Curriculum
The clinical curriculum is progressive with a focus on graduated autonomy from year one through year three spanning general to subspecialty care and outpatient to inpatient/intensive care settings. Residents experience both the university-based, tertiary/quaternary Golisano Children’s Hospital and the community-based Rochester General Hospital. We utilize X+Y scheduling with 2-week block rotations for 6 weeks followed by 2 weeks of outpatient experiences. Educational resources for all rotations are available to residents at any time through our Blackboard site. We use a night float system to cover the general floors and intensive care units so we do not have any 24-hour shifts.
Sample Intern Schedule by Block
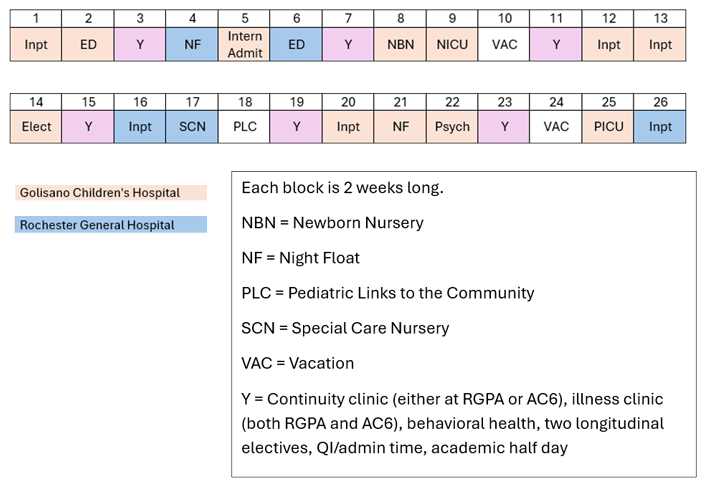
Intern Year
Rotations include:
- Inpatient pediatrics including general and subspecialty services
- Newborn and special care nurseries
- Neonatal and pediatric intensive care units
- Outpatient pediatrics
- Emergency medicine
- Mental health
- Community health and advocacy (Pediatric Links with the Community)
- Subspecialty/elective rotations
- Y Blocks: continuity clinic, general pediatrics including acute illness, mental health, subspecialties, outpatient academic half day, QI/admistrative time
Second Year
This training year incorporates progressive supervisory responsibility of interns and medical students as well as a more individualized curriculum including track options and increased elective time.
Rotations include:
- Neonatal and pediatric intensive care units
- Inpatient pediatrics
- Outpatient pediatrics
- Adolescent medicine
- Developmental and behavioral pediatrics
- Subspecialty/elective rotations including track blocks
- Y Blocks: continuity clinic, general pediatrics, adolescent medicine, subspecialties, outpatient academic half day, skills sessions, track time
Third Year
The third-year resident has increased autonomy and supervisory responsibilities and spends time in the following rotations:
- Inpatient pediatrics including Pediatric Admitting Officer (PAO)
- Newborn and special care nurseries
- Outpatient pediatrics
- Emergency medicine
- Subspecialty/elective rotations including track blocks
- Y Blocks: continuity clinic, acute illness, mental health, subspecialties, outpatient academic half day, QI/administrative time, track time
Unique Required Experiences
- Pediatric Links with the Community (PLC): A two-week rotation in which interns learn first-hand about critical factors affecting child health, while interacting with medical and non-medical providers at various community-based organizations and programs.
- Intern Admit: An inpatient experience focused on completing pediatric admissions to develop proficiency in the admission process and to foster clinical reasoning and management.
- Skills Sessions During Y Block: Second-year residents learn and practice skills in the following areas:
- Clinical: NICU and PICU simulations, splinting, bedside skills, procedural training, difficult conversations, de-escalation techniques, and lactation & breastfeeding
- Personal and Professional: safe space training, career options and planning, financial literacy, and QI project planning
- Pediatric Admitting Officer (PAO): In this role, third-year residents are responsible for (1) triaging all admissions to the children's hospital; (2) accepting admissions on behalf of Pediatric Hospital Medicine; (3) admitting, delegating, or supervising pediatric admissions; and (4) leading the management of acute patient events by responding to all rapid responses, behavioral emergencies, and pediatric codes.