Projects
Polychromatic Adaptive Optics Visual Simulation
Adaptive Optics, a technique inherited from astronomy, allows non-invasive manipulation of the optics of the eye. In Adaptive Optics Visual Simulators we evaluate psychophysically visual function and perceived visual quality in a patient, while ocular aberrations are measured and dynamically. For example, we can make a patient see the world with the eye’s of another, and measure neural adaptation to a new visual experience. Furthermore, it is possible to map phase maps representing a visual correction (contact lens, intraocular lens, cornea treatment) onto the active elements of the simulator, and to evaluate vision non-invasively before applying the treatment or manufacturing the lens. Adaptive Optics opens therefore the possibility to explore the factors limiting human spatial vision. Furthermore, adaptive optics is a valuable technique for optical designers and clinicians to investigate the vision with new optical designs, and select the optimal treatment for a patient.
The Polychromatic Adaptive Optics Visual Simulator uses a wide range of wavelengths in the visible and infrared to characterize both the monochromatic and chromatic aberrations of the eye. A Hartmann-Shack wavefront sensor allows capturing the eye’s wave aberrations. Visual stimuli are projected Digital-Micro-Mirror which is illuminated in monochromatic light of different wavelengths or white light. Active elements in the system include an electromagnetic deformable mirror, a spatial light modulator and opto-tunable lenses.
These are some of the questions that the Marcos Lab is addressing in Polychromatic Adaptive Optics Visual Simulation: How multifocal patterns modulate accommodative response in emmetropes and myopes? What is the relative contribution of monochromatic and polychromatic aberrations to perceived image quality, visual function and accommodation?
Marcos’ review articles on Adaptive Optics visual simulators, and their applications:
- Marcos S et al. Vision science and adaptive optics, the state of the field. Vision Res. 2017 Mar;132:3-33. doi: 10.1016/j.visres.2017.01.006.
- Marcos S, et al M. VioBio lab adaptive optics: technology and applications by women vision scientists. Ophthalmic Physiol Opt. 2020 Mar;40(2):75-87. doi: 10.1111/opo.12677
- S Marcos, P Artal, D.A. Atchison, K Hampson, R Legras, L Lundström, and G Yoon, "Adaptive optics visual simulators: a review of recent optical designs and applications [Invited]," Biomed. Opt. Express 13, 6508-6532 (2022)
Funding
- NIH-National Institute of Institute R01 EY035009. Interplay between multifocal optics and accommodation: implications for myopia progression
Meta Reality Labs
Effects of multifocality on vision in presbyopia and myopia
Multifocal lenses work under the principle of simultaneous vision, producing simultaneously on the retina images at multiple foci. In presbyopic patients multifocal (intraocular or contact) lenses provide functional vision at near. Recently multifocal contact lenses have been proposed as an alternative for the control of myopia progression in non-presbyopic myopes. There is an increasing number of multifocal lenses, which can have diffractive or refractive profiles, either segmented or smooth. The through-focus retinal image quality and optical quality with multifocal contact lenses depends on the interplay between the lens optical design, the eye’s aberrations and pupil diameter, and (in young eyes) crystalline lens accommodation.
Visual simulators give the patients the experience of a multifocal correction, allowing testing perceived visual quality and visual function non-invasively through a simulated multifocal lens. Visual simulators are therefore excellent tools to investigate the visual benefit at near and visual degradation at far with different multifocal lenses, adaptation to multifocal optics, and optimizations of lens design to improve perceived vision and visual performance. In young patients, the accommodative response through multifocal lenses may be key in their efficiency for myopia control.
Binocular see-through visual simulators allow further simulations of multifocal vision in a real environment, important in both studies of accommodation in young patients (proximity cues, larger field of view) and in presbyopic patients (including monovision and modified monovision treatment options).
These are some of the questions that the Marcos Lab addresses on multifocal vision: how is visual quality and visual function affected by multifocal optics through-focus? How do patients adapt to multifocal vision? Can we improve multifocal lens designs to optimize visual quality in a focus range? Can we optimize binocular strategies in the correction of presbyopia? How do young myopes accommodate in the presence of multifocal optics? Is there an optimal multifocal lens design that prevents hyperopic blur at near?
Marcos’ sample articles on multifocal lenses and vision
- Vinas M, Aissati S, Romero M, Benedí-García C, Garzon N, Poyales F, Dorronsoro C, Marcos S. Pre-operative simulation of post-operative multifocal vision. Biomed Opt Express. 2019 Oct 21;10(11):5801-5817. doi: 10.1364/BOE.10.005801.
- Vedhakrishnan S, Vinas M, Aissati S, Marcos S. Vision with spatial light modulator simulating multifocal contact lenses in an adaptive optics system. Biomed Opt Express. 2021 Apr 21;12(5):2859-2872. doi: 10.1364/BOE.419680.
- CM Lago, A de Castro, C Benedí-García, S Aissati, S Marcos, Evaluating the effect of ocular aberrations on the simulated performance of a new refractive IOL design using adaptive optics, Biomedical Optics Express 13 (12), 6682-6694 (2022)
- S Vedhakrishnan, A de Castro, M Vinas, S Aissati, S Marcos, Accommodation through simulated multifocal optics, Biomedical Optics Express 13 (12), 6695-6710 (2022)
Funding
- NIH-National Institute of Institute R01 EY035009. Interplay between multifocal optics and accommodation: implications for myopia progression
- Center of Emerging and Innovative Sciences, State of New York Development Funds
- Clerio Vision
- Bausch and Lomb
- CooperVision
Customizing selection of intraocular lens implantation
The aged crystalline lens is replaced by an intraocular lens (IOL) in a cataract surgery. Intraocular lens designs have increased in sophistication over years, expanding the initial goal of the procedure to restore transparency into a refractive treatment. Current intraocular lenses can at least partially correct the aberration of the cornea or expand depth of focus. However, the process to select the optimal intraocular lens for patient is limited by one-dimensional biometry, keratometry and a number of implicit assumptions regarding the posterior cornea and the estimated lens position.
Fully quantitative 3-D optical coherence tomography has allowed full reconstruction of the anterior segment of the eye, including anterior and posterior corneal topography and full crystalline lens shape. Estimated Lens Position can be obtained more accurately by introducing crystalline lens parameters, and ray tracing be used on custom eye models to select the IOL that produces optimal image quality on the patient’s retina. New paradigms for IOL selection may include as well methodologies of machine learning and artificial intelligence.
These are some of the goals of Marcos Lab in the improvement of IOL selection: Introducing paradigm changes in the way IOLs are selected today; Improving refractive, optical and visual outcomes of intraocular surgery over state-of-the-art.
Recent Marcos’ review articles on intraocular lens selection
- Marcos S et al. Simulating Outcomes of Cataract Surgery: Important Advances in Ophthalmology. Annual Review of Biomedical Engineering 2021 23:1, 277-306.
- Marcos S. Improving pseudophakic optical quality beyond aspheric intraocular lenses: the next frontier. J Cataract Refract Surg. 2021 Sep 1;47(9):1111-1114. doi: 10.1097/j.jcrs.0000000000000762.
Funding
- Center of Excellence in Data Science, State of New York Development Funds
Collagen organization in cornea and sclera
The cornea and the sclera are primarily composed by collagen type I. The interweaving and arrangement of the collagen fibers highly determines tissue integrity and its material properties. Disrupted corneal collagen organization 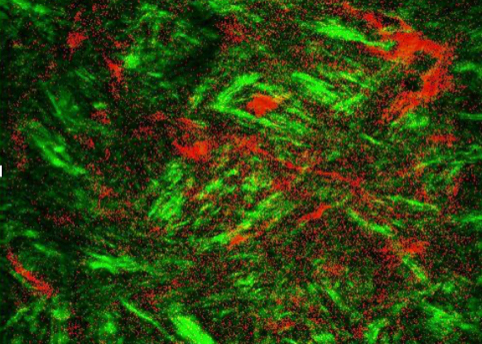 results in distorted corneal shape and decreased optical quality in disease such as keratoconus. On the other hand, development of myopia appears to be associated with reduced scleral collagen density.
results in distorted corneal shape and decreased optical quality in disease such as keratoconus. On the other hand, development of myopia appears to be associated with reduced scleral collagen density.
Corneal cross-linking (ultraviolet-riboflavin CXL or novel Green light-Rose Bengal CXL) has proved effective in stiffening the cornea and increasingly used to treat keratoconus. Likewise, cross-linking could be considered as a treatment for myopia if proved effective in stiffening the sclera, provided an available delivery to accessible scleral regions.
Assessing collagen organization is key in the understanding the underlying morphological changes in keratoconus and myopia, potential mechanisms of disease progression and the evaluation of prospective treatment strategies.
Second Harmonic generation (SHG) microscopy is a multi-photon microscopy modality that specific targets signals from non-centrosymmetric structures, in particularly collagen. SHG forward scattering (and to some extent SHG background scattering) reveals the structure and organization of collagen in cornea and sclera, and image processing techniques quantify the arrangement (using for example the collagen” order coefficient”). The order coefficient decreases from anterior to posterior cornea, shows differences between keratoconus and normal corneal tissue and changes with ex vivo and in vivo corneal cross-linking.
These are some of questions addressed in Marcos Lab regarding collagen organization assessed with Second Harmonic Generation microscopy : What is the relationship between collagen order and mechanical structure in cornea and sclera? What changes occur in collagen organization following corneal cross-linking, corneal refractive procedures and treatments targeting collagen repair? Does scleral collagen organization vary across the ocular globe? How does scleral collagen organization change during myopia development? How myopia treatments remodel the scleral tissue a microscopic scale? Towards in vivo SHG?
Some insights on the topic can be gained in these publications
- Germann JA, Martínez-Enríquez E, Marcos S. Quantization of collagen organization in the stroma with a new order coefficient. Biomed Opt Express. 2017 Dec 8;9(1):173-189. doi: 10.1364/BOE.9.000173.: PMC5772573.
- Germann JA, Martínez-Enríquez E, Martínez-García MC, Kochevar IE, Marcos S. Corneal Collagen Ordering After In Vivo Rose Bengal and Riboflavin Cross-Linking. Invest Ophthalmol Vis Sci. 2020 Mar 9;61(3):28. doi: 10.1167/iovs.61.3.28.
- Summers JA, Schaeffel F, Marcos S, Wu H, Tkatchenko AV. Functional integration of eye tissues and refractive eye development: Mechanisms and pathways. Exp Eye Res. 2021 Aug;209:108693. doi: 10.1016/j.exer.2021.108693. Epub 2021 Jul 3. PMID: 34228967.
Funding
- Center for Vision Research Pilot Funds for Vision Research Stuart Therapeutics
Optical Coherence Tomography-based ocular biometry and biomechanics
Swept source anterior segment Optical Coherence Tomography’s high spatial resolution and high acquisition rates make of it an ideal technique to quantify the geometry of the ocular structures and their dynamic properties.
Coupling sOCT image acquisition with custom-developed image processing routines for fan and optical distortion correction, automatic segmentation, novel basis functions, and quantification tools have made possible to achieve corneal and crystalline lens topographic maps and full lens shape (beyond the iris) parameters. Fully customized computer eye models to the patient’s anatomy can therefore be constructed based on 3D OCT quantitative information.
In addition, acquisition rates of 200.000 interferograms/second allow tracking dynamic changes of the crystalline lens with accommodation. It has also allowed acquisition of dynamic processes in the cornea and sclera during stimulation with an air pulse (multi-meridian air-puff corneal deformation imaging), sound (OCT vibrography) and ultrasound (Optical Coherence Elastography), which coupled with finite-element inverse analysis have allowed reconstruction of the tissue mechanical properties.
Marcos Lab is using custom-developed OCT-based technologies to tackle the following questions: What is the role of the crystalline lens in myopia development? How do myopia control contact lenses impact crystalline lens accommodation in young myopes? How lens morphology and dynamics change in presbyopia? Can we build OCT-based opto-mechanical models of the crystalline lens that capture its age-related changes? Do presbyopia treatments targeting the crystalline lens restore dynamic accommodation? What biomarkers of corneal weakening can be obtained from OCT-based technologies, and how are they related (i.e. Young’s modulus and shear modulus)? What is the relationship between tissue microstructure and mechanical properties? Is OCT viable to measure scleral mechanical properties in vivo?
A sample of three of Marcos’ articles on OCT technologies and their applications to cornea, crystalline lens or sclera:
- Muralidharan G et al Morphological changes of human crystalline lens in myopia. Biomed Opt Express. 2019 Nov 5;10(12):6084-6095. doi: 10.1364/BOE.10.006084.
- Curatolo A et al. Multi-meridian corneal imaging of air-puff induced deformation for improved detection of biomechanical abnormalities. Biomed Opt Express. 2020 Oct 14;11(11):6337-6355. doi: 10.1364/BOE.402402.
- Bronte-Ciriza D et al.. Estimation of scleral mechanical properties from air-puff optical coherence tomography. Biomed Opt Express. 2021 Sep 17;12(10):6341-6359. doi: 10.1364/BOE.437981.