News

20242023202220212020
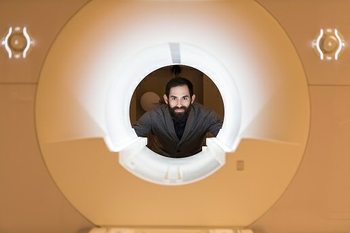
Researchers reveal how trauma changes the brain
Wednesday, December 7, 2022
 Exposure to trauma can be life-changing – and researchers are learning more about how traumatic events may physically change our brains. But these changes are not happening because of physical injury, rather our brain appears to rewire itself after these experiences. Understanding the mechanisms involved in these changes and how the brain learns about an environment and predicts threats and safety is a focus of the ZVR Lab at the Del Monte Institute for Neuroscience at the University of Rochester, which is led by assistant professor Benjamin Suarez- Jimenez, Ph.D.
Exposure to trauma can be life-changing – and researchers are learning more about how traumatic events may physically change our brains. But these changes are not happening because of physical injury, rather our brain appears to rewire itself after these experiences. Understanding the mechanisms involved in these changes and how the brain learns about an environment and predicts threats and safety is a focus of the ZVR Lab at the Del Monte Institute for Neuroscience at the University of Rochester, which is led by assistant professor Benjamin Suarez- Jimenez, Ph.D.
“We are learning more about how people exposed to trauma learn to distinguish between what is safe and what is not. Their brain is giving us insight into what might be going awry in specific mechanisms that are impacted by trauma exposure, especially when emotion is involved,” said Suarez-Jimenez, who began this work as a post-doctoral fellow in the lab of Yuval Neria, Ph.D., professor at Columbia University Irving Medical Center.
Their research, recently published in Communications Biology, identified changes in the salience network – a mechanism in the brain used for learning and survival – in people exposed to trauma (with and without psychopathologies, including PTSD, depression, and anxiety). Using fMRI, the researchers recorded activity in the brains of participants as they looked at different-sized circles – only one size was associated with a small shock (or threat). Along with the changes in the salience network, researchers found another difference – this one within the trauma-exposed resilient group. They found the brains of people exposed to trauma without psychopathologies were compensating for changes in their brain processes by engaging the executive control network – one of the dominate networks of the brain.
Read More: Researchers reveal how trauma changes the brainDr. Krystel Huxlin selected to Optica's 2023 fellows class
Tuesday, November 8, 2022
Krystel Huxlin was elected as a Fellow Member of Optica (formerly OSA) by Society’s Board of Directors.
Optica (formerly OSA) is dedicated to promoting the generation, application, archiving and dissemination of knowledge in optics and photonics worldwide. Founded in 1916, it is the leading organization for scientists, engineers, business professionals, students and others interested in the science of light. Optica’s renowned publications, meetings, online resources and in-person activities fuel discoveries, shape real-life applications and accelerate scientific, technical and educational achievement.
Fellow membership in Optica is limited to no more than ten percent of the membership and is reserved for members who have served with distinction in the advancement of optics and photonics.
Krystel is being honored specifically for innovative approaches to visual restoration, encompassing optics, ocular biology, laser tissue-interaction, and visual behavior.
Read More: Dr. Krystel Huxlin selected to Optica's 2023 fellows classKerry O’Banion recognized for national contributions to MD-PhD training
Thursday, November 3, 2022
Kerry O’Banion, director of the Medical Science Training Program at the School of Medicine and Dentistry and a professor of neuroscience, has received the 2022 MD-PHD National Association Dr. Bert Shapiro Award. The award recognizes an individual who has made significant contributions to physician-scientist training on the national level. O’Banion, who has been Rochester’s MSTP director since 2000, served as a member and chair of the MD-PhD Section of the Association of American Medical Colleges’ GREAT Group as well as of the National Institute of General Medicine Sciences’ TWD-A study section. He currently serves as an advisor for multiple MD-PhD programs nationwide. He is also a founding Board Member of the American Physician Scientists Association, a student-run organization that promotes careers for physician-scientists.
A serendipitous discovery and the choreographed dance of fragile X research
Tuesday, October 18, 2022
The choreography of development is a delicate dance. Beginning in utero, chromosomes, DNA, genes and RNA twirl, tap, and sashay their way in a precise pattern. A misstep or a missing step that changes the routine causes body and brain functions to go awry – as is the case with many intellectual and developmental disabilities (IDD). Fragile X syndrome is the most common known single-gene cause of inherited IDDs, including autism. Scientists know the misstep in this syndrome is in the gene FMR1. FMR1 is responsible for making the protein FMRP, which is necessary for typical brain development.
Lynne Maquat, Ph.D., founding director of the Center for RNA Biology at the University of Rochester, and professor of Biochemistry & Biophysics, Oncology, and Pediatrics, did not set out to study fragile X. It was through another line of research – her seminal discovery of and decades’ worth of work on nonsense-mediated mRNA decay (NMD) – that fragile X syndrome entered her radar. NMD is a cellular quality-control mechanism that plays a role in both healthy and disease states, and her lab discovered that it is overactive in people with fragile X.
“It was complete serendipity,” Maquat said. “No one ever thought to look at NMD and fragile X. So now we’re trying to figure out what happens at the molecular level when FMRP is absent; we want to understand the network of altered gene expression by identifying mis-regulated messenger RNAs (mRNAs).”
One of the most prominent surveillance systems in the body that protects against mistakes in gene expression that lead to disease, NMD is a complex pathway that is at the heart of many of the collaborations between Maquat and other University of Rochester scientists. Together, with funding from the National Institutes of Health (NIH) and the FRAXA Research Foundation, they aim to gain a deeper understanding of the sophisticated mechanisms related to NMD that will contribute to developing new drug therapies for genetic disorders such as fragile X syndrome, cystic fibrosis, and hundreds of others.
INTO THE BRAIN
Associate professor of Biomedical Genetics Christoph Pröschel, Ph.D., has spent much of his career interested in neurogenetic diseases that primarily affect the white matter of the brain, which carries signals throughout the organ. His lab started working with induced pluripotent stem cells (iPSCs) to understand different neural cell types, providing a solid foundation for their IDD research. “My lab and the Maquat lab have a mutual interest in the molecular mechanism of fragile X,” said Proschel. “It is key to finding any kind of hope for a future therapy.”
The Pröschel lab makes and differentiates neural stem cells that mimic fragile X syndrome, allowing his team to test hypotheses and understand how different therapies impact cell biology and function. He and Tatsuaki Kurosaki, Ph.D., research assistant professor in the Maquat lab, used these neural stem cells to understand the relationship between FMRP and NMD. They discovered that NMD controls the amounts of messenger RNAs deriving from a wide range of genes throughout the brain, including genes that govern motor control and cognitive processes related to attention, learning, and language. They also found that when FMRP is absent from cells, as it is in people with fragile X syndrome, NMD shifts into overdrive.
This work was part of a 2021 study published in Nature Cell Biology led by Maquat that revealed that tamping down NMD with small molecule inhibitors restored a large proportion of neurological functions in these cells.
Most recently, Pröschel co-authored research published in Molecular Cell led by Maquat and co-authored by Hana Cho, Ph.D., and Elizabeth Abshire, Ph.D., of her lab. The study highlighted a complex molecular dance between NMD and the enzyme AKT, which plays a key role in cell growth and survival. Both AKT and NMD are overactive in fragile X. Using neural stem cells that lack the FMRP protein, they tested a drug called Afuresertib, which inhibits AKT. They discovered that blocking AKT in the fragile X cells decreased its activity and decreased NMD. These cells then acted more like typical, non-disease cells.
There is still a lot the team doesn’t know about how AKT and NMD interact, because they both influence and regulate multiple activities in cells, but this work provides good direction that could inform the development of future treatments for fragile X syndrome.
“This has been one of the real fun chapters of my career – working with this group,” said Pröschel. “Everyone brings such a different perspective to the project.”
FROM SURGERY TO THE LAB
As a neurotologist (subspecialist of Otolaryngology), Hitomi Sakano, M.D., Ph.D., spends time in the clinic with patients with hearing issues or hearing loss. In the lab, she aims to understand how the brain adapts to sound information.
Her work with fragile X syndrome began as a resident at the University of Washington when she took interest in FMRP, which is highly expressed in the auditory brainstem nuclei of a typical brain and is the same protein missing in fragile X patients. When Sakano came to the Medical Center in 2018, she brought the fragile X mouse model to study this and joined the Center for RNA Biology.
“I also use the [knockout] mouse model to study hyperacusis – extreme sensitivity to sound,” said Sakano. “We know that fragile X patients have sensory and auditory sensitivity, so this model is a great tool to study both.” Hyperacusis is also very common in the general population (some report up to 15 percent) so understanding the mechanism could potentially impact our broader community.
Sakano hypothesizes that FMRP regulates genes that enable neuroplasticity to maintain
From left: Hitomi Sakano, M.D., Ph.D., and Lynne Maquat, Ph.D.
normal processing of auditory information. If true, there may be therapeutic targets for symptoms like auditory hypersensitivity in fragile X. Funding from the Schmitt Program in Integrative Neuroscience (SPIN) through the Del Monte Institute for Neuroscience Pilot Program and a NIH Research Career Development Award for clinician-scientists are supporting her research, which involves investigating the gene expression abnormalities in the auditory brainstem of the fragile X mouse model that might explain the auditory hypersensitivity in these mice. To date, she has found some interesting RNAs that encode synaptic proteins. These findings open up the possibility of targeting these genes for the treatment of hyperacusis.
She co-authored a study with the Maquat and Pröschel labs in Genome Biology. The research used the mouse model whose FMR1 gene is knocked-out. These findings build upon Maquat’s previous research that showed NMD hyperactivation in neuronally induced stem cells from fragile X patients. This hyperactivity negatively impacts many neuronal mRNAs important to brain development. The Genome Biology paper showed NMD goes into overdrive in the brain during early development in a mouse with fragile X. These researchers are now testing various therapeutics to inhibit NMD.
“Being able to collaborate to gain meaningful results to move this science forward is the value of being at an academic medical center like Rochester,” said Sakano. “These steps are what will ultimately lead to treatments and therapies that I use in the clinic someday to help my patients.”
ON THE HORIZON
Forthcoming research aims to broaden the scope of the fragile X work at the Medical Center. One of the world’s largest clinics for fragile X is in Israel, where an estimated 80 percent of women are screened for the inherited disease. Michael Telias, Ph.D., assistant professor of Ophthalmology, Neuroscience, and Center for Visual Science, began studying fragile X as a graduate student in Israel. He uses human embryonic stem cells that carry the mutation for fragile X to look inside neurons at the molecular and cellular levels to shed light on the human-specific mechanisms affected by this syndrome.
“Human neurons have shown us that these cells have a problem receiving information and communicating information to the next cell,” said Telias. “We cannot do this work in humans, so using human cells enables us to know what to target in the cell. That is the only way we will be able to develop treatments that work.”
In the Frederick J. and Marion A. Schindler Cognitive Neurophysiology Laboratory, research assistant professor Tufikameni Brima, Ph.D., is aiming to use electroencephalography (EEG) and event-related potentials (ERP) to better understand how the brains of patients with fragile X respond to various stimuli. This work has the potential to build upon the ongoing molecular research being conducted by Telias and others.
“Ultimately, what we are figuring out is what happens when FMRP is absent. We don’t know the whole story,” Maquat said. “However, FMRP is an RNA-binding protein, and in work soon to be published in Molecular Cell, Kurosaki and I have now defined those messenger RNAs that are normally bound by FMRP and how the absence of FMRP binding results in those mRNAs making too much protein. These results have allowed us to identify which genes are affected and how. Our work will pave the way for better therapeutics for those living with fragile X.”
Read More: A serendipitous discovery and the choreographed dance of fragile X researchThe prose of Dr. Seuss shines a light on how the brain processes speech
Wednesday, September 21, 2022
Researchers at the Del Monte Institute for Neuroscience have expanded the understanding of how the brain is engaged during complex audiovisual speech perception.
The study now out in NeuroImage, describes how listening and watching a narrator tell a story activates an extensive network of brain regions involved in sensory processing, multisensory integration, and cognitive functions associated with the comprehension of the story content. Understanding the involvement of this larger network has the potential to give researchers new ways to investigate neurodevelopmental disorders.

Lars Ross, Ph.D.
“Multisensory integration is an important function of our nervous system as it can substantially enhance our ability to detect and identify objects in our environment,” said Lars Ross, Ph.D., research assistant professor of Imaging Sciences and Neuroscience and first author of the study. “A failure of this function may lead to a sensory environment that is perceived as overwhelming and can cause a person to have difficulty adapting to their surroundings, a problem we believe underlies symptoms of some neurodevelopmental disorders such as autism.”
Using fMRI, researchers examined the brain activity of 53 participants as they watched a video recording of a speaker reading “The Lorax.” How the story was presented would change randomly in one of four ways – audio only, visual only, synchronized audiovisual, or unsynchronized audiovisual. Researchers also monitored the participants’ eye movements. They found that along with the previously identified sites of multisensory integration, viewing the speaker’s facial movements also enhanced brain activity in the broader semantic network and extralinguistic regions not usually associated with multisensory integration, such as the amygdala and primary visual cortex. Researchers also found activity in thalamic brain regions which are known to be very early stages at which sensory information from our eyes and ears interact.
“This suggests many regions beyond multisensory integration play a role in how the brain processes complex multisensory speech – including those associated with extralinguistic perceptual and cognitive processing,” said Ross.
Expanding the Research to Children
Researchers designed this experiment with children in mind, according to the investigators who have already begun working with both children and adults on the autism spectrum in an effort to gain insight into how their ability to process audiovisual speech develops over time.

John Foxe, Ph.D.
“Our lab is profoundly interested in this network because it goes awry in a number of neurodevelopmental disorders,” said John Foxe, Ph.D., lead author of this study. “Now
that we have designed this detailed map of the multisensory speech integration network, we can ask much more pointed questions about multisensory speech in neurodevelopmental disorders, like autism and dyslexia, and get at the specific brain circuits that might be impacted.”
Additional co-authors include Sophie Molholm, Ph.D., and Victor Bene of Albert Einstein College of Medicine, and John Butler, Ph.D., of Technological University Dublin. This research was a collaboration of two Intellectual and Developmental Disability Research Centers (IDDRC), which are supported by the National Institute of Child Health and Human Development (NICHD). In 2020, the University of Rochester was designated as an IDDRC by the NICHD. The award recognized the Medical Center’s national leadership in research for conditions such as autism, Batten disease, and Rett syndrome. Molholm is the co-director of the Rose F. Kennedy IDDRC at Einstein.
Congratulations to NGP members recognized at Convocation '22
Wednesday, September 14, 2022
The following NGP members are being recognized for a total of 7 awards:
- Andrea Campbell - URSMD Meliora Scholarship
- Mariah Marrero - Irving L. Spar Fellowship Award
- Tanique McDonald - J. Newell Stannard Scholarship Award
- Michael Lim - Merritt and Marjorie Cleveland Fellowship
- Emily Przysinda - Outstanding Student Mentor Award
- Brian Redmond - Graduate Student Award for Excellence in Equity & Inclusion
- Rianne Stowell - Outstanding Postdoc Mentor Award
We are incredibly proud of our honorees and recognition of their accomplishments. Please congratulate these award winners and be sure to provide a few high fives if you see them in the hallway.
Mild traumatic brain injury increases risk of behavioral and emotional problems in kids
Tuesday, September 13, 2022
University of Rochester researchers have been at the forefront of efforts to understand how blows to the head impact the brain, including how concussions change brain structure . Now researchers at the Del Monte Institute for Neuroscience have found that kids who experience a traumatic brain injury (TBI), even a mild one, have more emotional and behavioral problems than kids who do not.
 “These hits to the head are hard to study because much of it depends on recall of an injury since the impacts do not all require a visit to a doctor,” said Daniel Lopez, a Ph.D. candidate in the Epidemiology program and first author of the study out today in NeuroImage. "But being able to analyze longitudinal data from a large cohort and ask important questions like this gives us valuable information into how a TBI, even a mild one, impacts a developing brain."
“These hits to the head are hard to study because much of it depends on recall of an injury since the impacts do not all require a visit to a doctor,” said Daniel Lopez, a Ph.D. candidate in the Epidemiology program and first author of the study out today in NeuroImage. "But being able to analyze longitudinal data from a large cohort and ask important questions like this gives us valuable information into how a TBI, even a mild one, impacts a developing brain."
Researchers used MRI and behavioral data collected from thousands of children who participated in the Adolescence Brain Cognitive Development (ABCD) Study. They revealed children with a mild TBI experienced a 15-percent increased risk of an emotional or behavioral problem. The risk was the highest in children around ten years old. Researchers found that children who had a significant hit to the head but did not meet diagnostic criteria for a mild TBI also had an increased risk of these behavioral and emotional problems.
The University of Rochester Medical Center is one of 21 research sites collecting data for the National Institutes of Health ABCD Study. Since 2017, 340 children from the greater Rochester area have been part of the 10-year study that is following 11,750 children through early adulthood. It looks at how biological development, behaviors, and experiences impact brain maturation and other aspects of their lives, including academic achievement, social development, and overall health.
 Researchers hope future ABCD Study data will better reveal the impact these head hits have on mental health and psychiatric problems. “We know some of the brain regions associated with increased risk of mental health problems are impacted during a TBI,” said Ed Freedman, Ph.D., associate professor of Neuroscience and co-principal investigator of the ABCD Study at the University of Rochester. Freedman also led this study. “With more time and data, we hope to gain a better understanding of the long-term impact of even a mild TBI.”
Researchers hope future ABCD Study data will better reveal the impact these head hits have on mental health and psychiatric problems. “We know some of the brain regions associated with increased risk of mental health problems are impacted during a TBI,” said Ed Freedman, Ph.D., associate professor of Neuroscience and co-principal investigator of the ABCD Study at the University of Rochester. Freedman also led this study. “With more time and data, we hope to gain a better understanding of the long-term impact of even a mild TBI.”
Additional co-authors include Zachary Christensen, John J. Foxe, Ph.D., Laura Ziemer, and Paige Nicklas, all members of the Frederick J. and Marion A Schindler Cognitive Neurophysiology Lab that is part of the Del Monte Institute for Neuroscience at the University of Rochester. The research was supported by the National Institute on Drug Abuse, and the UR Intellectual and Developmental Disabilities Research Center.
Ross Maddox receives the National Science Foundation's Faculty Early Career Development (CAREER) Award
Thursday, September 1, 2022
The CAREER awards recognize role models in research, education and provides recipients five years of funding to help lay the foundation for their future research. Ross's research will explain how our brain stems help us listen and converse in noisy settings.
 Hearing one voice among many
Hearing one voice among many
After sound waves are converted into electrical signals in the ear, the signals are conveyed along an auditory brainstem to the brain’s cortex, where auditory perception occurs. But scientists are still trying to understand exactly how this “beautiful, but complicated network of connections” helps us focus our listening, says Maddox.
For example, do the downward connections that extend from the cortex back along the auditory brainstem help us concentrate on one voice among many?
To help answer questions like these, Maddox will use new methods to measure auditory brainstem responses in human subjects engaged in goal-oriented, lifelike tasks involving natural speech—not the rapid bursts of clicks and other stimuli used in traditional testing.
The results could help explain why even people with normal hearing sometimes struggle to understand conversations amid background noise
Read More: Ross Maddox receives the National Science Foundation's Faculty Early Career Development (CAREER) AwardNew Grant Will Unlock Workings of Glymphatic System
Monday, August 15, 2022
A decade ago, researchers in the lab of Maiken Nedergaard, M.D., D.M.Sc., answered a basic question of biology that up to that point had eluded scientists: how is waste removed from the brain? The discovery of what is now known as the glymphatic system and subsequent research have transformed the way we study a range of neurological disorders and critical brain functions. A new $15 million grant from the National Institutes of Health (NIH) will bring together several teams of researchers to accelerate our understanding of the complex mechanics that control this system, with an eye toward the development of new therapies for diseases like Alzheimer’s.
The new research program will be led by Nedergaard, co-director of the Center for Translational Neuromedicine, and involve scientists and engineers from the University of Rochester, Penn State University, Boston University, and the University of Copenhagen. The research is being funded through The BRAIN Initiative, a massive research program supported by NIH and several other federal research agencies that aims to fill gaps in our current knowledge of the brain’s organization and function.
The glymphatic system – a network of plumbing that runs parallel to blood vessels and pumps cerebral spinal fluid (CSF) through brain tissue to wash away waste – was all but invisible to the scientific world until 2012 when it was first described in a study published in Science Translational Medicine. A paper in the journal Science a year later showed that this system operates primarily while we sleep and removes toxic proteins associated with Alzheimer’s disease. These findings fundamentally changed scientists’ understanding of the biological purpose of sleep and opened the door to potential new ways to treat neurological disorders.
Read More: New Grant Will Unlock Workings of Glymphatic SystemLiz Romanski publishes new paper in Neuroscience
Thursday, June 23, 2022
New research led by Dr. Lizabeth Romanski confirms a role for the primate ventrolateral prefrontal cortex in the social communication network.
In the recent paper in Neuroscience, "Representation of Expression and Identity by Ventral Prefrontal Neurons”, Neuroscience (2022), together with former Neuroscience Graduate Student Dr. Maria Diehl, and former Research Professor Dr. Bethany Plakke, the investigators found that during working memory, single prefrontal neurons encode the identity and/or the expression of the face and vocal information that is remembered.
The work is cited in a separate commentary in the same issue, Neuroscience (2022).
Walking gives the brain a ‘step-up’ in function for some
Friday, June 17, 2022
It has long been thought that when walking is combined with a task – both suffer. Researchers at the Del Monte Institute for Neuroscience at the University of Rochester found that this is not always the case. Some young and healthy people improve performance on cognitive tasks while walking by changing the use of neural resources. However, this does not necessarily mean you should work on a big assignment while walking off that cake from the night before.
“There was no predictor of who would fall into which category before we tested them, we initially thought that everyone would respond similarly,” said Eleni Patelaki, a biomedical engineering Ph.D. student at the University of Rochester School of Medicine and Dentistry in the Frederick J. and Marion A. Schindler Cognitive Neurophysiology Laboratory and first author of the study out now in Cerebral Cortex. “It was surprising that for some of the subjects it was easier for them to do dual-tasking – do more than one task – compared to single-tasking – doing each task separately. This was interesting and unexpected because most studies in the field show that the more tasks that we have to do concurrently the lower our performance gets.”
Improving means changes in the brain
Using the Mobile Brain/Body Imaging system, or MoBI, researchers monitored the brain activity, kinematics and behavior of 26 healthy 18 to 30-year-olds as they looked at a series of images, either while sitting on a chair or walking on a treadmill. Participants were instructed to click a button each time the image changed. If the same image appeared back-to-back participants were asked to not click.
Read More: Walking gives the brain a ‘step-up’ in function for someHow the brain interprets motion while in motion
Monday, June 13, 2022
New findings about how the brain interprets sensory information may have applications for treating brain disorders and designing artificial intelligence.
Imagine you’re sitting on a train. You look out the window and see another train on an adjacent track that appears to be moving. But, has your train stopped while the other train is moving, or are you moving while the other train is stopped?
The same sensory experience—viewing a train—can yield two very different perceptions, leading you to feel either a sensation of yourself in motion or a sensation of being stationary while an object moves around you.
Human brains are constantly faced with such ambiguous sensory inputs. In order to resolve the ambiguity and correctly perceive the world, our brains employ a process known as causal inference.
Causal inference is a key to learning, reasoning, and decision making, but researchers currently know little about the neurons involved in the process.
In a new paper published in the journal eLife, researchers at the University of Rochester, including Greg DeAngelis, the George Eastman Professor of Brain and Cognitive Sciences, and his colleagues at Sungkyunkwan University and New York University, describe a novel neural mechanism involved in causal inference that helps the brain detect object motion during self-motion.
2022 University Research Award Recipients
Friday, June 3, 2022
Congratulations to several members of Neuroscience that have recieved University research awards for 2022.
University Research Awards provide seed money to help launch particularly innovative projects that would likely attract external funding once they are sufficiently developed. An award of up to $37,500 is made as a match to funds committed by the applicant’s home school (or applicants’ home schools) for a total of $75,000.
Congratulations Manuel Gomez-Ramirez, Kuan Wang, Edmund Lalor, and Brian Keane!
Read More: 2022 University Research Award RecipientsDr. Fiebelkorn named a Searle Scholar for 2022
Wednesday, May 25, 2022
Searle Scholars Program names 15 scientists as Searle Scholars for 2022
Members of the new class of Searle Scholars pursue ground-breaking research in chemistry and the biomedical sciences. Each receives an award of $300,000 in flexible funding to support his, her, or their work over the next three years.
The Searle Scholars Program makes grants to selected universities and research centers to support the independent research of exceptional young faculty in the biomedical sciences and chemistry who have recently been appointed as assistant professors on a tenure-track appointment. The Program’s Scientific Director appoints an Advisory Board of eminent scientists who choose the Scholars based on rigorous standards aimed at finding the most creative talent interested in pursuing an academic research career. This year, 186 applications were considered from nominations by 176 universities and research institutions.
Congratulations Dr. Fiebelkorn!
Read More: Dr. Fiebelkorn named a Searle Scholar for 2022Major Grant Funds Research to Understand Key Features of OCD: Inflexibility and Avoidance
Tuesday, May 24, 2022

With $15.6 million from the National Institute of Mental Health, scientists will investigate the brain networks central to obsessive compulsive disorder in order to guide the development of effective treatments. A team of scientists from across the country will use a $15.6 million award from the National Institute of Mental Health to investigate the brain networks central to obsessive compulsive disorder (OCD). The work will build on more than 15 years of research by lead investigator Suzanne N. Haber, Ph.D. and collaborators to understand the underlying biology of the disease and guide the development of effective treatments.
“Obsessive compulsive disorder is among the most disabling psychiatric disorders,” said Haber, professor of Pharmacology and Physiology, Neuroscience and Psychiatry at the University of Rochester School of Medicine and Dentistry. “It affects one to three percent of the population worldwide, yet it hasn’t received the same level of attention as other mental health disorders. We’re excited to receive this funding and use translational methods to understand circuit dysfunction in the disease and to develop new treatment approaches that can improve the lives of patients.”
The five-year grant funds a Silvio O. Conte Center for Basic and Translational Mental Health Research at the University of Rochester. Haber has received previous Conte Center grants that have propelled scientists’ understanding of the disease. Major findings include the discovery of a narrower, more defined network of brain regions that underlie the disorder. Dubbed the ‘OCD network,’ the new grant will allow scientists to test the idea that behavioral inflexibility in OCD results from faulty connections between brain circuits in this network.
Read More: Major Grant Funds Research to Understand Key Features of OCD: Inflexibility and AvoidanceCongratulations to Krystal Huxlin
Friday, April 29, 2022
Congratulations to Krystal Huxlin! She has been elected by the Vision Sciences Society membership to serve on the VSS Board of Directors.
Her four-year term will begin in May 2022.
Diverse minds and determined hearts make change: Forging equitability in Neuroscience
Monday, April 25, 2022
A group, mostly consisting of neuroscientists, meets bi-weekly outside the lab with a simple but powerful common purpose – to fundamentally change the bench.
“This experience has been eye-opening,” said Manuel Gomez-Ramirez, Ph.D., assistant professor of Brain and Cognitive Sciences at the University of Rochester and chair of the Del Monte Institute for Neuroscience Diversity Commission. “It is such a diverse group in every sense – cultural, gender, experience in both academics and non-academics – we are all able to have input and listen to each other while considering different perspectives and focusing on one problem together.”
In 2020, the Neuroscience Diversity Commission (NDC) was formed following a letter penned by the director of the Del Monte Institute, John Foxe, Ph.D., in response to the death of George Floyd.
Read More: Diverse minds and determined hearts make change: Forging equitability in NeuroscienceNew research finds the risk of psychotic-like experiences can start in childhood
Monday, April 25, 2022
 It has long been understood that environmental and socio-economic factors – including income disparity, family poverty, and air pollution – increase a person’s risk of developing psychotic-like experiences, such as subtle hallucinations and delusions that can become precursors to a schizophrenia diagnosis later in life. Research has long focused on young adults but now, thanks to data from the Adolescent Brain Cognitive Development (ABCD) Study, researchers at the University of Rochester have found these risk factors can be observed in pre-adolescent children.
It has long been understood that environmental and socio-economic factors – including income disparity, family poverty, and air pollution – increase a person’s risk of developing psychotic-like experiences, such as subtle hallucinations and delusions that can become precursors to a schizophrenia diagnosis later in life. Research has long focused on young adults but now, thanks to data from the Adolescent Brain Cognitive Development (ABCD) Study, researchers at the University of Rochester have found these risk factors can be observed in pre-adolescent children.
“These findings could have a major impact on public health initiatives to reduce the risk of psychotic-like experiences,” said Abhishek Saxena, a graduate student in the department of Psychology at the University of Rochester and first author of the study recently published in Frontiers in Psychiatry. “Past research has largely focused on the biological factors that lead to development of schizophrenia spectrum disorders, but we now know that social and environmental factors can also play a large role in the risk and development of schizophrenia. And this research shows these factors impact people starting at a very young age.”
Researchers looked at data collected from 8,000 kids enrolled in the ABCD study. They found that the more urban of an environment a child lived in – proximity to roads, houses with lead paint risks, families in poverty, and income disparity – the greater number of psychotic-like experiences they had over a year’s time. These findings are in line with past research conducted in young adults, but have not been found like this in pre-adolescences.
“It is disconcerting that the association between these exposures and psychotic-like experiences are already present in late childhood,” said David Dodell-Feder, Ph.D., assistant professor of Psychology and Neuroscience and lead author of this study. “The fact that the impact of these exposures may occur as early as pre-adolescence highlights the importance of early prevention.”
This research was supported by the National Institute of Mental Health.
The University of Rochester Medical Center is one of 21 research sites across the country collecting data for the National Institutes of Health ABCD Study. Since 2017, 340 children from the greater Rochester area have been participating in the 10-year study. In all, the study is following 11,750 children through early adulthood looking at how biological development, behaviors, and experiences impact brain maturation and other aspects of their lives, including academic achievement, social development, and overall health.
The art of smell: Research suggests the brain processes smell both like a painting and a symphony
Monday, April 4, 2022
What happens when we smell a rose? How does our brain process the essence of its fragrance? Is it like a painting – a snapshot of the flickering activity of cells – captured in a moment in time? Or like a symphony, an evolving ensemble of different cells working together to capture the scent? New research suggests that our brain does both.
“These findings reveal a core principle of the nervous system, flexibility in the kinds of calculations the brain makes to represent aspects of the sensory world,” said Krishnan Padmanabhan, Ph.D., an associate professor of Neuroscience and senior author of the study recently published in Cell Reports. “Our work provides scientists with new tools to quantify and interpret the patterns of activity of the brain.”
Researchers developed a model to simulate the workings of the early olfactory system – the network the brain relies on for smelling. Employing computer simulations, they found a specific set of connections, called centrifugal fibers, which carry impulses from other parts of the central nervous system to the early sensory regions of the brain, played a critical role. These centrifugal fibers act as a switch, toggling between different strategies to efficiently represent smells. When the centrifugal fibers were in one state, the cells in the piriform cortex – where the perception of an odor forms – relied on the pattern of activity within a given instant in time. When the centrifugal fibers were in the other state, the cells in the piriform cortex improved both the accuracy and the speed with which cells detected and classified the smell by relying on the patterns of brain activity across time.
Read More: The art of smell: Research suggests the brain processes smell both like a painting and a symphonyA key to restoring sight may be held in a drug that treats alcoholism
Friday, March 18, 2022

 Researchers may have found a way to revive some vision loss caused by age-related macular degeneration – the leading cause of blindness – and the inherited disease retinitis pigmentosa (RP), a rare genetic disorder that causes the breakdown and loss of cells in the retina. The drug disulfiram – marketed under the brand name Antabuse – used to treat alcoholism, may hold the key to restoring this vision loss.
Researchers may have found a way to revive some vision loss caused by age-related macular degeneration – the leading cause of blindness – and the inherited disease retinitis pigmentosa (RP), a rare genetic disorder that causes the breakdown and loss of cells in the retina. The drug disulfiram – marketed under the brand name Antabuse – used to treat alcoholism, may hold the key to restoring this vision loss.
“We knew the pathway that the drug disulfiram blocks to treat alcoholism was very similar to the pathway that’s hyper-activated in degenerative blindness,” said Michael Telias, Ph.D., assistant professor of Ophthalmology, Neuroscience, and Center for Visual Science at the University of Rochester Medical Center, and first author on the paper out today in Science Advances. “We expected some improvement, but our findings surpassed our expectations. We saw vision that had been lost over a long period of time preserved in those who received the treatment.”
Read More: A key to restoring sight may be held in a drug that treats alcoholismNew methods to understand how the brain responds to sounds, including singing
Wednesday, February 23, 2022
New research has identified neurons in the brain that ‘light up’ to the sound of singing, but do not respond to any other type of music. Assistant Professor of Neuroscience and Biostatistics and Computational Biology Samuel Norman-Haignere, Ph.D., with the Del Monte Institute for Neuroscience at the University of Rochester is first author on the paper in Current Biology that details these findings. “The work provides evidence for relatively fine-grained segregation of function within the auditory cortex, in a way that aligns with an intuitive distinction within music,” Norman-Haignere said.
The singing-specific area of the brain is located in the temporal lobe, near regions that are selective for speech and music. Researchers worked with epilepsy patients who had electrodes implanted in their brain (electrocorticography or ECOG) in order to localize seizure-related activity as a part of their clinical care. ECoG enables more precise measurements of electrical activity in the brain. “This higher precision made it possible to pinpoint this subpopulation of neurons that responds to song. This finding along with prior findings from our group give a bird’s eye view of the organization of the human auditory cortex and suggest that there are different neural populations that selectively respond to particular categories, including speech, music, and singing.”
In previous research, fMRI was used to scan the brains of participants as they listened to different types of speech and music. Norman-Haignere combined the fMRI data from this prior study in order to map the locations of song-selective neural populations, which were identified in their new ECoG study.
Read More: New methods to understand how the brain responds to sounds, including singingSarah Latchney, PhD: Teaching to Learn
Thursday, February 17, 2022
Sarah Latchney, Ph.D., is right where she had hoped to be: teaching science at a small, public, liberal arts college.
In the summer of 2019, she was hired as faculty at St. Mary’s College of Maryland. As an assistant professor of Biology and Neuroscience, she predominately teaches introductory-level biology for all incoming Biology and Neuroscience students as well as several introductory and advanced courses in the Neurosciences.
Latchney says she caught the teaching bug after designing and teaching a 200-level undergraduate course in toxicology as part of her training in the Rochester Postdoc Partnership (RPP) program.
“It was a course that I developed from scratch on my own,” Latchney recalls. “Through that experience, I learned what it truly means to teach at the college level – to be the sole instructor of record and everything that goes into designing a course, implementing it, and interacting with students. It was a lot of work but also lots of fun.”
Read More: Sarah Latchney, PhD: Teaching to LearnResearchers find new clues in the brain linking pain and food
Friday, February 11, 2022
It has long been known that there is an association between food and pain, as people with chronic pain often struggle with their weight. Researchers at the Del Monte Institute for Neuroscience may have found an explanation in a new study that suggests that circuitry in the brain responsible for motivation and pleasure is impacted when someone experiences pain. “These findings may reveal new physiological mechanisms linking chronic pain to a change in someone’s eating behavior,” said Paul Geha, M.D., lead author on the study published in PLOS ONE. “And this change can lead to the development of obesity.”
Finding pleasure in food comes from how our brain responds to what we are eating. In this study researchers were looking at the brain’s response to sugar and fat. Using a gelatin dessert and pudding researchers altered the sugar, fat, and texture of the foods. They found that none of the patients experienced eating behavior changes with sugar, but they did with fat. Those with acute lower back pain who later recovered were most likely to lose pleasure in eating the pudding and show disrupted satiety signals – the communication from the digestive system to the brain – while those with acute lower back pain whose pain persisted at one year did not initially have the same change in their eating behavior. But chronic lower back pain patients did report that eventually foods high in fat and carbohydrates, like ice cream and cookies, became problematic for them over time and brain scans showed disrupted satiety signals.
Read More: Researchers find new clues in the brain linking pain and foodDorsey: Telemedicine Can Narrow Health Inequities
Wednesday, February 9, 2022
Last week, URMC neurologist Ray Dorsey, M.D., testified before a Congressional subcommittee on how technologies like telemedicine can help to break down barriers to care for people with disabilities. The hearing is part of a legislative initiative under way by the U.S. House Ways and Means Committee, which seeks to understand and address “the role that racism, ableism, and other social, structural, and political determinants have in perpetuating health and economic inequity in the U.S.”
Read More: Dorsey: Telemedicine Can Narrow Health InequitiesRebecca Lowery Study Suggests Way to Restore Brain Immune System Function After Prenatal Exposure to Environmental Toxin
Tuesday, February 8, 2022
New research shows that exposure to the industrial byproduct TCDD in utero could cause the brain’s immune system to go array later in life, damaging important brain circuits, and potentially giving rise to neurodevelopmental disorders, such as autism and ADHD. TCDD is primarily released into the environment by vehicle exhaust and burning wood and low levels of the toxin are found in air, soil, and food. The most common way people are exposed is through meat, dairy, and fish.
In the same study, recently published in the journal Brain, Behavior, and Immunity, researchers also found that pharmacological manipulation could restore the function of microglia, important cells in the brain’s immune system. “This suggests that defects in microglia function resulting from prenatal exposures can be reversed later in life, indicating a possible additional therapeutic avenue for neurodevelopmental disorders,” said Rebecca Lowery, Ph.D., assistant research professor in the Del Monte Institute for Neuroscience at the University of Rochester, and co-first author of the study.
Read More: Rebecca Lowery Study Suggests Way to Restore Brain Immune System Function After Prenatal Exposure to Environmental ToxinResearchers provide insight into how the brain multitasks while walking
Monday, January 24, 2022
The associate professor of Neuroscience and his Del Monte Institute colleagues published a study in NeuroImage that provides evidence of how the brain takes on multiple tasks without sacrificing how either activity is accomplished. "Looking at these findings to understand how a young, healthy brain is able to switch tasks will give us better insight to what's going awry in a brain with a neurodegenerative disease like Alzheimer's disease," Freedman says.
Read More: Researchers provide insight into how the brain multitasks while walkingBenjamin Suarez-Jimenez authors study: Research finds anxiety cues in brain even in safe environment
Monday, January 3, 2022
A team of researchers used virtual reality to understand the impact anxiety has on the brain and how brain regions interact with one another to shape behaviour.
The study has been published in the ‘Communications Biology Journal’. “These findings tell us that anxiety disorders might be more than a lack of awareness of the environment or ignorance of safety, but rather that individuals suffering from an anxiety disorder cannot control their feelings and behavior even if they wanted to,” said Benjamin Suarez-Jimenez, Ph.D., assistant professor in the Del Monte Institute for Neuroscience at the University of Rochester and first author of the study.
“The patients with an anxiety disorder could rationally say — I’m in a safe space — but we found their brain was behaving as if it was not,” he added.
Using fMRI, the researchers observed the brain activity of volunteers with general and social anxiety as they navigated a virtual reality game of picking flowers. Half of the meadow had flowers without bees, the other half had flowers with bees that would sting them — as simulated by a mild electrical stimulation to the hand. Researchers found all study participants could distinguish between the safe and dangerous areas, however, brain scans revealed volunteers with anxiety had increased insula and dorsomedial prefrontal cortex activation — indicating that their brain was associating a known safe area to danger or threat.
“This is the first time we’ve looked at discrimination learning in this way. We know what brain areas to look at, but this is the first time we show this concert of activity in such a complex ‘real-world-like’ environment,” said Suarez-Jimenez.
“These findings point towards the need for treatments that focus on helping patients take back control of their body,” he added.
The brain differences were the only differences seen in these patients. For example, sweat responses, a proxy for anxiety, which was also measured, failed to reveal any clear differences.
Understanding the neural mechanisms by which the brain learned about the environment is the focus of Suarez-Jimenez’s research, particularly how the brain predicted what is threatening and what is safe. He used virtual reality environments to investigate neural signatures of anxiety disorders and post-traumatic stress disorder (PTSD). His goal is to understand how people build maps in the brain that are based on experience, and the role of those maps in psychopathologies of stress and anxiety.
“For next steps in this recent research, we still need to clarify if what we found in the brain of these patients is also the case in other disorders, such as PTSD. Understanding the differences and similarities across disorders characterized by deficits in behavioral regulation and feelings in safe environments, can help us create better personalized treatment options,” he said.