About the Program

This fellowship integrates the history of the biopsychosocial model with cutting edge work in consultation subspecialties. Our strengths are in inpatient consultation, psychiatry in medicine and collaborative care, transplant psychiatry, and other sub-specialty consultation.
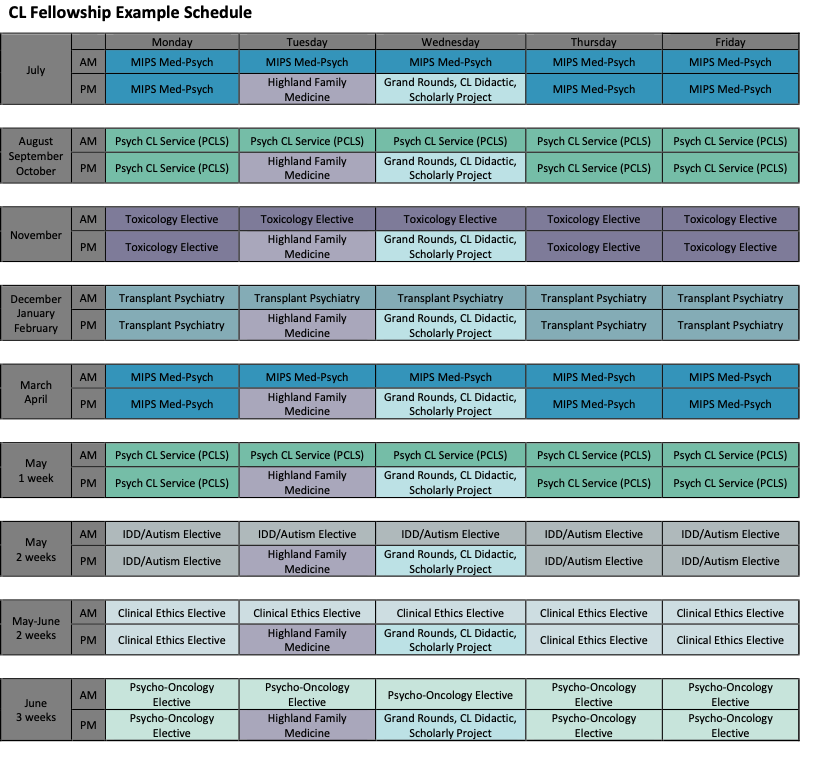
There are required rotations as well as many opportunities for electives based on fellow interest. Educational offerings include a weekly didactic series, monthly journal club as well as the weekly departmental grand rounds. The fellow is also heavily involved in teaching medical students and residents. Consultation-Liaison fellows are also required to complete a scholarly activity suitable for a poster presentation, which is included at the Department's Annual Poster Day.
Required Rotations
Psychiatric Consultation-Liaison Service
The Psychiatric Consultation-Liaison Service (PCLS) provides over 1800 consultations annually to Strong Memorial Hospital (SMH), the center of the University of Rochester Medical Center (URMC) health care delivery system. Strong Memorial has 886 patient beds and approximately 1400 full-time faculty members and 650 voluntary clinical faculty members organized into 32 departments and centers. It is the only Level 1 Trauma Center and quaternary care center in the region. The service operates both a traditional consultation model and a Proactive model. The service is staffed by psychiatrists and advanced practice nurses, and provides training to PGY-2 residents, Neurology and other residents, and medical students. While on this service, the Fellow will provide inpatient consultations and help train residents and students. The fellow will also have the opportunity to participate in telepsychiatry consultations to URMC-affiliated regional hospitals and Emergency rooms.
Transplant Psychiatry
Organ Transplant is a signature program of URMC, offering liver, kidney and heart transplantation. Annually, there are about 200 transplants in these programs. In addition, there is a robust VAD program, following over 200 VAD patients. Transplant Psychiatry has a full-time consultative presence in these programs; there are three transplant psychiatrists totaling over 1 FTE, as well as a psychologist embedded in the living donor program. The clinical work occurs in inpatient and outpatient settings and involves candidacy assessments of both recipients and donors, consultative short-term management of psychiatric issues, assessment and management of delirium, and helping patients and families with emotional adjustment when dealing with worsening health and during recuperation. Liaison work is a significant portion of the fellow’s experience, particularly in the heart transplant/VAD programs. The fellow will also participate in recipient listing and donor evaluation committee meetings.
The Medicine In Psychiatry Service (MIPS)
The URMC Psychiatry department has a division of Medicine in Psychiatry Services (MIPS) to address the often under-recognized medical needs of psychiatry patients. The specialized inpatient MIPS unit is a 20-bed acute med-psych unit for adults with acute medical conditions and concurrent psychiatric conditions. It is one of the few units of its kind in the entire country. The unit is staffed by family medicine and internal medicine physicians; some have additional training in addiction medicine, mental health, or geriatrics. There are two dedicated CL psychiatrists that round with the medical teams and provide proactive consultative psychiatric support. The interdisciplinary approach of MIPS includes close collaboration with colleagues in nursing, social work, psychology, psychiatry, pharmacy, substance and recovery counseling, and peer support. In addition, MIPS has a community-based patient-centered primary care medical home collocated with the Strong Ties program, an outpatient clinic for patients with serious mental illness. An important aspect of this rotation is learning about and experiencing an embedded model of psychiatric care and developing teaming skills.
Collaborative and Integrated Care
The Department of Psychiatry provides different models of integrated behavioral health care in a growing number of settings including Internal Medicine, Family Medicine, OBGYN, Neurology, Cardiology, Dermatology, and Oncology practices located throughout Rochester and the region. There are multiple different models used depending on the site including the Collaborative Care Model (IMPACT), and co-located care in addition to using multiple modalities including teleconsultations and e-consults. By being exposed to different models of integration and to different practices throughout the region, the Fellow can explore not only the clinical work in differing patient populations, but also how various care models can work.
Electives
While the fellow will have experiences with many of these subspecialties during required rotations, they can choose to do elective experiences in the following areas:
Psychiatry Elective Rotation Options:
Psychosocial Oncology (outpatient, inpatient)
Perinatal Consultation Clinic/Women’s Mental Health (outpatient)
Psychodermatology (outpatient)
Pain Psychiatry (outpatient)
Neuropsychiatry Integration (outpatient)
ECT / TMS consultations (outpatient, inpatient)
Geriatric Psychiatry consultations (inpatient, outpatient)
Bariatric Psychiatry evaluations (outpatient)
Addiction Psychiatry (outpatient, inpatient)

Off-service Elective Rotation Options:
Toxicology (inpatient)
Clinical Ethics (inpatient)
Epilepsy (inpatient)
Neurology Consult Service (inpatient)
Palliative Care (inpatient)
Movement Disorders (outpatient)
Neuroimmunology (mostly outpatient, some inpatient)
Headache (outpatient)
Pain treatment center (outpatient)

Eating Disorders (inpatient, outpatient)
IDD/Autism - Intensive Behavior Team and Complex Care Center (inpatient, outpatient)
In addition to these electives, the Fellowship is interested in providing its Fellows with experiences in areas that are of interest. Because URMC is an integrated academic health center that has specialists in every area of medicine, other electives can be arranged through discussions with the Program Director.