A Day in the Life of Our Residents
Obstetric Anesthesia
Soroush Besharat, MD - Class of 2027

My day starts when I wake up around 5:45 AM. I live very close to the hospital (8 minute walk), so I have the luxury of not having to deal with the busy parking lot madness in the mornings. After getting to the hospital, changing into scrubs, and greeting my fellow co-residents, I’m up on the labor and delivery floor by 6:30 AM to take sign-out from the overnight OB anesthesia resident.
Sign-out is where I get the lay of the land: who’s laboring, which epidurals are running, any complex patients to keep an eye on, and how wild the night shift was. From there, I log into Epic and get caught up on our patients—double-checking analgesia levels, reviewing labs, and making sure any consults or anticipated cases are accounted for. If there are scheduled C-sections, I will prepare the OR for the first case and pre-operatively evaluate the patient. Once that’s done, I round on our epidural patients to assess block levels, tweak infusions if needed, and just check in. It’s a nice part of the day to connect with patients and nurses before things really get moving.
From that point forward, anything goes. No two days are the same on OB. Some mornings are packed with elective C-sections, and other times we're managing multiple epidural placements, troubleshooting blocks, or responding to urgent pages. And yes, sometimes you hear that overhead call—OB STAT to the OR—and your heart skips a beat (before you’re running down the hallway).
We work closely with the obstetricians and nurses throughout the day, and there’s a strong sense of collaboration on the floor. Whether it’s managing a tricky labor epidural, placing a spinal for a STAT C-section, or preparing for a patient with complex comorbidities, the learning never stops. Most afternoons, once the pace slows a bit, there’s time for lunch and some structured teaching from one of our attendings. These mini-lectures are interactive and cover everything from the physiology of pregnancy to management of obstetric emergencies and the latest evidence behind our practices.
By mid-to-late afternoon, we begin prepping for the next day—checking scheduled cases, confirming anesthesia plans, and ensuring everything is in place for a smooth start tomorrow. Around 4:00 PM, we sign out to the OB "lates" resident, who covers until the night shift takes over around midnight. Of course, some days don’t go quite that smoothly—last-minute C-sections or epidural requests can roll in right before you leave, and it's always kind to take care of these loose ends before handing off to the "lates" resident.
After sign-out, I usually head home to decompress. Most days, I either go to the gym, on a long bike ride (weather permitting), or grab dinner/drinks with friends to maintain my sanity and prevent burnout. The OB anesthesia rotation is definitely one of the more dynamic and fast-paced experiences of residency. It challenges your clinical judgment, procedural skills, and ability to work as part of a truly multidisciplinary team. It’s exhausting at times—but incredibly rewarding.
Cardiac Anesthesia
Natasha Singh, MD- Class of 2026

Rise and shine; it’s 4:45am! Coffee’s brewing, protein bars are packed, and I’m skimming key points for the first case; an aortic valve replacement and single vessel CABG. After letting my dogs out in the yard and getting swindled by my cats for treats, I leave the house and arrive to the hospital around 5:30am. I set up my OR as I run through my checklist: ventilator, monitors, airway equipment, meds, pressor infusions on alaris pumps, and the transesophageal echocardiogram (TEE) machine. Around 6:30am, I greet our patient in the pre-op area. I go over their history, do a physical exam, get consent (including for post-op nerve blocks, courtesy of our rockstar acute pain team). I start my lines, placing an IV along with an ultrasound guided radial arterial line. After this, I’ll grab a sip of coffee, before heading back to the OR by 7:30am.
In the room, we place monitors, preoxygenate, with a smooth cardioprotective induction and intubation. As my attending places and navigates the TEE probe for initial imaging, I’m gowning up for a right internal jugular central line, placed after sterile prep and timeout. Once the case gets underway and sternotomy is made, pre-bypass TEE image findings are reviewed amongst our team along with the CT surgeon. My awesome attending sends me for a much- needed breakfast break. I return to find the case is progressing well, and we are soon to be on bypass. This portion of the case requires continuous communication amongst us, the surgical team, and the perfusionist. While managing perfusion pressures on bypass, I also set up for the next case, make an ICU transfer bucket and handoff sheet, discuss key learning points with the attending, review TEE images, and sneak in some case specific reading. Around 12pm, I grab some lunch and eat with my co-residents in the lounge.
Once we are coming off pump, all hands are on deck! We restart the lungs and the heart, manage arrhythmias, transfuse blood products, adjust anesthetic depth, rewarm the body, review blood gases, all while obtaining post repair TEE imaging to check for valve gradients, systolic function, and ejection fraction. Once we close, we take the patient sedated and intubated to the CVICU and give hand off to the team. Round two! I quickly turn over the room, and we get underway with our next case- an ECMO decannulation. Just like that, its 5pm and the resident or fellow on call relieves me for the night. I give hand off, pre-chart tomorrow’s cases, and chat with my attending about the plan. I get home around 6pm. The dogs get a long walk, dinner goes on the stove, and then I’ll sit down to study (or read a book, watch some Netflix, because— balance, right?). I tucker out by 9:30pm, ready to do it all again tomorrow!
Transplant Anesthesia
Tyler Lang, MD, MPH - Class of 2026

Days on the Transplant rotation are a bit variable given the unpredictability of organ availability. On a “standard” day when there is no imminent liver transplant, I’ll show up between 6 and 6:30 to set up my room for cases. You’ll usually be assigned to either a kidney transplant or a larger abdominal surgery such as a hepatectomy or a Whipple. These cases are engaging and typically require larger line placement. I usually end up leaving between 3:30 and 5, if not on call.
When you’re the transplant resident on-call and there is a pending liver transplant, it’s a different story. You’re alternating calls for two weeks at a time with another resident. I’ll get to the hospital 2-3 hours ahead of the start to give myself plenty of time to set up the room. There are tons of supplies and equipment you need to have ready to start these big surgeries. The team can begin at any hour of the day because of the limited survivability of a liver once removed, so if there is a late start, the clinical coordinators try to send you home from daytime duties to get a bit of rest. They can be long and intense operations, but the surgical teams and anesthesia attendings are all wonderful to work with and cases typically fly by. I feel like I’ve come away with a lot of new knowledge and confidence from having experienced liver transplants.
You’ll also get the occasional scheduled live liver donor, which involves two simultaneous surgeries where they’ll take a segment of liver from a donor and wheel it across the hallway to the recipient. These are also long days (sometimes up to 18+ hours) but you’ll likely get a post-call day at home to recover!
Anesthesia OR Orientation
Henry Zimmer, MD- Class of 2028

One of the highlights of our program is the opportunity to begin our clinical anesthesia training and OR orientation early on during our CBY (intern) year. Half of the class begins with anesthesia orientation in September, and the latter half in January. Not only are you able to obtain plenty of anesthesia experience early on, but you also begin to build relationships with senior residents, faculty, and other perioperative staff with this opportunity.
The first week of orientation consists of a lecture series led by senior residents and attendings. During this week, we arrive around 8 AM and have lectures until around 3 or 4 PM. These lectures focus on all of the basic topics you need to review before begin working in the ORs, including basic pharmacology and physiology, volatile anesthetics, airway management, fluid management, properties of the anesthesia machine, preoperative evaluation, etc.
The second week of orientation is your first actual experience in the operating room, and you are paired up with a senior resident. The day before, you check what cases you are assigned to, write the preoperative note including your anesthetic plan, and then contact your attending to discuss the plan for the next day. You can expect to arrive to work around 6:30, as this will give you enough time to set up the room and go evaluate the first patient. Being paired up with a senior for the first week allows them to show you the ropes and the general flow of the day. You are dismissed from the OR by 3:30 PM at the latest, and then you will have a daily lecture until around 4:30 or 5 PM.
Weeks 3-6, you are paired up with another co-intern and an attending preceptor for the week. During this week, you and your co-intern will generally rotate who takes the "lead" for each case. Whoever is taking the lead for the case will do the majority of the management of the case, while the other intern sits back with the attending, and it is a great opportunity for some one-on-one intraoperative teaching. The attending is in the room with you the entire time, so there is plenty of time for teaching and questions. These weeks you are again relieved at 3:30 to attend afternoon lecture. I really enjoyed these weeks as I was able to build stronger relationships with different co-interns and attendings because we worked together for an entire week.
During the last week of orientation, you are again paired with a senior resident, similar to the second week. On the last day, each individual resident is sent to our anesthesia simulation room to showcase what they have learned the last 8 weeks and make sure they are ready to begin delivering anesthesia safely in a more independent setting. Throughout the entire orientation you are leaving the hospital by 4:30 or 5 PM at the latest. This allows you to go home with plenty of time to unwind, study if you wish, or pursue any other hobbies you might have.
Night Float
Jeff Seeley, MD- Class of 2028

At URMC, we use a designated night float rotation with three residents (with the occasional moonlighter and CRNA) to cover the ORs overnight. A week of nights entails a total of 6 shifts, starting on Saturday night and ending on Friday morning, with shifts lasting from 6:45pm – 7:00am. We start covering nights as early as intern year, depending on how yearly rotation scheduling works out. I received lectures from residents in all years and was able to work with them in the ORs in the early part of the orientation.
During my week of nights, I will typically arrive at the hospital around 6:30pm to give myself enough time to change into scrubs and take a peek at the OR board to see what cases are still going. Most nights, you’ll be relieving someone from one of the ORs right away and will finish up the case (hopefully quickly!). The weekends are usually less busy at the start of the shift with fewer ORs running than during the week, so you may have some free time in the beginning! As a junior resident, nights are an incredible time for rapid learning and getting exposure to cases you likely have not experienced yet during normal daytime shifts – don’t worry, we have amazing senior residents and night attendings that will be there to help! As a level 1 trauma center, Strong gets anything and everything. My first week of nights featured an emergent craniotomy and a couple of ruptured aortic aneurysms, as well as more typical “intern-level” cases, so you never know what might come up in the middle of the night!
On top of emergent cases, you might also get the chance to do some nerve blocks and floor airways, depending on how the week goes. If there’s downtime during the night, we usually fill it with movies/gaming in the lounge, mid-night cafeteria runs, or sleep (of course!). Although it can be intense at times, nights are a great time for bonding with senior residents, expanding your growing skill set, and gaining confidence in managing high acuity cases.
SICU
Molly Cherny, DO- Class of 2029
My day on SICU starts at around 5am when I wake up thinking about my first sip of coffee. As an intern, this 3-week rotation entails working six days a week from 6a-6p, with Thursday as my day off. SICU is split between two units, either 81400 or 83600, with similar patients and staffing in each. I roll into the hospital at about 5:45am, which gives me enough time to be ready for sign out at 6am from the night APP or senior resident. During the day each unit generally has a team of 2 interns, 1 PGY2/3, an APP, and sometimes a MICU fellow. Residents from anesthesiology, emergency med, & all the surgical subspecialties rotate through SICU and may be part of the team. The APPs run the teams with the help of the attending who rounds and then is available for questions throughout the day.
In the clinic, which opens at 8:00am, we see both new and established patients. After sign out, between 6:30-8ish, I preround on my patients and write my notes/my preliminary plan, review consult recommendations, review and edit orders, etc. I carry 2-3 patients most days and occasionally 4 when it's busy. Morning rounds depend on the attending but generally start between 8:30-10:00. After rounds, I ensure all the orders are updated based on my new or confirmed plan, do procedures that are needed, call and give updates to family, and take some downtime. At first, I was afraid to leave the unit, but everyone does and it's okay! It is nice to take a break from a stimulating environment when patients are stable and tasks are complete, and the nurses are great at reaching out if they are concerned or need something. I also use this time to look into some of the other patients on the unit who I'm not specifically covering. We are a liver transplant center, so a lot of SICU patients are chronic cirrhosis patients, either pre or post-transplant, which are great patients to learn balancing complex pathophysiology.
We typically afternoon round at some point, and there is ICU education at 3pm every weekday. I enjoy the education sessions as they cover different MICU and SICU topics as well as some ethical/social circumstances. New consults come in throughout the day and are taken by the APP or senior resident, but whenever a new patient comes, we help update their problem list and pend an H&P for their SICU admission prior to them arriving at the unit.
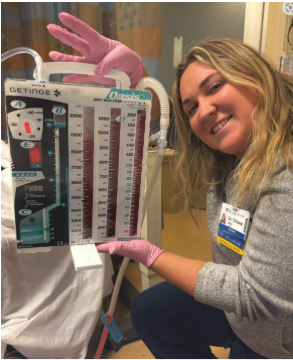
Procedure wise, I was able to place a couple of arterial lines, perform multiple rapid sequence intubations, and even place a chest tube (proud photo evidence of successful drainage)! Overall, SICU is a busy rotation with a lot of hours, but as an intern it is a rewarding experience full of learning and collaboration with other specialists, and I felt supported by the other residents, APPs, and attendings who are happy to teach while still providing some autonomy. Though high stress situations arose and I was responsible for critical patients, being exposed to this early in my intern year has helped prepare me for SICU nights as a CA-1 as well as for complex ICU level anesthesia cases.
Affiliate rotations
Esther Kim, MD- Class of 2028

As an anesthesiology resident at URMC, you will be well-trained in all aspects of anesthesiology. Our main hospital, Strong Memorial Hospital (SMH), is a tertiary/quaternary facility and the sole level 1 trauma center in the region. Therefore, complex cases are regularly transferred to us from surrounding hospitals. An additional bonus to training here is our affiliation with multiple regional healthcare facilities; this gives you the opportunity to provide anesthesia care outside of an academic institution. For example, Highland Hospital is a community hospital where attendings often perform their own cases; we also partner with multiple ambulatory surgical sites and to crank it up a notch, you even have the option for a rural rotation if that is an area of interest for you.
Gaining exposure to various health care settings during your residency training sets you up for success because you develop skills in efficiency, interpersonal communication, and adaptability; it can also help you find your niche within the broad world of anesthesiology. Thus far I have spent a total of 5 weeks in one of our affiliated sites. While it can be daunting at first to visit a new hospital, you'll quickly adapt with the help of hospital staff, senior residents and our resident guidebooks. Each site offers a different experience but to give you a sense of what I'm talking about, here's what a typical day at Highland Hospital looks like:
The first case starts at 7:30 and it's a 7-minute drive from my apartment and a 7-ish-minute walk from the parking garage to the locker rooms. I allow myself extra time to orient myself to a different hospital and aim to leave my apartment by 6:00. Once I enter Highland Hospital, I walk up to the 2nd floor to the operating rooms and take a moment to admire the stunning mural paintings in the staircase. After I change into OR scrubs, I drop off my lunch in the staff break room and head to my assigned OR. From here, I set up my first case and the rest of my day looks similar to a day at SMH; the main difference is the quick turnovers, so I'll often turnover my own room to avoid potential delays. After each case, I safely transport my patient to PACU and within half an hour, I'm rolling back with the next patient. After I finish my cases for the day, I check in with the clinical coordinator who usually sends me home. The cases I'm assigned to at Highland Hospital vary from ortho, ENT, breast surgery, gynecology, and urology. A core memory for me is that my first successful intubation with a Miller blade happened at Highland Hospital!
Chronic Pain Clinic
Monica Brown-Ramos, MD - Class of 2024

I wake up at around 6:30 am and arrive to the Chronic Pain Clinic by 7:20 am. First, I check in with the attendings working that day to find out whether I am most needed on the clinic team or procedure team. Today, I’ll be on the clinic side in the morning and the procedure side in the afternoon- the best of both worlds! At 7:30 am we have chronic pain lectures, taught by either an attending, fellow, or resident. The excellent 30-minute presentation today was about neuropathic pain management.
In the clinic, which opens at 8:00am, we see both new and established patients. We take detailed history on their pain and any treatments or diagnostic tests they’ve completed, perform a comprehensive physical exam, and then present to the attending. The attending reviews images with us and discusses important pharmacologic considerations for our treatment plans before going into the patient’s room and finishing the visit. Between visits, we put in orders and complete notes.
Lunch is around 12pm, and my first afternoon procedure is at 1pm. We do a number of procedures including epidural injections, radiofrequency ablations, sympathetic blocks, intraarticular and facet injections, spinal cord stimulator trials, and many more! The afternoon is spent completing the pre-procedure notes and assisting the fellow and attending during the procedure. The day flies by between the many procedures, and we are done at 4:30 pm! I check in with the clinic attendings to see if they need any more help. Upon completion, I will get the green light to go home!
When I get home, I catch up on reading about topics discussed during the day, and then spend the rest of the evening having dinner with my fiancé and going for a walk in our neighborhood. By the time 10pm rolls around, it’s time for bed, and I am ready for another day tomorrow!
