URMC / Labs / Mooney Lab / Projects / Role of gut microbiome in mediating increased incidence and severity of osteoarthritis in obese
Role of gut microbiome in mediating increased incidence and severity of osteoarthritis in obese patients
Osteoarthritis (OA), a degenerative joint disease, afflicts 31 million people in the US, with a global prevalence of disease recently estimated to exceed 250 million. Unfortunately, the only clinically accepted treatment strategies are palliative, with no disease modifying OA drug approved for use in humans. Thus, an effective treatment strategy for OA is a critical unmet need.
Obesity, a key risk factor for the development of OA, has become a global epidemic due to decreased physical activity and the consumption of the typical Western diet. Currently, 66 percent of all adults diagnosed with OA are overweight, obese or obese/type 2 diabetic. Our clinical and animal studies suggest the association between obesity and OA is rooted in obesity-associated systemic and local inflammation. Synovial membrane surrounding the joint in obese patients and animal models is hyperplastic with increased abundance of activated macrophages and other inflammatory cells together with elevated inflammatory cytokines such as TNF.
Since global ablation of TNF protects against progression of joint degeneration in the OA of obesity, one potential therapeutic approach is to reduce the systemic inflammation in this disease. It is now established that activation of inflammation in obesity is caused, at least in part, by alterations in the normal gut microbiome. We now have evidence suggesting that a proinflammatory shift in the obese gut microbiome is causal in the OA of obesity.
Excitingly, reversal of this shift via oral supplementation with the non-digestible prebiotic oligofructose will ameliorate systemic and joint inflammation, thereby mitigating the influence of obesity on the progression of OA. Continuing investigations are exploring the mechanistic links between the gut microbiome, inflammation, and OA progression as well as the therapeutic potential of prebiotics and probiotics as disease modifying therapies in OA.
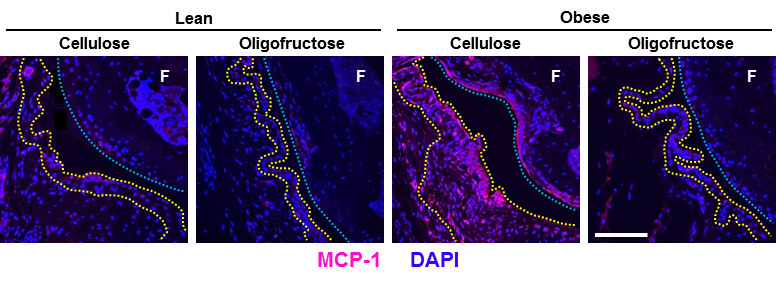
Above: Oligofructose suppresses hyperplasia and inflammation of synovial in obese mice. Tissue sections from knees of obese and lean mice treated with dietary oligofructose (prebiotic) or cellulose (control) were subjected to immunofluorescence detection of the chemokine MCP-1. Nuclei were counterstained with DAPI, yellow dotted lines outline the synovial membrane, blue dotted lines demarcate the articular cartilage surface on the femur. Note the thickened, hyperplastic synovium in the cellulose treated, obese sample.
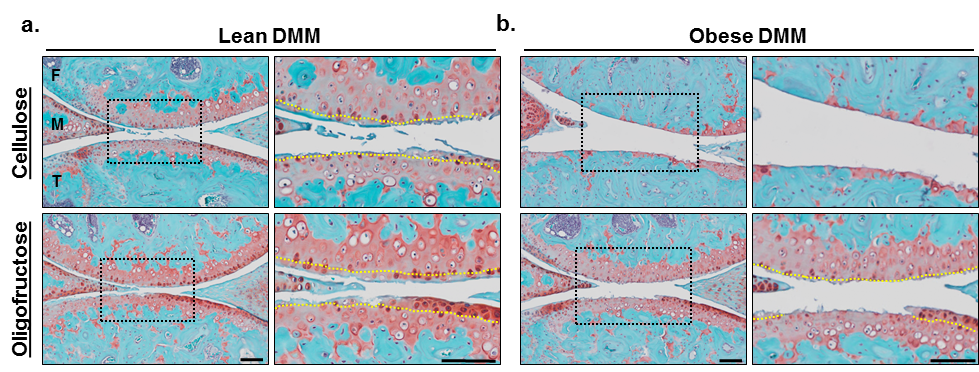
Above: Oligofructose protects against accelerated OA in obesity. Two weeks after obese mice were started on cellulose or oligofructose, an OA-initiating knee surgery was performed. Knee joints were collected 12 weeks later. Stained sections show remaining cartilage in red with bone in blue. Note the impact of oligofructose to suppress OA progression and cartilage loss.
« back to all projects