Case Diagnosis and Discussion
Diagnosis
Inflammatory myofibroblastic tumor (IMT).
Discussion
IMTs represent a myofibroblastic lesion that is benign but can be locally aggressive with recurrences and metastases reported. This spindle cell proliferation with inflammatory infiltrates are most commonly seen in the lung but can also be seen in other organ systems and include the genitourinary tract, gastrointestinal tract, abdominal cavity, and central nervous system. Laryngeal involvement by IMT is rare with 39 reported cases, typically involving the true vocal cord and occurring in patients with a mean age of 44.
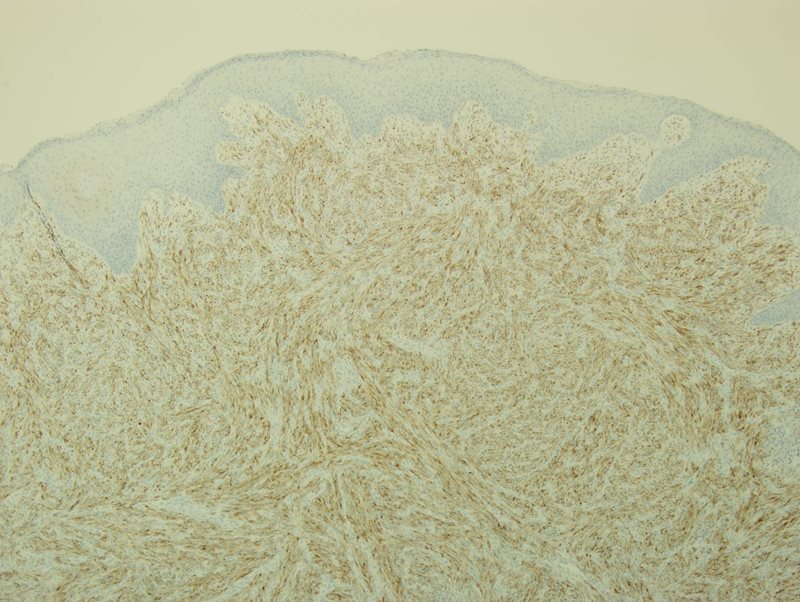
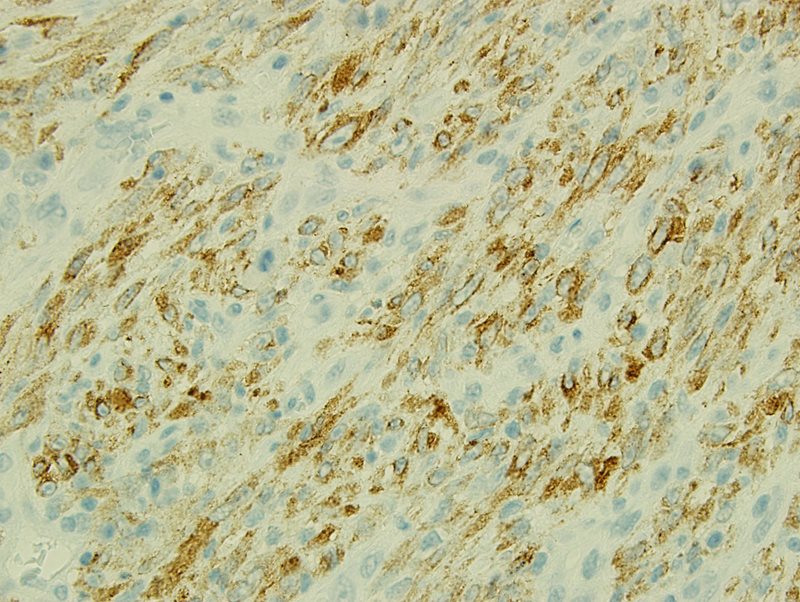
There are many postulations as to the cause of this entity including trauma, infection, smoking, and neoplasia. Most recently neoplasia has been the supported cause following identification of the anaplastic lymphoma kinase 1 (ALK1) chromosomal rearrangement involving chromosome 2p23 with multiple gene fusion partners including, TPM3, TPM4, ATIC, CLTC, CARS, RANBP2, and SEC31L1. ALK rearrangement can be identified via immunohistochemical (IHC) staining, is present in about 50% of cases, and is usually seen in younger patients. This was also present in our case (Fig 4 and Fig 5). Additional IHC stains were performed for our case and revealed the spindle cells were negative for CD34, c-kit, CD34, myogenin D, pan-cytokeratin, and EBV. Focally reactivity was also seen with smooth muscle actin (SMA).
Important differential diagnostic considerations to rule out include spindle cell squamous cell carcinoma, nodular fasciitis, and low grade myofibrosarcoma. Spindle cell squamous cell carcinomas usually show in situ carcinoma or an invasive squamous cell carcinoma element (although this may be focal), and pan-cytokeratin is usually positive. Nodular fasciitis rarely occurs in the larynx, will be ALK negative, and will not show the varied increased array of chronic inflammatory cells seen in IMT. Low grade myofibrosarcomas may be focally positive for SMA and desmin and have a destructive and infiltrative growth pattern with increased nuclear hyperchromasia and atypia usually apparent. These are also ALK negative.
Although epithelial lesions are much more common in the larynx, mesenchymal entities must be kept in mind. If there is suspicion for IMT, ALK will be helpful however this is seen in 50% of cases and thus the histologic features are paramount in conjunction with IHC.
References
Covello R, Licci S, Pichi B, Spriano G, Vidiri A, Morelli L, Rosenberg AE. Low-grade myofibroblastic sarcoma of the larynx. International journal of surgical pathology. 2011 Dec 1;19(6):822-6.
Gleason BC, Hornick JL. Inflammatory myofibroblastic tumours: where are we now?. Journal of Clinical Pathology. 2008 Apr 1;61(4):428-37.
Svrakic M, Bent JP, Adler E. Neonatal nodular fasciitis of the larynx. International journal of pediatric otorhinolaryngology. 2009 Jul 31;73(7):1007-9.
Tay SY, Balakrishnan A. Laryngeal inflammatory myofibroblastic tumor (IMT): a case report and review of the literature. Journal of Medical Case Reports. 2016 Jun 23;10(1):180.
Völker HU, Scheich M, Höller S, Ströbel P, Hagen R, Müller-Hermelink HK, Eck M. Differential diagnosis of laryngeal spindle cell carcinoma and inflammatory myofibroblastic tumor–report of two cases with similar morphology. Diagnostic pathology. 2007 Jan 9;2(1):1.
Wenig, Bruce M., Kenneth Devaney, and Michele Bisceglia. "Inflammatory myofibroblastic tumor of the larynx. A clinicopathologic study of eight cases simulating a malignant spindle cell neoplasm." Cancer 76.11 (1995): 2217-2229.