Latest Neuroscience News

Feb 25, 2026
Frequently Distracted? Science Says, Blame It on Your Brain Rhythms
Frequently Distracted? Science Says, Blame It on Your Brain Rhythms

Feb 25, 2026
A Smarter Map for the Brain: Surgeons Pioneer Next-Generation Navigation
A Smarter Map for the Brain: Surgeons Pioneer Next-Generation Navigation
Feb 25, 2026
The Interstate of Science: Merging Neuroscience and AI
The Interstate of Science: Merging Neuroscience and AI

Feb 25, 2026
Student Spotlight: Lia Calcines-Rodríguez
Student Spotlight: Lia Calcines-Rodríguez

Feb 3, 2026
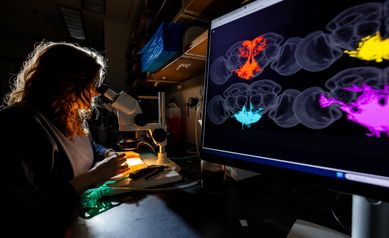
A Gallery: Neuroscientists in Color
A Gallery: Neuroscientists in Color