Biventricular Assist Device Implantation
What is a biventricular assist device?
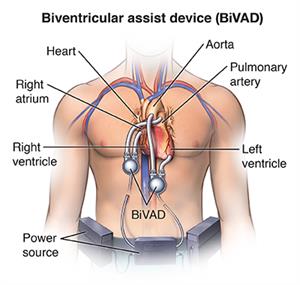
A biventricular assist device (BiVAD) is an implantable pump. It is designed to help
your heart function better when both the right and left pumping chambers of your heart
are failing.
When blood from your body returns to the right side of your heart, the right ventricle
(one of the pumping chambers) pumps the blood into your lungs to receive oxygen. The
oxygen-rich blood then goes back to the left side of your heart. Here your left ventricle
pumps blood out through the main artery leaving your heart.
A person may need a device to help pumping blood from both the right ventricle into
the lungs and the left ventricle out to the body under extreme circumstances. There
are 2 main types of ventricular assist devices: a left ventricular assist device and
a right ventricular assist device. When used in combination, they are called a BiVAD.
A BiVAD is a battery-operated pump that helps both your right and left ventricles
move blood through your heart. Your surgeon implants a BiVAD during open-heart surgery.
Why might I need a biventricular assist device?
You may need a BiVAD if you are in severe heart failure. Heart failure means your
heart is too weak to work normally. A BiVAD may be needed:
-
To keep your heart working during or after heart surgery until you recover
-
To keep your heart working while you wait for a heart transplant
-
As a lifelong (permanent) treatment for heart failure
What are the risks of biventricular assist device implantation?
BiVAD surgery is major surgery. You will need general anesthesia to put you to sleep.
Any general anesthesia has the risk of heart or brain injury. There is even more of
a risk if you have heart failure. Major surgery also increases the risk of blood clots
forming during or after surgery. These clots can break free and travel to your lungs
(pulmonary embolism) or your brain (stroke). They can block blood flow where the clot
becomes lodged. Other risks of this surgery include:
-
Infection
-
Bleeding
-
Device failure or device malfunction
-
Abnormal heart rhythm (arrhythmia)
-
Infection in your heart tissue (endocarditis)
-
Damage to the kidneys (renal failure)
There may be other risks, depending on your specific health problem. Discuss any concerns
with your healthcare provider before the procedure.
How do I get ready for biventricular assist device implantation?
Before surgery, your medical and surgical team will evaluate you. You will likely
have X-rays, blood tests, and procedures to check the health of your lungs and heart.
Your healthcare team will also do a heart test called an echocardiogram (echo) and
cardiac catheterization. An echocardiogram is an ultrasound that uses sound waves
to make images of your heart.
Cardiac catheterization is used to look at circulation through the arteries in the
heart muscle. It also measures how much pressure is inside the heart chambers and
the lungs.
Other preparation may include:
-
Your healthcare provider will explain the procedure to you and ask you if you have
any questions.
-
You will be asked to sign a consent form that gives your permission to do the procedure.
Read the form carefully and ask questions if something is not clear.
-
Follow all directions you are given for not eating or drinking before the surgery.
-
If you are pregnant or think that you may be pregnant, tell your provider
-
Tell your provider if you are sensitive to or are allergic to any medicines, iodine,
latex, tape, or anesthesia (local and general).
-
Tell your provider about all prescription and over-the-counter medicines, vitamins,
and herbal supplements you are taking.
-
Tell your provider if you have a history of bleeding disorders or if you are taking
any blood-thinning (anticoagulant) medicines, aspirin, or other medicines that affect
blood clotting. You may need to stop some or all of these medicines before the procedure.
-
Your provider may ask you to have a blood test before the procedure to find out how
long it takes your blood to clot.
-
Stop smoking as soon as possible before the procedure. This may improve your chances
for a successful recovery from surgery. It will also help your overall health.
Your provider may give you other instructions for getting ready based on your condition.
What happens during biventricular assist device implantation?
The surgery may take between 4 and 6 hours. Here is how the surgery usually proceeds:
-
You will be asked to remove any jewelry or other objects that may interfere with the
procedure.
-
You will be asked to remove your clothing and will be given a gown to wear.
-
You will be asked to empty your bladder before the procedure.
-
An IV (intravenous) line will be started in your arm or hand. Other catheters may
be inserted in your neck and wrist to keep track of your heart and blood pressure.
They can also be used for taking blood samples. Other sites for these catheters include
under the collarbone area and the groin.
-
You will be put on the operating table, lying on your back.
-
The anesthesiologist will give you some medicine to help you relax and fall asleep.
They will keep track of your heart rate, blood pressure, breathing, and blood oxygen
level during the surgery. A breathing tube will be put through your throat into your
lungs once you are sedated. You will be connected to a breathing machine (ventilator).
It will breathe for you during the surgery.
-
The skin over the surgical site will be cleansed with an antiseptic solution.
-
The surgeon will make a cut (incision) in the front of your chest, down through your
chest wall to reach your heart. They will put tubes into your heart. This is so a
cardiopulmonary machine can keep your blood moving during the surgery.
-
The surgeon will put a tube into your right atrium or ventricle. The tube is attached
to a pump. Another tube from the pump will be attached to your pulmonary artery. The
pump will circulate blood in the right side of your heart to get oxygen. This will
occur through the pump and out the pulmonary artery to your lungs.
-
For the left side of your heart, your surgeon will put a tube into your left ventricle
and attach it to a second pump. They will then connect another outflow tube to the
pump and attach it to your aorta. This pump will circulate blood in the left side
of your heart. This will occur through the pump and out the aorta to the rest of your
body.
-
With inflow and outflow tubes for each side of your heart attached to their own pump,
your surgeon will implant the 2 pumps either inside your upper belly or on the outside
of your skin.
-
A cable that comes out through your skin connects the pumps to a power source and
a system controller that you will wear on the outside of your body.
-
The pumps will be turned on to restore blood flow through your heart, lungs, and aorta.
This is done after all the attachments have been completed.
-
Once the procedure has been completed, the blood circulating through the bypass machine
will be allowed to reenter your heart and the tubes to the bypass machine will be
removed.
-
The incisions will be closed with stitches (sutures) or surgical staples.
-
Tubes will be inserted into your chest to drain blood and other fluids from around
the heart. These tubes will be connected to a suction device to drain fluids away
from the heart.
-
A tube will be inserted through your mouth or nose into your stomach to drain stomach
fluids.
-
A sterile bandage or dressing will be applied to the incisions.
What happens after biventricular assist device implantation?
In the hospital
The length of time you stay in the hospital will depend on your overall condition
after surgery.
-
For the first few days, you will be in intensive care (ICU). You will be watched closely
until your vital signs have stabilized.
-
The tubes that give you nourishment, help you breathe, and drain fluids from your
body will gradually be removed as you recover.
-
You may have temporary pacing wires that are placed during the surgery. These wires
will be removed once your heart rhythm is stable and you no longer need them.
-
Physical rehabilitation (cardiac rehab or physical therapy) and pulmonary rehabilitation
are important for your long-term recovery. You will begin a step-wise program of increasing
time and intensity of activity. This is to get you ready to go home.
-
You will be given an incentive spirometer device to use often. This is to help expand
your lungs and prevent pneumonia after the surgery.
Caregivers will help you care for your incision, provide pain relief, and get you
up walking.
You will be taught how to care for the BiVAD before you leave the hospital. You will
learn how it works and what to do if its alarm goes off, or there is a power loss.
You will also learn how to travel with your BiVAD. And to keep your battery and controller
dry when you bathe.
At home
You will be discharged home once your healthcare providers feel that you have recovered
enough . Follow all your instructions for medicines, pain control, diet, activity,
bathing, and wound care. Make sure to keep all of your follow-up appointments. Make
sure to keep in close contact with your transplant center if you are waiting for a
heart transplant.
Other common instructions after surgery include:
-
Walk every day, or as advised by your provider.
-
Don't do any heavy lifting.
-
Slowly go back to normal activities as much as possible (ask your provider about driving,
working, and sexual activity). You may be asked not to drive a car for a time after
the surgery. This is to allow for healing of the breastbone (sternum) and muscles
of the chest wall.
-
Check your wounds for any sign of swelling, redness, bleeding, or discharge. Report
these to your medical and surgical team.
-
Let your provider know about any increasing pain, fever, chest pain, or shortness
of breath.
-
Eat a heart-healthy diet and maintain a healthy weight. Eat foods that are low in
salt, cholesterol, and fat. Try to eat fruits, vegetables, and lean meats.
-
Don't smoke and stay away from secondhand smoke. Don't use any tobacco products, including
electronic cigarettes.
Next steps
Before you agree to the test or procedure make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure