Spinal Cord Compression
What is spinal cord compression?
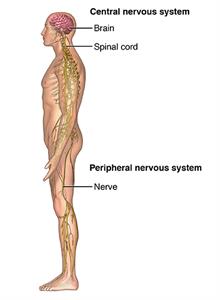
Spinal cord compression is caused by any condition that puts pressure on your spinal
cord. Your spinal cord is the bundle of nerves that carries messages back and forth
from your brain to your muscles and other soft tissues. As your spinal cord travels
down your back, it's protected by a stack of backbones called vertebrae. They also
hold your body upright. The nerves of your spinal cord run through the openings between
the vertebrae and out to your muscles.
Spinal cord compression can occur anywhere from your neck (cervical spine) down to
your lower back (very top of lumbar spine). Symptoms include numbness, pain, weakness,
and loss of bowel and bladder control. Depending on the cause of the compression,
symptoms may develop suddenly or gradually. They may require anything from supportive
care to emergency surgery. If compression becomes severe, a condition called myelopathy
may happen. Myelopathy leads to symptoms, such as problems with walking, pain, and
numbness.
What causes spinal cord compression?
One of the most common causes of spinal cord compression is the gradual wear and tear
on the bones of the spine. This is known as osteoarthritis. People who develop spinal
cord compression from this are usually older than 50.
Other conditions that may cause spinal cord compression can develop more quickly,
even very suddenly. These can occur at any age:
What are the symptoms of spinal cord compression?
Symptoms of spinal cord compression can develop quickly or slowly. It depends on the
cause. Injuries may cause immediate symptoms. Tumors or infections may cause symptoms
that develop over days or weeks. Wear and tear of the spine may take years to cause
symptoms.
These are common symptoms:
-
Pain and stiffness in the neck, back, or lower back
-
Burning pain that spreads to the arms, buttocks, or down into the legs (sciatica)
-
Numbness, cramping, or weakness in the arms, hands, or legs
-
Loss of sensation in the feet
-
Trouble with hand or leg coordination
-
"Foot drop," weakness in a foot that causes a limp
-
Loss of sexual ability
Pressure on nerves in the lumbar region (lower back) can also cause more serious symptoms
known as cauda equina syndrome. If you have any of these symptoms, you need to get
medical care right away, typically in the emergency room:
-
Loss of bowel or bladder control
-
Severe or increasing numbness between the legs, inner thighs, and back of the legs
-
Severe pain and weakness that spreads into one or both legs, making it hard to walk
or get out of a chair
How is spinal cord compression diagnosed?
To diagnose spinal cord compression, your healthcare provider will ask you questions
about your symptoms and do a complete physical exam. During the exam, they will look
for signs of spinal compression, such as loss of sensation, weakness, and abnormal
reflexes. Tests that help with your diagnosis may include:
-
X-rays of your spine. These may show bone growths called spurs that push against spinal
nerves. X-rays may also show an abnormal alignment of your spine.
-
Special imaging tests of your spine. A CT scan or MRI will give a more detailed look
at the spinal cord and the structures surrounding it.
-
Other studies. These may include a bone scan, a special X-ray or CT scan taken after
injecting dye into the spinal column (myelogram), and electromyography (EMG), an electrical
test of muscle activity.
How is spinal cord compression treated?
The medical team involved in treating your spinal cord compression may include arthritis
specialists, bone surgeons, nerve specialists, and physical therapists. Treatment
depends on the cause and your symptoms. It may involve medicines, physical therapy,
injections, and surgery. Except in cases of emergency, such as cauda equina syndrome
or a broken back, surgery is usually the last resort.
-
Medicines may include nonsteroidal anti-inflammatory drugs (NSAIDs) that relieve pain
and swelling and steroid injections that reduce swelling.
-
In more acute spinal cord compression, high-dose steroids are used to save nerve cells
until other treatment can be given.
-
Radiation therapy may be used to shrink tumors that are compressing the spinal cord.
-
Physical therapy may include exercises to strengthen your back, abdominal, and leg
muscles. You may learn how to do activities more safely. Braces to support your back
or a cervical collar may also be helpful.
-
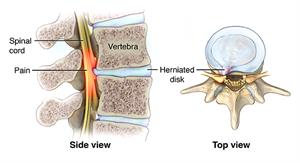
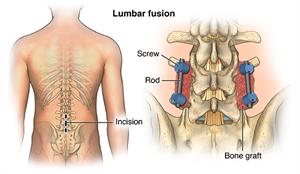
Surgical treatments include removing bone spurs and making the space between vertebrae
wider. Other procedures may be done to ease pressure on the spine or fix fractured
vertebrae. The back may also be stabilized by fusing some of the vertebrae together.
-
Some other treatments that may be helpful for some people are acupuncture and chiropractic
care.
What can I do to prevent spinal cord compression?
Many causes of spinal cord compression can’t be prevented. You can help prevent symptoms
of spinal cord compression caused by gradual wear and tear by keeping the muscles
and bones of your back as strong and healthy as possible.
-
Get regular exercise. Exercise makes the muscles that support your back stronger and
helps keep your spine flexible.
-
Maintain good posture and learn how to safely lift heavy objects. Other good body
mechanics include sleeping on a firm mattress and sitting in a chair that supports
the natural curves of your back.
-
Maintain a healthy weight. Excess weight puts more stress on your back. It can contribute
to developing symptoms of spinal compression.
-
Eat a well-balanced diet.
-
Don't smoke.
How is spinal cord compression managed?
The best way to manage spinal cord compression is to learn as much as you can about
your condition, work closely with your healthcare providers and caregivers, and take
an active role in your treatment.
Keep your back as healthy as possible. Stay at a healthy weight. Practice good body
mechanics. Get regular exercise.
Simple home remedies like an ice bag, heating pad, massage, or a long hot shower can
help reduce pain.
The nutritional supplements glucosamine and chondroitin have been recommended as nutritional
supplements for people with osteoarthritis. But recent studies have been disappointing.
Ask your healthcare provider if they recommend any supplements for you. And always
discuss any alternative treatments or medicines you’d like to try.
When should I call my healthcare provider?
Spinal cord compression or cauda equina syndrome (compression of nerve bundle in lower
spine) is a medical emergency. Call your healthcare provider or go to the emergency
room if you have:
-
Sudden loss of bowel or bladder control
-
Severe or increasing numbness between your legs, inner thighs, or back of your legs
-
Severe pain and weakness that spreads into one or both legs, making it hard to walk
or get out of a chair
Key points about spinal cord compression
-
Spinal cord compression is caused by a condition that puts pressure on your spinal
cord.
-
Symptoms, such as pain, numbness, or weakness in the arms, hands, legs, or feet, can
come on gradually or more suddenly, depending on the cause.
-
Spinal cord compression can often be helped with medicines, physical therapy, or other
treatments. Except in emergencies, surgery is usually a last resort.
-
Keep your back healthy by living a healthy lifestyle. This includes staying at a healthy
weight, eating a well-balanced diet, not smoking, and getting regular physical activity.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells
you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments,
or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also
know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that
visit.
-
Know how you can contact your healthcare provider if you have questions.