Miracle Kid: Leah Upsher
Odds Were Against Baby Girl Born 17 Weeks Early
 The pattern was the same for a while: Helen Bell-Upsher, pregnant with twins, would start bleeding, go to the doctor for an ultrasound, then be sent home for bed rest after learning that her babies were fine. Eventually, though, the blood turned into blood clots, and she was admitted to a hospital near her Greece home, where her water broke at just 21 weeks along.
The pattern was the same for a while: Helen Bell-Upsher, pregnant with twins, would start bleeding, go to the doctor for an ultrasound, then be sent home for bed rest after learning that her babies were fine. Eventually, though, the blood turned into blood clots, and she was admitted to a hospital near her Greece home, where her water broke at just 21 weeks along.
The rupture caused a serious infection in Helen’s uterus, placing each baby at risk for death or, if born alive, a more complicated course of neonatal intensive care. At 23 weeks, she was transferred to Strong Memorial Hospital’s obstetrical unit. With the ongoing infection, however, one of the twins, named Avah, soon passed away.
“I felt like I couldn’t breathe,” recalled Helen, who was able to hold and kiss Avah on the forehead. “I felt like I wanted to die, but I knew I had to live for Leah. She was still there.”
Leah’s only chance for survival was an early delivery. Typically, a baby born at 23 weeks has less than a 50 percent chance for survival; in Leah’s case, her odds were even lower because of the infection, her sister’s death, and the fact that she had a low amount of fluid in the amniotic sac to help her develop lungs and breathe. Kristin M. Scheible, M.D., a neonatologist at Golisano Children’s Hospital, placed Leah’s chances of survival between 20 and 25 percent, and lower than 10 percent for survival without severe developmental problems.
Helen remembers feeling nervous and pressure in her back while being rushed to the operating room to deliver. After pushing four times, Leah was born. She weighed 1 pound, 5.5 oz., had a low heart rate, was breathing poorly, and was blue and limp. But soon, with a breathing tube and surfactant to help open her lungs, she was stabilized, brought in to see her parents, then rolled to the Neonatal Intensive Care Unit.
“I saw her legs kicking, like little chicken legs,” Helen said. “My husband said, ‘Babe, she’s OK.’”
 Lamont Upsher, who works in the environmental services department at Golisano Children’s Hospital, used work breaks to visit his daughter, who’d developed a reputation for being feisty. For Helen, who marveled over her baby’s tiny frame, it would take two visits before she was comfortable touching Leah. (“I’d never seen a baby so small. I was afraid to touch her,” she said.) The first time she lifted the incubator flap and snapped a picture with her cell phone; the second time she touched her daughter’s arm very lightly with her fingers.
Lamont Upsher, who works in the environmental services department at Golisano Children’s Hospital, used work breaks to visit his daughter, who’d developed a reputation for being feisty. For Helen, who marveled over her baby’s tiny frame, it would take two visits before she was comfortable touching Leah. (“I’d never seen a baby so small. I was afraid to touch her,” she said.) The first time she lifted the incubator flap and snapped a picture with her cell phone; the second time she touched her daughter’s arm very lightly with her fingers.
Though Leah did well her first four days – as babies born this early often do, in a phase known as the “honeymoon period” – her lungs became inflamed and she was switched from a conventional ventilator, which gives breaths 60 to 70 times per minute, to a high-frequency ventilator, allowing 700 to 900 breaths per minute. She needed stress-dose steroids, medication to raise her systemic blood pressure and open the blood vessels in her lungs, and antibiotics to treat the infection. Her kidneys started to fail, mandating the intensely careful management of her fluids and chemistry levels with intravenous support. She suffered a serious setback with a chest infection, and required surgery to fix a condition called patent ductus arteriosus, in which a blood vessel outside the heart fails to close after birth. (She did manage to avoid a major complication that often comes with such early deliveries, a catastrophic bleed inside the head known as intraventricular hemorrhage.)
Through it all, the doctors and nurses at Golisano Children’s Hospital were compassionate, calming, and able to offer hope in seemingly hopeless situations.
“There were times I’d break down and cry and ask whether I should prepare to lose another baby,” Helen said. “They would tell me it wasn’t the end of the road.”
Before Leah’s chart was reviewed or morning exams were performed each morning, Helen and Lamont faithfully reported how they felt their baby was doing, insights that were vital to Leah’s treatment plan.
“We know better than to assume that our babies are a collection of numbers and vital signs,” Scheible said. “Each patient has his or her own likes, dislikes, and physiology, which can only be appreciated by being at the bedside each day. The parents really knew her best, and we relied on their participation in her care. It was truly a team effort in getting her home.”
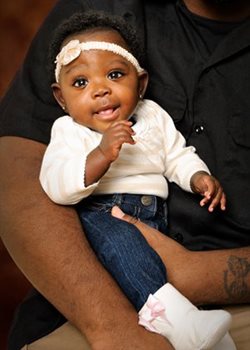
At 7 months old, Leah weighs nearly 11 pounds, is growing well both in length and weight, has been taken off medication, and loves to follow her parents around the house with her eyes. She returns to Golisano Children’s Hospital for monthly gastrointestinal checkups, and to see a developmental specialist. Hearing loss – one of the more common complications with prematurity – may be an issue, but Leah’s recovery and subsequent growth has been called truly remarkable.
Helen thanks her daughter’s caretakers at Golisano Children’s Hospital for that: “They made a way out of no way.”