Acute Stroke Treatment
A variety of imaging techniques are used in stroke diagnosis.
CT is the prime diagnostic test performed in the emergency room. CT generates detailed pictures of the brain and can confirm the diagnosis of stroke and can tell whether the stroke was caused by hemorrhage into the brain or blockage of the artery.
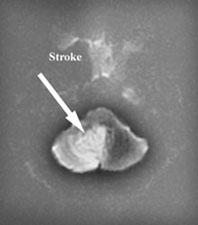
MRI or angiography are adjunct diagnostic methods. Magnetic resonance imaging can be used to create pictures of the brain and can also be used to create pictures of a blood vessel so called MR angiogram (MRA).
Ultrasound uses a technique that is called Doppler ultrasound and creates pictures using the sound waves from the blood vessels. Ultrasound can be used to determine if there is stenosis of the blood vessels in the neck.
By these techniques the doctors can pinpoint the area of stroke in the brain as well as the area of blockage of the vessels.
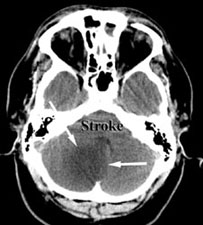
CT
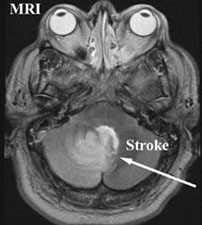
T2 MR

Flair MR
DWI
Educational Presentations
Stroke Diagnosis & Interventional Therapy