News
20242023202220212020
Medical Mystery: Doctor's Diagnosis Drew Laughs, But It Saved Woman's Life
Tuesday, December 7, 2010
Donna Landrigan - with her husband, Dan, and children, Kyle, left, Emma and Zach - says, "I'm so thankful to be back with my family" after surviving an illness that could have killed her. (George Bates For The Washington Post Kevin Rivoli)
As the all-too-familiar number flashed on his cellphone shortly before 9 p.m., Dan Landrigan reflexively braced himself for bad news. The caller was one of the doctors treating his wife, Donna, who had been in a coma for four months. She sounded pretty choked up,
Landrigan recalled.
I think we've found out what's making your wife sick,
the specialist at the University of Rochester's Strong Memorial Hospital told him, as a wave of relief flooded his body. I was completely shocked,
said the telecommunications executive, now 37. My hope for so long was that this was the phone call I was going to get.
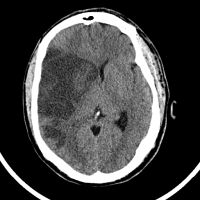
Doctors at three Upstate New York hospitals had been stymied by Donna Landrigan, whose case was unlike any they had seen. The previously healthy 35-year-old mother of three had initially become so psychotic she had to be tied to her hospital bed to keep her from hurting herself or attacking others. A few weeks later she had been placed in a medically induced coma to protect her from the continuous seizures wracking her brain, spasms that could have killed her.
Canandaigua Woman’s Ordeal Illuminates Rare Form of Seizures
Tuesday, October 19, 2010
The remarkable story of a Canandaigua, N.Y. woman who emerged from a more than six month long coma is now being used to educate physicians about how to recognize and treat her extremely rare condition. The elusive source of her uncontrolled seizures, which physicians at the University of Rochester Medical Center (URMC) ultimately traced to ovarian cancer, and her subsequent recovery are the subject of a paper appearing today in the journal Neurology.org.
Researchers Target HIV-Related Brain Difficulties
Thursday, October 7, 2010
During the last two decades, scientists and doctors have developed a potent mix of medications that nearly stops HIV in its tracks for most patients. This combination antiretroviral therapy, or cART, can knock down levels of the virus in the body to a thousandth or less of what it would otherwise be. That means more years of a healthy life for many HIV patients.
But that success does not extend fully to the brain, where an assault triggered by the virus continues despite treatment. About half of patients infected by HIV experience symptoms, such as difficulty thinking or concentrating, as a result of the effects of the virus on the brain. So far, nearly a dozen studies in people have failed to identify a drug useful for treating the condition, which is known as HIV-associated neurocognitive disorder.
At the University of Rochester Medical Center, neurologist Harris A. Handy
Gelbard, M.D., Ph.D., leads a team of scientists intent on developing the world’s first treatment designed specifically to prevent or ease the neurological effects of HIV. This week, Gelbard – whose team has spent a decade exploring novel ways to treat the condition – received word that the project would continue for another five years, thanks to $6.7 million in new funding from the National Institute of Mental Health.
Rochester Helps Lead Global Parkinson’s Study
Wednesday, October 6, 2010
Patients, doctors and nurses in Rochester will be a key part of a major national research study initiated by the Michael J. Fox Foundation to identify biomarkers to track the progression of Parkinson's disease in a precise way that is impossible to do today.
The study, known as the Parkinson's Progression Markers Initiative, seeks to fill a crucial gap: While doctors can generally predict the course that the disease takes in patients, there is no reliable, objective way to actually measure how the disease is progressing. A measure known as a biomarker, based on a biological measure that would be consistent among all patients, would help researchers measure the effectiveness of current treatments on their patients.
A reliable biomarker is also a critical tool to have in hand for scientists trying to identify new drugs to treat the disease. Currently there is no known biomarker for Parkinson's disease.
The study of approximately 600 people around the world will include up to 30 people at the University of Rochester Medical Center, which is one of 18 participating sites worldwide. The Rochester site is led by neurologist Irene Richard, M.D.
Rochester Leads International Effort To Improve Muscular Dystrophy Treatment
Friday, September 3, 2010
A large international study aimed at improving the care of muscular dystrophy patients worldwide is being launched by physicians, physical therapists, and researchers at the University of Rochester Medical Center.
Neurologist Robert “Berch” Griggs, M.D., is heading the study of treatments for Duchenne muscular dystrophy, the most common form of the disease that affects children. The condition, which affects boys almost exclusively, progresses rapidly. Boys’ symptoms start when they are toddlers; untreated, they end up in a wheelchair before they become teenagers. With today’s best treatments, the disease, which affects about 28,000 boys and young men in the United States, is often fatal by the time a patient reaches his 20s or early 30s.
Rochester’s Pinpoint Gene Control Boosts Parkinson’s Research
Tuesday, August 24, 2010
Top: The dark area shows a part of the mouse brain where dopamine neurons have died when toxic LRRK2 is active. Below: Dopamine neurons (in red) thrive when toxic gene activity is blocked.
A technology developed at the University of Rochester Medical Center that enables scientists to turn on genes exactly when and where they want in the nervous system is helping scientists in the hunt for an agent to stop Parkinson's disease.
The work employs the herpes virus – the bane of so many people, but in this instance an aid to researchers – to help mimic in mice the activity of a gene that plays a role in some cases of Parkinson's disease in people. Scientists used the virus to carry a copy of the faulty gene into mice, creating brain conditions identical to Parkinson's disease. The step allowed researchers to then screen compounds in the search for one that might stop the toxicity of the gene.
The team of scientists, led by investigators at Johns Hopkins University, found two promising candidates and reported its results August 22 in Nature Medicine.
“While there are many drugs to treat symptoms of Parkinson's disease, there is currently no drug available to stop the death of nerve cells that is at the core of the disease,” said neuroscientist William Bowers, Ph.D., of the University of Rochester Medical Center. “This study identifies a few viable candidates that show promise against one form of the disease.”
Scientists Pinpoint Earliest Steps of Common Form of Muscular Dystrophy
Thursday, August 19, 2010
Nearly two decades after they identified the specific genetic flaw that causes a common type of muscular dystrophy, scientists believe they have figured out how that flaw brings about the disease. The finding by an international team of researchers, including scientists at the University of Rochester Medical Center, settles a longstanding question about the roots of facioscapulohumeral muscular dystrophy or FSHD. The work was published online August 19 in the journal Science Mag.
Unraveling how the genetic defect causes FSHD has been especially challenging for scientists. Unlike with many genetic diseases, their identification of the mutation that is the basis of FSHD did not quickly lead to a deeper understanding of how the disease actually comes about. The lack of clarity has posed a significant barrier to researchers hoping to turn the knowledge of the genetic flaw into significant progress for patients.
Acupuncture’s Molecular Effects Pinned Down
Sunday, May 30, 2010
Scientists have taken another important step toward understanding just how sticking needles into the body can ease pain.
In a paper published online May 30 in Nature Neuroscience, a team at the University of Rochester Medical Center identifies the molecule adenosine as a central player in parlaying some of the effects of acupuncture in the body. Building on that knowledge, scientists were able to triple the beneficial effects of acupuncture in mice by adding a medication approved to treat leukemia in people.
The new findings add to the scientific heft underlying acupuncture, said neuroscientist Maiken Nedergaard, M.D., D.M.Sc., who led the research. Her team is presenting the work this week at a scientific meeting, Purines 2010, in Barcelona, Spain.
URMC’s First Chief of Child Neurology Dies
Monday, May 24, 2010
Frederick A. Horner, M.D., the first chief of Child Neurology at the University of Rochester School of Medicine and Dentistry, died April 20, 2010, at the age of 90.
Dr. Horner graduated in 1947 from the University of Rochester School of Medicine and Dentistry and went on to complete a pediatric internship and an assistant residency here at Strong Memorial Hospital. After specialty training elsewhere, he joined the faculty in 1968 to become the first chief of Child Neurology at the University of Rochester.
Dr. Horner is survived by his wife, Marjorie; sister, Kathryn Altmas; brother, David Horner; nieces and nephews. Services will be private. Contributions in memory of Dr. Horner may be made to the Dr. Frederick A. Horner Social Work Emergency Fund, University of Rochester, P.O. Box 270032, Rochester, NY 14627.
URMC Named Batten Disease Center of Excellence
Wednesday, May 12, 2010
The largest Batten Disease research and support organization in North America named the University of Rochester Medical Center as a Batten Disease Center of Excellence today. The Ohio-based organization, Batten Disease Support and Research Association, has chosen URMC because of its comprehensive services for patients and its long clinical and research history with the disease.
Batten Disease is a rare neurodegenerative syndrome that erupts with little warning. It first steals sight, then cripples cognitive and motor capacities, and while different variations of the disease brings a difference age of onset and progression, it is, ultimately, terminal. The most common form is juvenile, in which symptoms begin between 5 and 8 years of age. There are between 500 and 1,000 people with Batten Disease in the United States and only a few thousand in the world.
"Finding treatment with a comprehensive team that has experience with the disease is incredibly hard for families," said Jonathan Mink, M.D., Ph.D., chief of Child Neurology and professor of Neurology, Neurobiology & Anatomy and Pediatrics at URMC. "The Batten Disease Support and Research Association is hoping to streamline families' search for expertise by endorsing centers like ours."
URMC Named Batten Disease Center of Excellence by BDSRA
Wednesday, May 12, 2010
Lance Johnston, Executive Director of the BDSRA, awarding Dr. Jonathan Mink with the Batten Disease Center of Excellence plaque.
The largest Batten Disease research and support organization in North America named the University of Rochester Medical Center (URMC) as a Batten Disease Center of Excellence today. The Ohio-based organization, Batten Disease Support and Research Association, has chosen URMC because of its comprehensive services for patients and its long clinical and research history with the disease.
Batten Disease is a rare neurodegenerative syndrome that erupts with little warning. It first steals sight, then cripples cognitive and motor capacities, and while different variations of the disease brings a difference age of onset and progression, it is, ultimately, terminal. The most common form is juvenile, in which symptoms begin between 5 and 8 years of age. There are between 500 and 1,000 people with Batten Disease in the United States and only a few thousand in the world.
Finding treatment with a comprehensive team that has experience with the disease is incredibly hard for families,
said Jonathan Mink, M.D., Ph.D., chief of Child Neurology and professor of Neurology, Neurobiology & Anatomy and Pediatrics at URMC. The Batten Disease Support and Research Association is hoping to streamline families’ search for expertise by endorsing centers like ours.
Variations in Decisions for Care of Patients with Brain Injury “Disturbing”
Wednesday, May 12, 2010
Treatment decisions involving patients with severe brain injury vary widely between medical institutions, and appear to be more driven by hospital and physician practices and priorities. In an article appearing today in the New England Journal of Medicine, physicians at the University of Rochester Medical Center argue that providers must take steps to develop a process of communication and decision-making that gives greater weight and voice to the informed preferences of patients and their families.
"The decision whether or not to continue aggressive medical treatment for patients with severe brain injury requires tough discussions about the benefits and burdens," said URMC neurologist Robert Holloway, M.D., co-author of the article. "Such decisions are often made without a clear understanding of the patient's medical prognosis and with suboptimal input from the patient and family. The possibility that decisions of this magnitude are being overly influenced by factors other than patient values and preferences informed by an understanding of the medical options and potential outcomes should make us cringe."
Heart Drug Effective for Treating Symptom of Muscular Dystrophy
Tuesday, May 4, 2010
A medication most often used to treat heart arrhythmias also reduces a central symptom of myotonic dystrophy, the most common type of muscular dystrophy in adults. The findings about the medication mexiletine -- a chemical cousin of lidocaine -- were published May 4 in the journal Neurology, a publication of the American Academy of Neurology.
Currently there is no drug approved to treat myotonic dystrophy, an inherited disease that is marked by progressive muscle weakness. While the course of the disease can vary dramatically from patient to patient, symptoms besides weakness can include muscle stiffness, difficulty speaking and swallowing, problems walking, and in some patients, heart problems and cataracts. Physicians estimate that approximately 40,000 Americans have the condition.
URMC Receives $4.5 Million in NYS Stem Cell Grants
Thursday, March 25, 2010
The University of Rochester Medical Center (URMC) has received a total of $4.5 million in funding from the Empire State Stem Cell Board for research in neurological disease, cancer, cardiovascular disease, and bone repair.
“Stem cell and regenerative medicine represents one of the scientific foundations of the Medical Center’s strategic plan for growth in biomedical research,” said Bradford C. Berk, M.D., Ph.D., CEO of URMC. “These grants represent critical resources necessary to advance our understanding of stem cells and bring these discoveries into new therapies for a host of diseases.”
Berk is also a member of Funding Committee of the Empire State Stem Cell Board.
The awards to URMC were part of $34.7 million in grants recently announced by Governor David Paterson. To date, URMC scientists have received $8.1 million in research grants from the Empire State Stem Cell Board.
Hickok Center for Brain Injury hosts Epilepsy Panel
Wednesday, March 17, 2010
The Hickok Center for Brain Injury hosts a free Brown Bag Educational Panel entitled “The Brain – Living With Epilepsy” on Monday, March 29, 2010 at their Rochester Center located at 114 South Union Street, Rochester, NY 14607 from 11:30 a.m. - 1 p.m.
The panel will feature: J. Craig Henry, MD, Assistant Professor of Neurology, Strong Epilepsy Center; A. James Fessler, III, MD, Assistant Professor of Neurology at University of Rochester and Director of Clinical Research and Assistant Director, Strong Epilepsy Center; and Michael Radell, Community Educator & Camp EAGR Director, Epilepsy Foundation of Rochester-Syracuse-Binghamton.
This is the first of four brown bag educational events the Hickok Center will host throughout 2010. Bring your lunch and learn about the medical and social issues of living with epilepsy. If you or someone you love has epilepsy, here is an opportunity to learn and ask questions of area professionals. Lot and street parking available.
Reservations strongly suggested as seating is limited. To make a reservation, please call (585) 271-8640 x207 or email ghewson@hickokcenter.org to reserve a seat.
New Center to Focus on Early Stage Clinical Research
Tuesday, March 2, 2010
A new initiative at the University of Rochester Medical Center will provide academic and industry researchers the expertise and scientific collaboration necessary to conduct early stage clinical studies. The Center for Human Experimental Therapeutics (CHET) represents the first university-based program focused on accelerating the development of novel medical therapies.
This Center consists of both infrastructure and a group of people with decades of combined experience in conducting experimental human therapeutics and running some of the more complex clinical studies in the world,
said URMC neurologist Karl Kieburtz, M.D., director of CHET. It is a unique approach that represents a marriage of scientific expertise and logistical competence, with a focus on the early stage of drug development.
Drug Shows Promise for Huntington’s Disease
Monday, February 8, 2010
An early stage clinical trial of the experimental drug dimebon (latrepirdine) in people with Huntington's disease appears to be safe and may improve cognition. That is the conclusion of a study published today in the Archives of Neurology.
This is the first clinical trial that has focused on what is perhaps the most disabling aspect of the disease,
said University of Rochester Medical Center neurologist Karl Kieburtz, M.D., the lead author of the study. While more investigation needs to be done, these results are encouraging and show, for the first time, a statistically significant benefit in terms of improved cognitive function in patients with Huntington's disease.
Huntington's disease is a progressive neurodegenerative disorder that impacts movement, behavior, cognition, and generally results in death within 20 years of the disease's onset. The disease steadily erodes a person's memory and their ability to think and learn. Over time, this cognitive impairment contributes to the loss of the ability to work and perform the activities of daily life. There are no treatments currently available that effectively alter the course of the disease or improve cognition.
New Multiple Sclerosis Drug has URMC Ties
Friday, January 22, 2010
The Food and Drug Administration has approved the drug fampridine-SR for the treatment of multiple sclerosis. Researchers at the University of Rochester Medical Center (URMC) have been evaluating the effects of the drug in MS for more than 10 years– it is the first medication shown to enhance some neurological functions in people with the disease – and their efforts helped pave the way for today’s action by the FDA.
“This is a good day for people who suffer from multiple sclerosis,” said Andrew Goodman, M.D., chief of the URMC Multiple Sclerosis Center. “Physicians will now have a new tool at their disposal that complements existing disease modifying therapies. For some patients, this drug will be a way to improve walking and help regain some independence in their daily lives.”
Study: Era of Rapid Growth in Biomedical Research Over
Tuesday, January 12, 2010
After a decade of remarkable growth, total annual funding for biomedical research in the U.S. has decelerated and may have even fallen when adjusted for inflation. That is the conclusion of a study today published in the Journal of the American Medical Association.
"The era of rapid expansion in biomedical research funding that began in the 1990's has ended," said Ray Dorsey, M.D., a neurologist at the University of Rochester Medical Center and lead author of the study. "Looking back at this period, one of the striking observations is that while research funding increased, the number of novel treatments entering the market remained steady. If research funding levels are to return to a phase of growth, we should examine funding priorities, particularly in health services research, and barriers to the development of new therapies."
Impact of FDA Safety Warnings Examined
Monday, January 11, 2010
A study published today in the Archives of Internal Medicine examines the impact of a safety warning issued by the Food and Drug Administration for commonly prescribed antipsychotic medications. The results show the warnings resulted in a decline in usage among the elderly with dementia, yet raise the question as to whether the FDA's system of communicating these warnings is sufficiently targeted and effective.
"Because this medication class has limited evidence of benefit among the elderly with dementia and significantly increases their risk of death, the 'right' magnitude of decline in usage is not clear," said University of Rochester Medical Center neurologist Ray Dorsey, M.D., the study's lead author. "More generally, the study raises larger issues about appropriate prescribing, particularly among the elderly, and the need to improve risk communication to patients and providers."
Rochester Neurologist Takes a Lead Role Tackling Charcot-Marie-Tooth
Thursday, December 31, 2009
A Meissner corpuscle, a tiny structure in the skin that allows us to feel light touch. David Herrmann monitors these structures to gauge the extent of a patient's neuropathy.
Neurologist David Herrmann, MBBCh, associate professor of Neurology and of Pathology and Laboratory Medicine at the University of Rochester Medical Center, is taking part in a newly funded nationwide study focusing on a condition known as Charcot-Marie-Tooth disease, a painful nerve condition that affects more than 100,000 Americans.
Herrmann, director of the Peripheral Neuropathy Clinic at Strong Memorial Hospital, is part of a team that has been awarded $6.25 million from the National Institutes of Health. The project is based at Wayne State University in Detroit and includes Herrmann and other collaborators from around the world.
The new funding, part of NIH's Rare Diseases Clinical Research Network, will support the Inherited Neuropathies Consortium for the next five years.
UR Study Reveals Chemo’s Toxicity to Brain, Possible Treatment
Thursday, December 17, 2009
Researchers have developed a novel animal model showing that four commonly used chemotherapy drugs disrupt the birth of new brain cells, and that the condition could be partially reversed with the growth factor IGF-1.
Published early online in the journal Cancer Investigation, the University of Rochester Medical Center study is relevant to the legions of cancer survivors who experience a frustrating decline in cognitive function after chemotherapy treatment, known as chemo brain.
"It is not yet clear how our results can be generally applied to humans but we have taken a very significant step toward reproducing a debilitating condition and finding ways to treat it," said Robert Gross, M.D., Ph.D., professor of Neurology and of Pharmacology and Physiology at URMC and principal investigator of the study.
Rochester Physician Named Editor of Leading Neurology Journal
Thursday, November 5, 2009
A neurologist and epilepsy expert at the University of Rochester Medical Center has been named editor in chief of one of the world's leading journals devoted to issues involving the brain and central nervous system.
Robert A. Gross M.D., Ph.D., professor of Neurology and of Pharmacology and Physiology, was named today to lead the medical journal Neurology, the world's leading clinical neurology journal. As editor, Gross assumes a major leadership role in the world of neurology, helping set the direction and focus for the discipline worldwide. He will contribute to decisions about which issues are of most importance to physicians and patients, and which new findings and new research avenues are most worthy of attention.
Gross has been involved with the journal for 20 years, first as a reviewer, then associate editor for the past eight years. During the last two he has also been deputy editor and most recently served as interim editor in chief.
Gross succeeds another Rochester neurologist, Professor Robert Griggs, M.D., who is now president of the American Academy of Neurology, an association of more than 21,000 neurologists and neuroscience professionals that publishes Neurology. Griggs himself served as the editor of the journal from 1997 to 2007.
Cost Effectiveness of Blood Pressure Device Evaluated
Thursday, October 15, 2009
A study conducted by the University of Rochester Medical Center demonstrates that, for certain patient populations, an experimental device that lowers blood pressure may be a cost effective treatment. The implantable device, called Rheos, is in advanced stages of testing for individuals with drug resistant hypertension.
The study – which appears this month in the Journal of Clinical Hypertension – used data from two large population-based studies and compared the incidence of adverse health events such as stroke and heart attack for groups of individuals with and without the blood pressure lowering benefit of the device. Researchers then projected the health care costs associated with those events over a patient’s lifetime. The results show that if Rheos continues to perform at a level consistent the initial findings in ongoing clinical trials, then the device is a cost effective way to control hypertension.
Our goal was to determine whether or not the benefit of Rheos would offset the higher upfront costs,
said Kate C. Young, Ph.D., MPH, an instructor in the departments of Surgery and Neurology at URMC and lead author of the study. What we found is that the device’s cost effectiveness is dependent upon the degree to which it can reduce blood pressure and the starting point of the patient.
Rochester-Led Parkinson’s Study Pays Off Again, Two Decades Later
Monday, October 12, 2009
Parkinson’s disease progresses more slowly in patients who have higher levels of urate, a chemical that at very high level is associated with gout, scientists have found. While it’s unknown whether the high levels actually somehow protect patients or simply serve as a marker of protection, the finding supports the idea that patients and doctors may one day be able to better predict the course of the illness.
The study, led by scientists at Massachusetts General Hospital and the Harvard School of Public Health and including physicians at the University of Rochester Medical Center, was published online in the Archives of Neurology.
Emmy Awarded to ABC News Primetime
Story Featuring Jonathan Mink, M.D., Ph.D.
Tuesday, September 29, 2009
ABC News was recognized with an Emmy Award from the National Academy of Television Arts and Sciences for a Primetime
story featuring URMC pediatric neurologist Jonathan Mink, M.D., Ph.D. Dr. Mink, a professor of Neurology, Neurobiology & Anatomy, Pediatrics, and Brain & Cognitive Sciences, focuses his research on the function of the basal ganglia in normal control of movement and the pathophysiology of basal ganglia disorders characterized by abnormal involuntary movements.
Genetic Source of Muscular Dystrophy Neutralized
Thursday, July 16, 2009
Researchers at the University of Rochester Medical Center have found a way to block the genetic flaw at the heart of a common form of muscular dystrophy. The results of the study, which were published today in the journal Science, could pave the way for new therapies that essentially reverse the symptoms of the disease.
The researchers used a synthetic molecule to break up deposits of toxic genetic material and re-establish the cellular activity that is disrupted by the disease. Because scientists believe that potentially all of the symptoms of myotonic dystrophy – the most common form of muscular dystrophy in adults – flow from this single genetic flaw, neutralizing it could potentially restore muscle function in people with the disease.
This study establishes a proof of concept that could be followed to develop a successful treatment for myotonic dystrophy,
said URMC neurologist Charles Thornton, M.D., the senior author of the study and co-director of the URMC Wellstone Muscular Dystrophy Cooperative Research Center. It also demonstrates the potential to reverse established symptoms of the disease after they have developed, as opposed to simply preventing them from getting worse.
Study in Nature: MicroRNAs Hold Promise For Treating Diseases in Blood Vessels
Sunday, July 5, 2009
The pictured microRNA molecule (green) may prevent the thickening of blood vessels walls that leads to clogged vessels and heart attacks.
A newly discovered mechanism controls whether muscle cells in blood vessels hasten the development of both atherosclerosis and Alzheimer's disease, according to an article published online today in the journal Nature.
The study was led by the Gladstone Institute of Cardiovascular Disease in San Francisco, with key contributions from the Aab Cardiovascular Research Institute at the University of Rochester School of Medicine and Dentistry.
Thanks to stem cells, humans develop from a single cell embryo into a complex being with about 250 unique cell types. As the fetus develops, cells divide and multiply (proliferate) in many generations and specialize (differentiate) with each generation until millions of functional cells result (bone, nerve, blood, skin, muscle, etc.). To serve specific roles in the body, some stem cells also switch back and forth between primitive, rapidly proliferating precursors and their mature, functioning, non-proliferating counterparts, a quality called plasticity.
Telemedicine Expands Reach of Care for Parkinson’s Patients
Wednesday, June 17, 2009
A unique and innovative telemedicine project is providing distant nursing home patients with Parkinson's disease access to neurologists at the University of Rochester Medical Center. A pilot study of the project -- the results of which were released this month at the International Congress of Parkinson's Disease and Movement Disorders in Paris -- demonstrates that the system can improve the quality of life and motor function of patients.
This study shows that we can effectively deliver care for Parkinson's patients via telemedicine,
said URMC neurologist Ray Dorsey, M.D. This system enables us to reach and provide a high level of care to patients who might otherwise not have access to a specialist.
Dorsey and his colleague Kevin Biglan, M.D. oversee the project and divide patient responsibilities between them. The effort is a joint initiative between URMC and the Presbyterian Home for Central New York in New Harford, a 250 bed nursing home near Utica and about 150 miles from Rochester.
Protein Regulates Movement of Mitochondria in Brain Cells
Monday, June 15, 2009
Scientists have identified a protein in the brain that plays a key role in the function of mitochondria – the part of the cell that supplies energy, supports cellular activity, and potentially wards off threats from disease. The discovery, which was reported today in the Journal of Cell Biology, may shed new light on how the brain recovers from stroke.
Understanding the molecular machinery that helps distribute mitochondria to different parts of the cell has only recently begun to be understood,
said University of Rochester Medical Center neurologist David Rempe, M.D., Ph.D., the lead author of the study. We know that in some disease states that mitochondria function is modified, so understanding how their activity is modulated is important to understanding how the brain responds to a pathological state.
Brain Protein Central to Both Parkinson’s, Drug Addiction Identified
Thursday, April 30, 2009
Scientists have identified a protein that appears not only to be central to the process that causes Parkinson’s disease but could also play a role in muting the high from methamphetamine and other addictive drugs.
The action of the protein, known as organic cation transporter 3 or oct3, fills a longstanding gap in scientists’ understanding of the brain damage that causes symptoms like tremor, stiffness, slowness of movement and postural instability. While these are found mainly in patients with Parkinson’s disease, there are more than three dozen other known causes of this array of symptoms, known as parkinsonism.
In a paper published online this week in the Proceedings of the National Academy of Sciences, scientists at the University of Rochester Medical Center and Columbia University have shown that oct3, a protein that shepherds molecules into and out of cells, plays a critical role, bringing toxic chemicals to the doorstep of the brain cells that die in patients with Parkinson’s disease. The team found that oct3 is involved in the brain’s response to addictive drugs like methamphetamine as well.
URMC Physician Elected President of American Academy of Neurology
Thursday, April 30, 2009
University of Rochester Medical Center neurologist Robert C. Griggs, M.D. has been elected president of the American Academy of Neurology (AAN), the world’s largest professional organization of neurologists.
Griggs, who was elected at the AAN’s annual meeting this week in Seattle, will lead an organization that was established 1948 and consists of more than 21,000 neurologists and neuroscience professionals. Griggs has also served as chair of the AAN Education Committee and editor-in-chief of the Academy’s prestigious scientific journal Neurology for 10 years.
Dr. Griggs is a visionary and has made extraordinary contributions to the field of neurology,
said Catherine M. Rydell, executive director and CEO of the AAN. His decades of leadership with the Academy and the respect of his peers position him well to lead the organization. The AAN relies on outstanding continued leadership as we look ahead toward furthering research and treatments for the neurology patient and professional.
Neurologists Establish Professorship in Honor of Robert J. Joynt
Wednesday, April 29, 2009
Colleagues and friends in the Department of Neurology at the University of Rochester Medical Center are more than halfway toward their goal of raising $1.5 million to honor the physician who founded the department.
The professorship will honor neurologist Robert J. Joynt, M.D., Ph.D., one of the most influential neurologists of the last half century, who is now Distinguished University Professor at the University of Rochester Medical Center. Joynt founded the University’s Department of Neurology in 1966 and guided the department for 18 years, laying the foundation for what is today one of the nation’s leading neurology departments.
The professorship, to be known as the Robert J. Joynt Chair in Experimental Therapeutics in Neurology, is designed to further development of treatments to treat neurological diseases. The Joynt Chair will support research to treat disorders like Parkinson’s, Huntington’s, and Alzheimer’s diseases. Friends, alumni, colleagues and grateful patients have contributed to the fund thus far.
Poor Sleep Quality Leads to Poorer Prognosis after Stroke
Tuesday, April 28, 2009
Stroke victims tend to do worse if they also have diagnosed or undiagnosed obstructive sleep apnea prior to having the stroke, according to a study presented April 28, 2009, at the American Academy of Neurology (AAN) annual meeting in Seattle.
Latha Stead, M.D., professor and chair of the Department of Emergency Medicine at the University of Rochester Medical Center, and professor of Neurosurgery, reported the findings at AAN, along with several other stroke studies measuring the factors that lead to a poor prognosis.
We know that obstructive sleep apnea has been linked to a multitude of cardiovascular problems, yet it is concerning that the vast majority of cases remain undiagnosed,
Stead said. In the context of recovering from a stroke, sleep apnea can have a serious impact, and for that reason we encourage people to become more aware of obstructive sleep apnea and to get treatment.
3 Events Offer Hope for People with Brain Tumors
Thursday, April 16, 2009
A PET scan allows doctors to see a brain tumor in an elderly man.
People with brain tumors, and those who love and care for them, will observe Brain Tumor Awareness Week with three educational and celebratory events sponsored by the University of Rochester Medical Center and James P. Wilmot Cancer Center.
On Friday, May 1, there will be a seminar for patients, their families, and physicians that focuses on the latest research and treatment approaches in brain and spinal tumors. Then on Thursday, May 7, patients, families and clinicians will gather for the Community Sharing Hope Picnic at Kings Bend Park in Pittsford. And on Saturday, May 9, there will be an education and supportive program for caregivers.
Each year, approximately 500 people with brain tumors are treated at the Medical Center and Wilmot Cancer Center, making it the largest program in the region. The events are offered by the Program for Brain and Spinal Tumors at the Medical Center and the Wilmot Cancer Center.
Rochester Scientist Wins Major Award for Alzheimer’s Research
Wednesday, April 15, 2009
A Rochester researcher whose work has opened up a whole new avenue in Alzheimer’s disease research has received a major prize from the American Academy of Neurology.
Berislav Zlokovic, M.D., Ph.D., director of the Center for Neurodegenerative and Vascular Brain Disorders at the University of Rochester Medical Center, will receive the 2009 Potamkin Prize for Research in Pick’s, Alzheimer's, and Related Diseases during the AAN annual meeting later this month in Seattle.
Zlokovic will split the $100,000 prize with two other researchers, Michael Wolfe, Ph.D., of Brigham and Women’s Hospital and Harvard Medical School, and Robert Vassar, Ph.D., of Feinberg School of Medicine at Northwestern University. The prize, which honors researchers for their work on Alzheimer’s disease and related disorders, will go toward the investigators’ Alzheimer’s research.
Oxycodone Effective Against Shingles Pain
Wednesday, March 25, 2009
The painkiller oxycodone is effective at treating the acute pain of shingles, an illness that often causes severe pain which can become long-lasting and sometimes even permanent.
The study, published in the April issue of the journal Pain, is one of the first to carefully evaluate different methods to relieve pain during a course of shingles, which many patients say causes the worst pain they have ever experienced. Effective pain treatment is crucial. Not only can the pain of shingles disrupt people’s quality of life, but it is also possible that the less effectively the pain is treated, the more likely it will become a long-term problem that can change a person’s life forever.
Abnormal EKG Can Predict Death in Stroke Patients
Friday, March 20, 2009
People who suffer an ischemic stroke and also have an abnormality in the heart’s electrical cycle are at a higher risk of death within 90 days than people who do not have abnormal electrical activity at the time of emergency treatment, according to new research.
The study also provides a threshold at which the threat of death is highest: QTc intervals greater than 440 milliseconds in women and 438 milliseconds in men have the worst prognosis. The findings are published online March 20, 2009, in the Journal of Stroke and Cerebrovascular Diseases.
Weighing the Options after Life-Altering Stroke
Thursday, March 12, 2009
Choosing to have aggressive brain surgery after suffering a severe stroke generally improves the patients' lives and allows them to live longer, according to research by neurologists at the University of Rochester Medical Center.
The findings should help patients and families put into perspective a decision that is nearly always painful and difficult to make – whether putting a patient through aggressive surgery after a catastrophic stroke is worth it.
For families facing this difficult choice, the more information we can provide, the better for their decision-making,
said neurologist Adam G. Kelly, M.D., who has helped hundreds of families chart a course after severe stroke. Kelly presented the findings last month at the International Stroke Conference in San Diego.
Long-Term Effects of Early Parkinson’s Treatments Similar
Tuesday, March 10, 2009
A study published online today in the Archives of Neurology involving two common drugs used to treat early-stage Parkinson's disease shows that, while the drugs each have advantages and disadvantages, the overall impact tends to even out over a long period of treatment.
Clinicians and patients often struggle with what is the right initial approach to treating Parkinson's disease,
said University of Rochester Medical Center neurologist Kevin Biglan, M.D., M.P.H., the lead author of the paper and a member of the Parkinson's Study Group, an international network of researchers that oversaw the clinical trial. This study tells us that, over the long haul, patients on the different drugs end up at roughly the same place in terms of their level of disability and quality of life.
Event to Benefit Those Affected by Neuromuscular Disorders
Monday, February 16, 2009
An arts and crafts show to be held in Batavia later this month will benefit patients and their families who have been affected by neuromuscular disorders like neuropathy, muscular dystrophy, and amyotrophic lateral sclerosis (Lou Gehrig’s disease).
The show will be from 9 a.m. to 5 p.m. Saturday, Feb. 28, at the Batavia Holiday Inn at 8250 Park Road, immediately off Thruway Exit 48. Admission is free.
Tingling Hands, Burning Feet? Rochester Neurologist an Expert in Tracking Down Neuropathy
Monday, January 5, 2009
Hands that feel like they're burning; feet that make it feel like you're walking on pins and needles; numbness that spreads gradually up the limbs. These are among the most vexing of symptoms for patients and their doctors alike. Many patients spend years going from doctor to doctor seeking a diagnosis, and many doctors order test upon test, with no firm conclusion.
Now a Rochester neurologist has helped compile a national set of guidelines that aim to help doctors better diagnose the most common cause of such symptoms more quickly and efficiently and with less expense.
David Herrmann, MBBCh, director of the Peripheral Neuropathy Clinic at Strong Memorial Hospital, is an author of the guidelines for a painful nerve condition known as neuropathy, which affects millions of people with diabetes and many other patients as well. The new practice parameters were published last month in the journal Neurology.
Two Cardiovascular Proteins Pose a Double Whammy in Alzheimer's
Sunday, December 21, 2008
Amyloid is visible as white around the blood vessels in the brain of a mouse with a condition like Alzheimer's.
Researchers have found that two proteins which work in tandem in the brain's blood vessels present a double whammy in Alzheimer's disease. Not only do the proteins lessen blood flow in the brain, but they also reduce the rate at which the brain is able to remove amyloid beta, the protein that builds up in toxic quantities in the brains of patients with the disease.
The work, described in a paper published online Dec. 21 in the journal Nature Cell Biology, provides hard evidence directly linking two processes thought to be at play in Alzheimer's disease: reduction in blood flow and the buildup of toxic amyloid beta. The research makes the interaction between the two proteins a seductive target for researchers seeking to address both issues.
Scientists were surprised at the finding, which puts two proteins known for their role in the cardiovascular system front and center in the development of Alzheimer's disease.
This is quite unexpected,
said Berislav Zlokovic, M.D., Ph.D., a neuroscientist and a senior author of the study. On the other hand, both of these processes are mediated by the smooth muscle cells along blood vessel walls, and we know that those are seriously compromised in patients with Alzheimer's disease, so perhaps we shouldn't be completely surprised.
Breaking the Silence After a Study Ends
Monday, December 8, 2008
While an estimated 2.3 million people in the U.S. take part in clinical trials every year, there currently exists no formal requirement to inform them of study results; an oversight that leaves participants confused, frustrated, and, in some cases, lacking information that may be important to their health. In an article published today in the Archives of Neurology, researchers at the University of Rochester Medical Center have proposed a novel and effective approach to disseminate the results of clinical trials to study volunteers.
Industry, government, and academic researchers are dependent upon the willing participation of millions of individuals to fill the estimated 50,000 clinical trials conducted every year that evaluate the safety and efficacy of experimental drugs and medical devices.
Researchers are only required to inform participants in instances when new information arises that may affect their willingness to continue participation. However, neither federal guidelines nor institutional review boards generally require disclosure of results at the conclusion of a study -- even if the study is halted. Consequently, many research participants never learn the outcome of studies in which they volunteer.
Individuals who volunteer to participate in clinical research frequently expose themselves to risks, both known and unknown,
said URMC neurologist Ray Dorsey, M.D., the report's author. Because of their participation, they should be informed of the results of these studies in a timely and personalized manner.
URMC Leads Study for New Treatment for Tourette’s
Tuesday, December 2, 2008
The University of Rochester Medical Center is leading a multi-center clinical research study of a new experimental treatment for Tourette’s syndrome. The study will examine whether or not a drug that alters the chemical activity in the brain can alleviate the symptoms of the disease.
Tourette’s syndrome (TS) is a neurological disorder characterized by multiple, repeated tics. These tics generally consist of abrupt and involuntary vocal outbursts or muscular jerks. Symptoms usually begin at an early age and can increase in frequency and severity over time. Many individuals with TS have a mild form of the disease and do not require medical intervention unless the tics interfere with normal daily function. Patients with more severe forms of TS are currently treated with various antipsychotic drugs.
While the precise mechanism that causes Tourette’s is unknown, we have long observed that the neuro-chemical dopamine is overly active in individuals with the disease,
said URMC neurologist Roger Kurlan, M.D., the study’s principal investigator. This chemical imbalance in the brain may play a role in the disease and, consequently, the drugs that are currently used to treat the disease are known to suppress dopamine production. However, these drugs are also associated with severe side effects that often deter their use.
Scientists Exploring New Compounds to Target Muscular Dystrophy
Wednesday, November 19, 2008
The CUG triplet repeat at the root of myotonic muscular dystrophy
Scientists have identified a promising set of new compounds in the fight against muscular dystrophy. Using a drug-discovery technique in which molecules compete against each other for access to the target – the strand of toxic RNA that causes the most common form of muscular dystrophy in adults – a team at the University of Rochester Medical Center has identified several compounds that, in the laboratory, block the unwanted coupling of two molecules that is at the root of the disease.
The work was published online November 7 by the Journal of the American Chemical Society.
This discovery gives us, for the first time, a molecule that targets the wayward RNA at the root of myotonic muscular dystrophy,
said Benjamin Miller, Ph.D., the chemist who led the study. This is a first step toward developing a drug-like molecule that perhaps could be used someday to treat the disease. This lead molecule provides a framework for moving forward.
Researchers Identify Toehold for HIV’s Assault on Brain
Friday, November 14, 2008
Scientists have unraveled in unprecedented detail the cascade of events that go wrong in brain cells affected by HIV, a virus whose assault on the nervous system continues unabated despite antiviral medications that can keep the virus at bay for years in the rest of the body.
The new research reveals key steps taken in the brain by Tat, a protein that is central to HIV’s attack on cells called neurons. Researchers discovered the receptor that Tat uses to attack neurons, and they were able to reverse the effects of Tat in the laboratory by blocking the receptor.
The discovery of a major molecular player in the process opens up a new avenue for researchers to explore in their efforts to prevent or treat HIV’s neurological effects, for which there is no currently approved treatment. Researchers say that much of the molecular action that underlies HIV’s attack on the brain also occurs in other diseases, such as Parkinson’s and Alzheimer’s diseases, and that the results spell progress for those conditions as well.
The team from the University of Rochester Medical Center and other institutions published its results online Nov. 13 in the journal PloS One.
Alzheimer's Gene Slows Brain's Ability to Export Toxic Protein
Thursday, November 13, 2008

A ring of amyloid in the wall of an arteriole
in the brain of a patient who had Alzheimer's disease
(Courtesy of James M. Powers, M.D.)
The only known genetic risk factor for Alzheimer's disease slows down the brain's ability to export a toxic protein known as amyloid-beta that is central to the damage the disease causes, scientists have found.
The research, published Nov. 13 by the Journal of Clinical Investigation, provides new clues into the workings of a protein known as apolipoprotein E4, or ApoE4. People who carry two copies of the gene have roughly eight to 10 times the risk of getting Alzheimer's disease than people who do not.
The new results are in line with a body of research amassed over the last 15 years by the leader of the team, Berislav Zlokovic, M.D., Ph.D., of the University of Rochester Medical Center, that blood circulation plays a key role in the disease. His team has identified much of the molecular machinery that allows amyloid-beta to sidestep the body's safeguards and enter the brain, and he has discovered molecules that falter when the toxic protein accumulates in the brain.
Our latest findings help explain one of the major risk factors for Alzheimer's disease,
said Zlokovic. ApoE4 changes the brain's ability to rid itself of amyloid-beta. It's becoming more and more apparent that the brain's ability to clear out amyloid-beta, through the vascular system and across the blood-brain barrier, is central to the development of Alzheimer's disease.
Music on My Mind Chamber Orchestra Set to Debut
Tuesday, November 11, 2008
More than 30 health care professionals from throughout the University of Rochester Medical Center are getting ready for their inaugural orchestral performance tomorrow afternoon. The Music on My Mind Chamber Orchestra, which includes a broad cross section of health care disciplines, including an emergency medicine physician, a scientist in the Laboratory for Laser Energetics, and an athletic trainer, will play at 4:30 p.m. Wednesday, Nov. 12 in the Flaum Atrium.
Conducted by David Harman, who also conducts the University of Rochester’s Symphony Orchestra and Chamber Orchestra, as well as the Penfield Symphony and the Rochester Philharmonic Youth Orchestra, the group will perform selections by Mozart, Beethoven and von Weber.
Pearson Lands Two National Leadership Appointments
Friday, November 7, 2008
International heart and stroke prevention expert Thomas Pearson, M.D., Ph.D., has been tapped by two national organizations to lead efforts aimed at decreasing the incidence of two of the nation's leading causes of death and disability: cardiovascular disease and stroke. Pearson is the Albert D. Kaiser Professor in the Department of Community and Preventive Medicine and Professor of Medicine at the University of Rochester School of Medicine and Dentistry.
For the past three decades, Pearson has been a driving force behind the development of many of our nation's policies and guidelines as they relate to heart disease and stroke. He has participated on dozens of policy panels for national organizations including The National Institutes of Health, the Centers for Disease Control and Prevention, the Institute of Medicine, the American College of Cardiology and the American Heart Association.
URMC Expert on Stroke to Give Free Talk
Wednesday, October 15, 2008
Curtis Benesch, M.D., director of the Strong Stroke Center at the University of Rochester Medical Center, will give a free talk on Treatment and Prevention of Stroke
from 4 to 5:30 p.m. Monday, Nov. 3, at the Hahnemann Club, 301 Stoutenburgh Lane, located on the campus of The Highlands at Pittsford, off of Route. 31, just east of the village Pittsford.
Benesch will discuss how to recognize the symptoms of a stroke, what to do when those symptoms occur and how to prevent a stroke in high-risk individuals. Also discussed will be the treatment of acute stroke and the many ways patients can decrease their risk.
Neurologist to Discuss Pioneering Stem Cell Research
Friday, October 3, 2008
Steven Goldman, M.D., Ph.D., professor and chair of the Department of Neurology, will discuss his pioneering efforts to use stem cells to treat human disease as part of a lecture series highlighting biological and biomedical research at the University of Rochester.
Goldman will speak at 4 p.m. Friday, Oct. 10, in the Class of 1962 Auditorium at the Medical Center. It's the latest installment of the Second Friday Science Social
lecture series geared mainly to faculty, staff and students at the University, though the general public is welcome as well.
Goldman, who is also professor of Neurosurgery, is internationally recognized for advancing our understanding of stem cells and their use to treat human disease. He began his studies of the brain's stem cells more than 25 years ago, and his doctoral thesis in 1983 was the first report of neurogenesis -- the production of new brain cells -- in the adult brain and opened the door to the idea of neural stem cells as the source.
Out of Iraq Emerges Hope for Those with the Severest of Head Injuries
Wednesday, September 24, 2008
There may be more hope than has been recognized for some people with severe brain injuries, according to a U.S. neurosurgeon who earlier this year spent four months in Iraq treating soldiers and civilians. Jason Huang, M.D., this week presented his results from his experience in Iraq at the annual meeting of the Congress of Neurological Surgeons in Orlando, Fla.
Huang discussed blast injuries, a type of wound that has affected thousands of U.S. soldiers and others in Iraq. The term includes injuries caused by roadside bombs or improvised explosive devices (IEDs
), as well as car bombs, suicide bombs, and other blasts.
This is a type of injury unlike anything seen regularly here in the United States,
said Huang, an assistant professor of Neurosurgery at the University of Rochester Medical Center who is also a major in the U.S. Army Reserve.
Here we might see gunshot wounds to the head, or severe injuries from motor vehicle accidents, but we don't see blast injuries, and so neurosurgeons haven't really had much experience treating them. What we're seeing in Iraq is different even from injuries suffered by soldiers in previous wars. The extent of the blast injuries was far worse than I ever would have imagined,
Huang said.
Rochester Neuroscientist Honored By Danish Academy
Tuesday, September 23, 2008
Maiken Nedergaard, M.D., D.M.Sc., has been elected a member of the Royal Danish Academy of Sciences, the premier scientific society in Denmark. The society elects only six new members worldwide every other year.
Nedergaard has been a pioneer in brain research, demonstrating that brain cells known as astrocytes play a role in a host of human diseases. For decades, much of the attention of neuroscientists had been focused on brain cells known as neurons, which send electrical signals. Astrocytes were long considered cells whose primary function was to support the neurons.
Nedergaard has turned that notion on its head, showing that astrocytes themselves play an important role in epilepsy, spinal cord disease, migraine headaches, stroke, and Alzheimer's disease.
Researchers Disclose Key Advance in Treating Spinal Cord Injuries
Friday, September 19, 2008
Researchers in Rochester, NY and Colorado have shown that manipulating stem cells prior to transplantation may hold the key to overcoming a critical obstacle to using stem cell technology to repair spinal cord injuries.
Research from a team of scientists from the University of Rochester Medical Center and the University of Colorado Denver School of Medicine, published online today in the Journal of Biology, may lead to improved spinal cord repair methods that pave the way for victims of paralysis to recover the use of their bodies without the risk of transplant-induced pain syndromes.
The research focuses on a major support cell in the central nervous system called astrocytes. When nerve fibers are injured in the spinal cord, the severed ends of the nerve fibers fail to regenerate and re-connect with the nervous system circuitry beyond the site of the injury. During early development, astrocytes are highly supportive of nerve fiber growth and scientists believe that, if properly directed, these cells could play a key role in regenerating damaged nerves in the spinal cord.
University of Rochester and The Highlands at Pittsford Present To Your Health!
Friday, September 19, 2008
The free To Your Health! series featuring health experts from the University of Rochester Medical Center resumes in September, with programs offering advice on learning more about your health and preventing and treating common age-related health issues.
Offered at convenient times, the afternoon programs are taught by URMC’s distinguished physicians and other providers affiliated with Strong Memorial Hospital, Highland Hospital, the Eastman Dental Center, Visiting Nurse Service and other affiliates of the Medical Center.
All lectures through November will be held at the Hahnemann Club, 301 Stoutenburgh Lane, located on the campus of The Highlands at Pittsford, off of Rt. 31, just east of the village of Pittsford. The Club is an ideal setting for learning and socializing with curious, like-minded peers, and parking is conveniently located right outside the clubhouse, along the street.
All seminars are free but registration is limited. Register by calling 585-275-2838.
Gelbard Named Director of Center for Neural Development and Disease
Thursday, September 18, 2008
Harris A. Gelbard, M.D., Ph.D., professor of neurology, pediatrics and of microbiology and immunology, has been named director of the Center for Neural Development and Disease at the University of Rochester Medical Center.
The center, which brings together a broad array of physicians and scientists, targets a complex system rather than a single disease. Center researchers investigate stroke, traumatic brain injury, brain tumors, nerve injuries, HIV-1 associated neurologic disorders, Alzheimer's and other diseases with the goal of creating treatments and therapies.
We think it is most crucial to understand the development of the nervous system — how it is put together — so we can better understand how diseases of the brain and peripheral nervous system take away function,
said Gelbard. This kind of understanding is what translates into treatments and better care.
Steven Goldman to Lead University’s Department of Neurology
Thursday, September 4, 2008
After an extensive national search, a neurologist who is a leading international figure in efforts to use stem cells to treat human disease has been tapped to lead the Department of Neurology at the University of Rochester Medical Center.
Steven Goldman, M.D., Ph.D., a professor of Neurology who has been with the University since 2003, will become the Edward A. and Alma Vollertsen Rykenboer Professor of Neurophysiology Chair, Department of Neurology within the School of Medicine and Dentistry beginning October 1. He will lead a department known nationally for its research and the education it provides its students and young doctors.
Dr. Goldman’s efforts will be central to the advancement of the field of neuromedicine, an area we’ve targeted in our strategic plan for significant growth and future investment in faculty and resources,
said Bradford C. Berk, M.D., Ph.D., Medical Center CEO. His experience as an outstanding researcher and clinician is a perfect fit for the position.
Wilmot Cancer Center Answers Calls to Stand up to Cancer Sept. 4
Wednesday, September 3, 2008
Doctors from the James P. Wilmot Cancer Center will answer questions about cancer screening, diagnoses, treatment and ways to reduce your risk during a special call-in program set from 5 to 6:30 p.m. Thursday, Sept. 4. The event is part of the Wilmot Cancer Center’s participation in the national Stand Up To Cancer effort.
URMC & NIH Partner to Expand, Accelerate Clinical Research in Neurological Diseases
Thursday, August 14, 2008
The University of Rochester Medical Center and the National Institute of Neurological Disorders and Stroke are hosting a week-long training session designed to create a new generation of researchers with the specialized skills necessary to conduct clinical trials in neurological disorders.
The session, which is titled the Clinical Trial Methods Course in Neurology,
is part of a push on the part of the National Institutes of Health to beef up the nation’s translational research capabilities by increasing the ranks of clinical researchers and focusing more resources on clinical research skills, technologies, and systems that will accelerate medical discoveries.
Neurological disorders are a critical area of need in terms of expanding our ability to design and conduct trials that have maximum efficiency at the lowest possible cost,
said URMC neurologist Bernard Ravina, M.D., the director of the course. Participants in this course consist of a select group of individuals who are committed to being clinical researchers and conducting clinical trials and will benefit from hands-on training that they really cannot get anywhere else.
AHA Recognizes Quality of URMC Cardiac, Heart Failure, Stroke Programs
Tuesday, July 15, 2008
The American Heart Association/American Stroke Association has honored Strong Memorial Hospital of the University of Rochester Medical Center with a Triple Performance Achievement Award for meeting its high standards for coronary artery disease, heart failure and stroke care.
Strong Memorial is the only Rochester-area hospital to receive this honor, and the only Rochester-area hospital to receive any level of American Heart Association recognition for its coronary artery disease and heart failure care.
The achievements of Strong Memorial in three program modules of the AHA/ASA Get With the Guidelines program consist of: coronary artery disease and stroke care, which each earned a Gold Sustained Performance Award to celebrate two or more years of adherence to all measures of AHA/ASA performance standards; and heart failure care, which received a Silver Performance Achievement Award for 12 consecutive months of compliance of performance measures.
Quick Formula Could Forecast Which Cancers Chemo Could Kill
Tuesday, July 15, 2008
Researchers at the University of Rochester Medical Center have coined a simple formula that predicts how well a certain chemotherapy will work for targeting brain and other nervous system cancers. The formula, which will publish in mid-July in Cancer Chemotherapy and Pharmacology, is pegged to two important proteins that compose such hard-to-kill tumors – one of which, ironically, makes them so drug-resistant in the first place.
We’re unraveling the mysterious, even paradoxical, ways chemotherapies interact with various cancers,
said one of the study’s investigators Nina F. Schor, M.D., Ph.D., the William H. Eilinger professor and chair of the Department of Pediatrics at Rochester. From this, we’re developing techniques that will help us more quickly predict which medicines are most effective for each tumor.
Doctors Testing New Treatments for Lower Back Pain
Wednesday, June 11, 2008
Physicians are testing two drugs approved to treat other conditions to see whether they might also help patients who have severe pain in their lower back and in their legs. The research studies at the University of Rochester Medical Center are part of an effort to come up with new treatments for pain caused by a condition known as lumbar spinal stenosis. Doctors are looking for up to 75 people to take part in the studies.
Lumbar spinal stenosis is the most common reason that people older than 65 choose to have back surgery. Nerve roots in the spinal canal are put under pressure as age causes the bones in our back to degenerate. The pressure on the nerves results in pain, sometimes very severe, in the lower back and the legs when patients stand or walk.
Doctors turn to a variety of drugs to treat the pain, but no drug has ever been proven to relieve the pain effectively. Even the most effective solution, surgery, does not significantly relieve pain in approximately one-third of patients. A study recently published in the New England Journal of Medicine found that the pain relief experienced by many patients after surgery often did not translate into better mobility and function in their daily lives.
Neurologist John Markman, M.D., assistant professor and director of Translational Pain Research in the Department of Neurosurgery, designed the new studies to study the benefit of non-surgical treatments.
World Experts in Specialized Radiation Therapy to Gather at URMC
Wednesday, June 11, 2008
Cancer survivor Jarod Finlay will share his experiences as the first patient to undergo an investigational procedure – stereotactic body radiation therapy – during a conference of world experts on the procedure this Friday and Saturday at the University of Rochester Medical Center.
Finlay, who had metastatic tumors in his lungs, received the groundbreaking therapy more than seven years ago when his doctors treated his lung tumors using technology originally designed to destroy brain tumors. This technique and scientists’ research to support its expanded use will be discussed by more than 100 experts attending the Scientific Conference on Stereotactic Body Radiation Therapy. Finlay will deliver the opening address by describing his care and perspective.
Human Stem Cells Show Promise Against Fatal Children’s Diseases
Wednesday, June 4, 2008
Scientists have used human stem cells to dramatically improve the condition of mice with a neurological condition similar to a set of diseases in children that are invariably fatal, according to an article in the June issue of the journal Cell Stem Cell.
With a one-time injection of stem cells just after birth, scientists were able to repair defective wiring throughout the brain and spinal cord – the entire central nervous system – of mutant shiverer mice,
so called because of the way they shake and wobble. The work marks an important step toward the day when stem cells become an option for the treatment of neurological diseases in people.
Neuroscientists at the University of Rochester Medical Center injected a type of fetal human stem cell known as glial stem cells into newborn mice born with a condition that normally claims their lives within about 20 weeks of birth, after a lifetime of seizures and other serious consequences. While most of the 26 mice that received transplanted glial stem cells still died, a group of six lived far beyond their usual lifespan, and four appeared to be completely cured – a first for shiverer mice. The scientists plan to gather more evidence before trying the approach in sick children.
It’s extremely exciting to think about not only treating but actually curing a disease, particularly an awful disease that affects children,
said neurologist Steven Goldman, M.D., Ph.D., a leader in manipulating stem cells to treat diseases of the nervous system.
Conference to Highlight Rochester Stem Cell Research
Monday, May 12, 2008
A half-day symposium showcasing research in the field of stem cell biology at the University of Rochester will be held on May 23. The symposium, titled Frontiers in Stem Cell Medicine,
is being sponsored by the University’s Clinical and Translational Science Institute and the Stem Cell and Regenerative Medicine Institute.
Speakers at the symposium include: biomedical geneticist Mark Noble, Ph.D., director of the Stem Cell and Regenerative Medicine Institute; neurologist Steven Goldman, M.D., Ph.D., chief of the Division of Cell and Gene Therapy; cancer researcher Craig Jordan, Ph.D., director of Translational Research for Hematologic Malignancies at the James P. Wilmot Cancer Center; Edward Puzas, Ph.D., with the Department of Orthopaedics, and Rocky Tuan, Ph.D., chief of the Cartilage Biology and Orthopaedics Branch of the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
May 1 Picnic to Celebrate Brain Tumor Awareness Week
Wednesday, April 30, 2008
Brain tumor survivors and their families, friends and University of Rochester Medical Center staff will celebrate Brain Tumor Awareness Week with a picnic from 5 to 8 p.m. Thursday, May 1, at Kings Bend Park in Pittsford.
Many in attendance at the picnic will be members of Brainstormers and the Adult Brain Tumor Network at Strong Memorial Hospital and the James P. Wilmot Cancer Center, which provide support for brain cancer survivors and their families. Every year, more than 185,000 people will be diagnosed with brain tumors in the United States.
Brain Tumor Care, Treatment in Spotlight
Thursday, April 24, 2008
Patients, physicians, and those caring for loved ones with brain tumors will have an opportunity to attend two full days of programs hosted by health care professionals from the University of Rochester Medical Center. The efforts, co-sponsored by the James P. Wilmot Cancer Center, are offered through the recently enhanced brain tumor treatment program at the University, where approximately 500 brain tumor patients are treated each year.
A seminar Saturday, April 26, will focus on people caring for patients with brain tumors. One week later, on Friday, May 2, another full-day session is geared toward patients, their families, and physicians, covering the latest research and treatment approaches in brain and spinal tumors.
Neurologist Wins Fellowship to Support Parkinson’s Research
Thursday, April 24, 2008
A physician at the University of Rochester Medical Center has been recognized for her work aiming to ease the side effects of medications widely used to treat patients with Parkinson's disease.
Michelle Burack, M.D., Ph.D., instructor of Neurology and Pediatrics, received a clinical research training fellowship from the American Academy of Neurology. The fellowship covers her salary and related costs for two years.
Burack is studying ways to try to alleviate some of the troublesome consequences of treatment that many patients with Parkinson's disease face. The disease is marked by shaky, stiff and slow movements, a result of the death of key nerve cells in the brain known as dopamine neurons. Early treatment with a medication designed to boost the amount of the signaling molecule dopamine in the brain is usually very effective.
Promising Parkinson's Finding Spurs New Clinical Study
Tuesday, April 15, 2008
The progression of Parkinson’s disease is slower in patients who have high blood levels of urate, a close chemical cousin of the molecule that causes gout, researchers have found. The finding could lead to a way to predict how a given patient with the disease will fare, and it opens the door to a new approach for treating or preventing the disease.
The findings were made public - posted online by the Archives of Neurology on April 14 - the same day that the Michael J. Fox Foundation announced a new study aimed at slowing the disease by continuing the research in people. The foundation is funding a $5.6 million study, the largest award in the foundation’s history, to investigate the potential of boosting urate levels to slow or stop the disease.
The project is being led by physicians at Harvard and Massachusetts General Hospital together with neurologists at the University of Rochester Medical Center.
Leaky Blood Vessels Open up Nerve Cells to Toxic Assault In Lou Gehrig’s Disease
Monday, April 7, 2008
Leaky blood vessels that lose their ability to protect the spinal cord from toxins may play a role in the development of amyotrophic lateral sclerosis, better known as ALS or Lou Gehrig’s disease, according to research published in the April issue of Nature Neuroscience.
The results mark the first time that scientists have witnessed molecular changes occurring long before key nerve cells start dying. The unexpected finding opens up a new front in studies of ALS, a disease in which motor neurons in the spinal cord die off for unknown reasons, resulting in dramatically weakened muscles. Patients lose their strength, their ability to move or swallow, and eventually lose their ability even to breathe. Most patients live only a few years after diagnosis.
We believe these changes contribute to or possibly initiate the onset of ALS,
said lead author Berislav Zlokovic, M.D., Ph.D., of the University of Rochester Medical Center. It’s clear that these changes occur before the loss of neurons, and it’s well known that the types of changes we are seeing certainly injure or kill these types of cells, which are extremely sensitive to their biochemical environment.
Stopping a Receptor Called 'Nogo' Boosts the Synapses
Tuesday, March 18, 2008
Changing dendritic spines on a neuron - evidence of brain rewiring
New findings about a protein called the nogo receptor are offering fresh ways to think about keeping the brain sharp. Scientists have found that reducing the nogo receptor in the brain results in stronger brain signaling in mice, effectively boosting signal strength between the synapses, the connections between nerve cells in the brain. The ability to enhance such connections is central to the brain's ability to rewire, a process that happens constantly as we learn and remember. The findings are in the March 12 issue of the Journal of Neuroscience.
The work ties together several research threads that touch upon the health benefits of exercise. While those benefits are broadly recognized, how the gains accrue at a molecular level has been largely unknown. The new research gives scientists a way to produce changes in the brain that mirror those brought about by exercise, by reducing the effect of the nogo receptor.
The find comes as a surprise, because for much of the last decade, the nogo receptor has been a prime target of researchers trying to coax nerves in the spinal cord to grow again. They named the protein after its ability to stop neurons from growing. Its action in the brain has not been a hot topic of study.
Friday Open House for New Neurology Outpatient Clinic
Wednesday, March 12, 2008
The Department of Neurology is holding an open house for its new outpatient clinic located on the first floor of the Ambulatory Care building. The open house will be held on Friday, March 14 from 11:00 a.m. to 1:00 p.m.
This new clinic is the culmination of years of growth and planning and will now enable us to provide our patients with the level of care they require in a setting that is far more convenient and designed to their needs,
said Robert C. Griggs, M.D., chair of the Department of Neurology.
Our Understanding of Movement Is on the Move
Monday, January 14, 2008
How our brain controls our movements is a bit more complex and varied than scientists have previously recognized, according to research recently published in Science by a team of scientists and physicians at the University of Rochester Medical Center.
The team led by neurologist Marc Schieber, M.D., Ph.D., professor of Neurology and of Neurobiology & Anatomy, showed that at least occasionally, the brain is able to bypass the usual route of nerve fibers it uses for controlling hand and finger movements, using an alternate route to send its signals. Such flexibility in controlling movement has been suspected but not actually shown before.
Copper Damages Protein that Defends Against Alzheimer’s
Wednesday, November 7, 2007
The research by neuroscientists at the URMC was presented at the annual meeting of the Society for Neuroscience in San Diego Nov. 3-7. The work was highlighted as part of a press conference on potential environmental influences on Alzheimer's disease.
The team found that copper damages a molecule known as LRP (low-density lipoprotein receptor-related protein), a molecule that acts like an escort service in the brain, shuttling amyloid-beta out of the brain and into the body. The molecule's role in Alzheimer's was revealed more than a decade ago by another author of the work, Berislav Zlokovic, M.D., Ph.D., professor of Neurosurgery and Neurology and director of the Frank P. Smith Laboratory for Neuroscience and Neurosurgery Research. Zlokovic is widely recognized for demonstrating that blood vessels, blood flow, and the blood-brain barrier are central to the development of Alzheimer's disease.
Study of New Epilepsy Treatment Underway at URMC
Saturday, September 15, 2007
The University of Rochester Medical Center is participating in a multi-center study of a new medical device to treat epilepsy. The Rochester study is being overseen by neurologists Michel Berg, M.D. and James Fessler, M.D., and neurosurgeons Web Pilcher, M.D., Ph.D. and Jason Schwalb, M.D.
Uncontrolled seizures related to epilepsy are generally treated with medications,
said Berg, medical director of the Strong Epilepsy Center. However, many individuals treated with medication alone continue to experience seizures or have unacceptable medication side effects. If these patients are not candidates for epilepsy surgery, then options to effectively control their seizures are limited.
Study of New Epilepsy Treatment Underway at URMC
Friday, September 14, 2007
The University of Rochester Medical Center is participating in a multi-center study of a new medical device to treat epilepsy. The Rochester study is being overseen by neurologists Michel Berg, M.D. and James Fessler, M.D., and neurosurgeons Web Pilcher, M.D., Ph.D. and Jason Schwalb, M.D.
Uncontrolled seizures related to epilepsy are generally treated with medications,
said Berg, medical director of the Strong Epilepsy Center. However, many individuals treated with medication alone continue to experience seizures or have unacceptable medication side effects. If these patients are not candidates for epilepsy surgery, then options to effectively control their seizures are limited.
The Responsive Neurostimulator System (RNS) is an implantable device that is designed to suppress seizures in patients with epilepsy before any symptoms appear, much like implantable cardiac pacemakers are intended to detect abnormal heart rhythms and then deliver electrical stimulation to correct them. Neuropace, the California-based developer and manufacturer of the RNS system, is funding the trial. URMC is one of 28 centers across the country testing the new technology.
Alzheimer’s Project Focuses on Role of Brain Inflammation
Thursday, August 30, 2007
Scientists at the University of Rochester Medical Center have received $1.37 million to continue their work looking at some of the earliest events that occur at the start of Alzheimer's disease - a condition that now generally goes undetected until the death of key brain cells has been underway for decades.
The team led by William Bowers, Ph.D., associate professor of Neurology and a scientist in the Center for Neural Development and Disease, is focusing on the role of inflammation in the evolution of the disease. Just as rheumatoid arthritis can ravage the body's joints because of the inflammation it causes, scientists are realizing that the same thing happens to the brain in patients with Alzheimer's disease. The brain can be under assault for decades as the body attempts to fend off some perceived threat.
Rochester Awarded New MS Research Center
Monday, June 12, 2006
A new research center whose scientists are working on better ways to treat multiple sclerosis has been established in Rochester by the National Multiple Sclerosis Society.
The University of Rochester Medical Center is bringing together experts who normally focus on Alzheimer’s disease, HIV vaccines, and spinal cord repair, as well as multiple sclerosis, in a unique center designed to stimulate MS research by drawing on the expertise of scientists from a wide array of disciplines. The new Collaborative Multiple Sclerosis Research Center Award – the only one in the nation established by the society this year – is headed by neurologist Benjamin Segal, M.D., associate professor of Neurology and director of Neuroimmunology Research. Segal has enlisted several of his colleagues to direct their attention on new ways to investigate the disease.
Also taking part in the project are neurologists Steven Schwid, M.D., and Andrew Goodman, M.D., who have extensive experience with clinical trials in MS; and Howard Federoff, M.D., Ph.D., and Tim Mosmann, Ph.D., who head research centers in aging and in vaccine biology, respectively.
New Findings About Brain's 'Compass' Offer Clues About Alzheimer's
Thursday, March 28, 2002
A tiny section of the brain that is ravaged by Alzheimer's disease is more important for our ability to orient ourselves than scientists have long thought, helping to explain why people with the disease become lost so easily. The findings by neuroscientists at the University of Rochester Medical Center are reported in the March 29 issue of Science.
Neurologist Charles Duffy, M.D., Ph.D., previously discovered that a small section of brain tissue slightly above and behind the ear - known as the medial superior temporal area (MST) - acts much like a compass, instantly updating your mental image of your body's movements through space. In new research, Duffy and graduate student Michael Froehler show that the MST acts not only as a compass but also as a sort of biological global positioning system, providing a mental map to help us understand exactly where we are in the world and how we got there.
Road Skills Hint At "Motion Blindness" Of Alzheimer's
Thursday, January 31, 2002
Doctors have added to the evidence that patients with Alzheimer's disease lose their way not simply because their memory is failing but because they are subject to a unique form of brain damage that causes symptoms doctors call "motion blindness." Some of the new data comes from driving tests of a small number of patients, where researchers have linked the condition to the loss of one specific driving skill: the ability to stay in one's lane while driving.
While it's obvious that people with Alzheimer's disease are losing their memory, that's only part of the reason why they become lost,
says neurologist Charles Duffy, M.D., Ph.D., who leads the research team at the University of Rochester Medical Center. These patients also lose their ability to perceive their own motion. That's ultimately what puts them at much greater risk than others of becoming lost.
New Mouse Marks Latest Stride in Muscular Dystrophy Research
Thursday, September 7, 2000
Most days, neurologist Charles Thornton, M.D., spends some time away from his patients and heads for the laboratory, where he works with mice. It might seem an unlikely action for a doctor ultimately concerned with human health. But his forays in the laboratory have helped Thornton and his team develop a new kind of mouse that may someday help doctors around the world treat patients with myotonic dystrophy, the most common form of muscular dystrophy in adults.
Two Scholars Win Sloan Fellowships
Tuesday, April 18, 1995
Charles J. Duffy, professor of neurology and ophthalmology, and Turan Erdogan, assistant professor of optics, have been awarded 1995 Sloan Research Fellowships.
The two University of Rochester professors were among 100 scientists and economists selected from a field of 400 nominees. Each Sloan Research Fellowship recipient is awarded $30,000 over a two-year period. Sloan Research Fellows are engaged in pioneering research in physics, chemistry, computer science, mathematics, neuroscience and economics. Once they have been selected, Fellows are free to pursue whatever line of inquiry interests them. The Alfred P. Sloan Foundation created the fellowship program in 1955 to encourage research by young scholars at a critical time in their careers.