms. These may include:
Paraesophageal hernias may have more severe symptoms. These can include:
-
Having trouble swallowing sometimes, most often with solid foods
-
Feeling full after eating only a small amount of food
-
Belly (abdominal) or chest pain
-
Abdominal bleeding
-
Blood loss (anemia)
In some cases, a paraesophageal hernia can lead to a medical emergency. The stomach
or abdominal organs may turn or twist, causing very bad pain. There is a danger that
the stomach’s blood supply may be cut off (strangulation). This is an emergency. You
will likely need surgery right away.
The symptoms of a hiatal hernia may look like other health problems. Always see your
healthcare provider to be sure.
How is a hiatal hernia diagnosed?
Your healthcare provider will give you a physical exam. They will look at your past
health.
You may also have tests, including:
-
Chest X-ray. This may show that you have a hiatal hernia.
-
Upper endoscopy, also called EGD (esophagogastroduodenoscopy). This test looks at the lining of your food pipe (esophagus), stomach, and the first
part of your small intestine (the duodenum). It uses a thin, lighted tube called an
endoscope. The tube has a camera at one end. The tube is put into your mouth and throat
while you are sedated. Then it goes into your esophagus, stomach, and duodenum. Your
healthcare provider can see the inside of these organs.
-
Upper GI (gastrointestinal) series or barium swallow. This test looks at the organs of the top part of your digestive system. It checks
your food pipe (esophagus), stomach, and the first part of your small intestine (the
duodenum). You will swallow a metallic fluid called barium. Barium coats the inside
of the esophagus, stomach, and intestines so that they can be seen on an X-ray.
-
Esophageal manometry. This test checks the strength of your esophagus muscles. It can see if you have any
problems with reflux or swallowing. A small tube is put into your nostril, then down
your throat into your esophagus. This measures the pressure that your esophagus muscles
make at rest and during swallowing.
How is a hiatal hernia treated?
Treatment will depend on your symptoms, age, and general health. It will also depend
on how bad the condition is.
In most cases, you won’t need treatment. But you may need medical care if your hernia:
-
Is at risk of being twisted so much that blood supply is cut off to your stomach (strangulation)
-
Is more difficult because of severe GERD (gastroesophageal reflux disease)
-
Is more difficult because of redness and swelling (inflammation) of your esophagus
(esophagitis)
Your healthcare provider may suggest medicines to:
-
Weaken or neutralize stomach acid (antacids)
-
Reduce the amount of acid your stomach makes (H-2 blockers or proton pump inhibitors)
-
Strengthen your lower esophageal sphincter, the muscle that stops stomach acid from
backing up into your esophagus
In severe cases, surgery may also be needed to:
What are possible complications of a hiatal hernia?
In most cases, a hiatal hernia won’t lead to other health problems.
In some cases, it can cause other problems, such as:
-
Severe GERD (gastroesophageal reflux disease)
-
Lung problems or pneumonia because stomach contents have moved up into your esophagus
and into one or both lungs
-
Strangulation of the hernia, cutting off blood flow to your stomach (medical emergency)
What can I do to prevent a hiatal hernia?
Health experts don’t know what causes hiatal hernias. They don’t know how to stop
them from happening.
Living with a hiatal hernia
Follow your healthcare provider’s advice for treating and managing your hiatal hernia.
You may need to make some lifestyle changes, such as:
-
Losing weight if you are overweight or obese
-
Not eating for 3 to 4 hours before going to bed
-
Not bending over right after eating
-
Quitting smoking
-
Elevating the head of your bed while you sleep
When should I call my healthcare provider?
Call your healthcare provider if your symptoms come back after treatment has stopped
them. Let your healthcare provider know if symptoms get worse or you have new symptoms.
Key points about hiatal hernia
-
A hiatal hernia is when part of your stomach pushes up into an opening (the hiatus)
in your diaphragm.
-
There are two types of hiatal hernias: sliding and paraesophageal.
-
Paraesophageal hernias are less common but can be more serious. You may need surgery.
-
Experts don’t know what causes hiatal hernias.
-
In most cases, there are no symptoms.
-
In most cases, no medical care is needed.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells
you.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments,
or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed and how it will help you. Also
know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that
visit.
-
Know how you can contact your healthcare provider if you have questions, especially
after office hours or on weekends.