Pediatric Neurocritical Care Fellowship

Director: Jake Deines, M.D.
(Pediatric Critical Care)
- Our comprehensive one-year, full time fellowship is New York State’s only pediatric neurocritical care training program.
- Our full-time pediatric neurointensivist works to provide advanced individualized training. Initially boarded in Pediatric Critical Care, Dr. Jake Deines is able to provide balanced expertise to fellows from various training backgrounds.
- The University of Rochester has a rich history of excellence in neurocritical care training that we draw on and expand with our pediatric training program.
- Fellows are an integral part of the clinical and educational success in the divisions of Pediatric Critical Care and Child Neurology. It is our highest aim to provide a supportive, rigorous and collaborative training environment for our fellows to achieve their goals.
Curriculum & Rotations
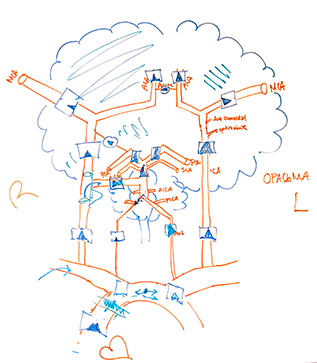
Fellows will develop expertise in the management of a diverse set of neurocritical illnesses including traumatic brain injury, seizure disorders and status epilepticus, stroke, hypoxic injuries and more.
 Core Curriculum
Core Curriculum
- Orientation – 2 weeks
- Pediatric Neurocritical Care Consult Service – 6 weeks
- Electrophysiology – 4 or 6 weeks (track dependent)
- Pediatric Neurosurgery – 6 weeks
- Adult Neuromedicine ICU – 10 or 12 weeks (track dependent)
- Neuroradiology – 2 weeks
- Neurovascular Service – 2 weeks
- Physical Medicine & Rehabilitation – 2 weeks
- Vacation – 4 weeks
- Pediatric Outpatient ICU Follow-up Clinic – 1 to 2 afternoons/month
Intensivist Track
Requires completion of a fellowship in Pediatric Critical Care
- Child Neurology Service – 6 weeks
- Adult Neurology Consult Service – 2 weeks
- Adult Stoke Service – 2 weeks
Child Neurologist Track
Requires completion of a residency in Child Neurology
- Pediatric Intensive Care Unit – 6 weeks
- Pediatric Cardiac Intensive Care Unit – 4 weeks
- Ultrasound/Vascular Access/Transport Teams – 2 weeks
- Pediatric Anesthesia – 2 weeks
 Didactic Curriculum
Didactic Curriculum
- Customized 2-week orientation schedule based on track. pNCC Fellowship specific orientation sessions and participation with Neurology Residency, Pediatric Critical Care and Adult Critical Care orientation
- Fellows will be invited to all didactic sessions with Pediatric Critical Care, Child Neurology and Adult Neurocritical care. Specific schedule will be based on fellow’s background and goals
- Monthly pNCC Fellowship specific teaching and administration sessions with program leadership
- Simulation sessions with a pediatric neurocritical care focus
- Opportunities for didactic teaching in multiple settings and learner groups including medical students, residents, fellows, nursing and transport teams
Research and Quality Improvement
- Fellow’s will be encouraged and mentored in their research or quality improvement efforts and can be involved in specific divisional projects based on individual interest. Ongoing multi-center projects include
- P-ICECAP Trial
- BOOST-3
- NEAR4KIDS
- Education in Pediatric Intensive Care (E.P.I.C.) Projects
- As this is a clinically focused fellowship, there is no research or QI project requirements
Program Goals
- Expertise in the diagnosis and management of the child with neurocritical illness
- Proficiency in clinical electrophysiology, including basic, long-term and intraoperative EEG
- Understand the modalities of pediatric neuroimaging, including advanced training in interpretation of neurologic CT and MRI
- Skill in management and real-time interpretation of invasive and non-invasive neuromonitoring techniques
- Exposure to pediatric and adult neurosurgical practice, including neurovascular procedures
- Robust experience in adult neurointensive care
- Appreciation for the role of the consulting pediatric neurointensivist in the neonatal, pediatric and cardiac intensive care populations
- Focus on inclusion, equity, interdisciplinary teamwork and evidence-based practice of pediatric neurocritical care
Application Instructions
- Applicants accepted with completion or anticipated graduation from ACGME-certified Pediatric Critical Care Fellowship, or Child Neurology Residency and anticipated eligibility or completion of respective subspecialty boards.
- Additionally, applicants must be U.S. citizens, permanent residents, or hold a J1 visa for consideration for fellowship training
- Email a current curriculum vitae, two letters of reference, and brief personal statement to our fellowship administrator, Vanessa Mace.
Our Team
- Jake Deines, M.D. (Pediatric Critical Care), Director
Supporting Faculty
- Debra Roberts, M.D., Ph.D. – Director of the Adult Neuromedicine ICU at Strong Memorial
- Howard Silberstein, M.D. – Pediatric Neurosurgery
- Inna Hughes, M.D., Ph.D. – Pediatric Epileptology
- Jeevek Almast, M.B.B.S. – Pediatric Neuroradiology
- Robert Stone, M.D. – Residency Director of Child Neurology
- Jill Cholette, M.D. – Pediatric Critical Care Chief
Former Fellows
 Travis Kauffmann, M.D.
Travis Kauffmann, M.D.
Dr. Travis Kauffmann earned his Bachelor's of Science in Biochemistry from North Carolina State University, Raleigh, NC. Expanding his horizons, he pursued a Master's in Public Health with a focus on Statistical Analysis and Human Resource Management. His academic journey led him to The Brody School of Medicine at East Carolina University, Greenville, NC, where he earned his medical degree.
Travis completed residency in Pediatrics at Le Bonheur Children's Hospital, University of Tennessee Health Sciences Center, Memphis, TN. His exceptional teaching skills were recognized by his peers and the student body, earning him The Golden Apple Teaching Award out of over 100 residents for the 2016-2017 academic year.
Upon completing his residency, he completed his Fellowship in Pediatric Critical Care Medicine at Nemours Children's Hospital, Wilmington, DE. It was there that he again won The Golden Apple Teaching Award, this time out of 67 fellows for the 2022-2023 academic year. His interest in vascular access led him to research “Complications of Transthoracic Intracardiac Lines versus PICC Lines in Post-Operative Management in a Pediatric CICU" under the guidance of Dr. Nicholas Kalbach.
Dr. Kauffmann's passion for Pediatric Neurocritical Care grew from his deep-rooted fascination with physiology, especially the marvel of consciousness and the wonders of neuroplasticity. He is excited to join the growing field of Pediatric Neurocritical Care, and even more excited to be doing his neuro year in Rochester New York, learning from such accomplished and nationally recognized teachers of Neurology.
Jacob Anderson, M.D.
Jacob received his Bachelors of Science in Biology at Utah Valley University and attended medical school at St George's University School of Medicine in Grenada. He completed his pediatric residency and chief residency at SUNY Upstate Medical University. He then completed his pediatric critical care fellowship at the University of Rochester while obtaining his M.S. in Health Professions Education with an emphasis on multi-modal learning theories and online curriculum development. Jacob developed a passion for neurocritical medicine during his PICU fellowship and is excited contribute to this growing academic field in pediatrics. His academic interests include status epilepticus, post-cardiac arrest care, TBI, cerebrovascular disorders, and transcranial doppler sonography.
Dr. Anderson accepted a position at University of Buffalo and Oshei Children’s Hospital as a pediatric intensivist, and will be building their Pediatric Neurocritical Care Program in Buffalo, NY.