News
Marijuana Permissiveness
Tuesday, September 15, 2015
In a study carried out by RTI researchers and presented at the PAINWeek meeting, which also used NSDUH data from 2002 to 2012, showed that the culture around marijuana permissiveness might influence legalization. The study found that states that passed marijuana legislation had higher marijuana use rates 5 years before and in the last data year available before legalization compared with states that did not legalize marijuana. The authors noted that of the 23 states with medical marijuana laws, 5 have passed legislation that allows for the possession and recreational use of marijuana among those aged 21 years and older.
Commenting on this research for Medscape Medical News, Armando Villarreal, MD, assistant professor, neurosurgery, Rochester Neurosurgical Partners, New York, said that while the data seem to suggest that culture around permissiveness might affect legislation, other factors play a role a role in establishing that culture. "Among them are the unemployment rate, the median level of education, religion, and political ideals," he said. Less than half of all states have passed medical marijuana laws, and only 10% of the states now allow recreational use.
"So the idea that we are about to see a sudden influx of states that will legalize marijuana seems to me overreaching." Dr Villarreal, who gave a separate presentation on "the science behind marijuana as an analgesic" at the meeting, said physicians should become familiar with local laws surrounding use of marijuana because their patients will ask their opinion. But he stressed that prescribing marijuana should be influenced only by available scientific data and not by public opinion.
"Currently the data is scant, mainly due to federal government laws that make it extremely difficult to do good research. I believe there is an urgent need to change these laws so that better information regarding the therapeutic use of marijuana becomes available."
Patients Prefer Relief from Lower Back Pain Over Improved Mobility
Friday, September 11, 2015
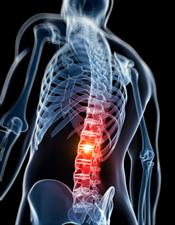
A new study out today in the journal Neurology examines the question of quality of life for individuals with a common form of lower back pain called lumbar spinal stenosis. The findings show that, when asked to choose between treatments that reduced pain or would help them stand or walk, patients overwhelmingly chose pain relief.
There has long been a debate in the medical community over striking the right balance between pain relief and physical function,
said John Markman, M.D., director of the Translational Pain Research Program in the University of Rochester Department of Neurosurgery and lead author of the study. While physicians have leaned toward the need to increase mobility, this study shows that patients have a clear preference for pain relief.
UR Medicine Honored for Stroke Care
Friday, July 24, 2015

UR Medicine’s Strong Memorial Hospital has received the American Heart Association/American Stroke Association’s (AHA/ASA) highest award for stroke care, including a new designation that recognizes excellence in rapid care that can save lives and improve the quality of life of stroke victims.
In stroke care, time equals brain,
said Curtis Benesch, M.D., medical director of the UR Medicine’s Comprehensive Stroke Center. This award recognizes the discipline and training that is required to provide appropriate and timely care to stroke patients and our team strives each and every day to provide the most comprehensive, cutting-edge care for patients from across upstate New York.
This award reflects the commitment of our team to providing the highest level of care possible for our patients who’ve suffered a stroke,
said Babak Jahromi, M.D., surgical director of the Comprehensive Stroke Center. The outstanding group of nurses, therapists, and physicians that we have assembled are dedicated to this common goal.
Strong has been named a Get With The Guidelines Stroke Gold Plus Achievement Award with Target: Stroke Honor Roll Elite Plus. The award recognizes the hospitals commitment and success ensuring that stroke patients received the most appropriate treatment according to nationally recognized, research-based guidelines based on the latest scientific evidence.
To receive the Gold Plus Quality Achievement Award, hospitals must achieve 85 percent or higher adherence to all Get With The Guidelines-Stroke achievement indicators for two or more consecutive 12-month periods and achieved 75 percent or higher compliance with five of eight Get With The Guidelines-Stroke Quality measures.
VasoMark advances to the next phase!
Tuesday, March 10, 2015

The VasoMark Team
A group of students from Neuroscience Graduate Program and Neurosurgery Residency Program have teamed up to compete
in the
National Institutes of Health
Neuro Startup Challenge
.
This new effort offers pre- and post-doctoral students from biomedical, legal, and business backgrounds the
opportunity to compete for licenses
to patented technologies from the NIH portfolio.
The teams model a business around the intellectual property, and seek startup funding from partnering angel investor and venture capitalist firms in order to bring the proposed technology to the biomedical marketplace. The NGP and Neurosurgery team, named VasoMark, selected two patents for the development of a minimally invasive diagnostic for the detection of primary and recurrent malignant brain tumors. VasoMark successfully completed Phase I of the competition, where they developed a two-minute elevator pitch and executive summary describing their intended entrepreneurial use of the selected technology. They are currently developing a business plan and live investor pitch describing their business model, intended market, and future areas of expansion for their selected patents.
Neuromedicine Intensive Care Unit Team Wins Award for Excellence
Thursday, January 29, 2015

URMC Board Chair George Hamlin presided over the recognition of the 2014 Excellence Award Winners at the Board meeting on Jan. 20. The awards, presented annually, laud the extraordinary efforts of our physicians, nurses, clinicians, and support staff. This year individuals and teams in 13 categories were recognized. Among them was the Neuromedicine Intensive Care Unit.
Implementation of nurse-led daily rounds is making a significant impact on patient care thanks to the Board Excellence Award-winning team, the Neuromedicine Intensive Care Unit. Introduced by Manjunath Markandaya, M.D., and created by nurse Catherine Gargan, RN, CNRN, the switch from physician-led rounds in the Neuromedicine ICU seemed like a natural transition. This change puts nurses, who are front-line caregivers, with the most up-to-date information on their patients in the lead during rounding. The nurse presents the patient to the residents, fellows, and physicians who are involved and often includes the pharmacist, respiratory therapist, and dietitian as well. Families are also welcome on rounds and they are grateful to be part of the process where they learn more about the care of loved ones and have an opportunity to ask questions of the entire care team. Rounds are more efficient under this new team approach and satisfaction scores for this critical care setting are higher.
The team was nominated by Associate Director of Adult Critical Care Nursing Kate Valcin and nurse leader LaShaunda Bradley. The departments of Neurology and Neurosurgery would like to extend their congratulations on this well-deserved award!
UR Medicine Opens Doors on New NeuroMedicine ICU
Monday, July 28, 2014
UR Medicine today unveiled a new state-of-the-art unit dedicated to highly specialized care for people with serious and life-threatening neurological conditions, like strokes, seizures, brain and spinal tumors, and traumatic brain injury. The Neuromedicine Intensive Care Unit (ICU), which is the only unit of its kind in the region, is located on the eighth floor of Strong Memorial Hospital.
The $5.5 million, 5,500-square-foot unit consists of 12 beds and is staffed around the clock by an extended multidisciplinary team trained to treat the most challenging and difficult neurological disorders. The neurocritical care team members include neurointensivists, neurologists, neurosurgeons, physician assistants, nurse practitioners, critical care nurses, anesthesiologists, respiratory therapists, social workers, physical therapists, speech-language pathologists, occupational therapists, nutritionists, and clinical pharmacologists.
Diseases and injuries that impact the brain and central nervous system have a unique set of challenges and require expertise that is not commonly found in a traditional ICU setting. While brain function must be continuously monitored, providers also need to be trained to recognize that these conditions can potentially lead to other problems, such as cardiovascular, kidney, and respiratory complications or infections, particularly if a patient remains in an ICU setting for a long period of time. Also, once a patient has been stabilized, there must be continuity of care as they begin the process of recovery and transition to rehabilitation.
Neurology and Neurosurgery Ranked Again as One of Best in Nation
Friday, July 18, 2014
For a second consecutive year, the departments of Neurology and Neurosurgery have been ranked in the top 50 in US News & World Report's 2015 Best Hospitals guidebook.
Under the leadership and guidance of Chairs Holloway and Pilcher, Neurology and Neurosurgery were ranked as the 49th best.
URMC's success in the U.S. News rankings reflects the hard work that our faculty and
staff have invested to continuously improve quality, patient safety and satisfaction. It also reflects
URMC's growing reputation for first-rate care,
said URMC CEO Bradford C. Berk, M.D., Ph.D.
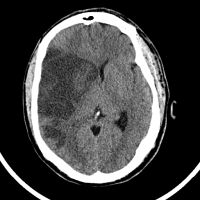
Model Sheds New Light on Sports-related Brain Injuries
Tuesday, April 29, 2014
A new study has provided insight into the behavioral damage caused by repeated blows to the head. The research provides a foundation for scientists to better understand and potentially develop new ways to detect and prevent the repetitive sports injuries that can lead to the condition known as chronic traumatic encephalopathy (CTE).
The research – which appears online this week in the Journal of Neurotrauma – shows that mice with mild, repetitive traumatic brain injury (TBI) develop many of the same behavioral problems, such as difficultly sleeping, memory problems, depression, judgment and risk-taking issues, that have been associated with the condition in humans.
“This new model captures both the clinical aspects of repetitive mild TBI and CTE,” said Anthony L. Petraglia, M.D., a neurosurgeon with the University of Rochester School of Medicine and Dentistry and lead author of the study. While public awareness of the long-term health risk of blows to the head is growing rapidly, our ability to scientifically study the fundamental neurological impact of mild brain injuries has lagged.
Heart/Stroke Association Honors UR Medicine for Highest Quality Care
Tuesday, April 22, 2014
The American Heart Association/American Stroke Association (AHA/ASA) has once again recognized UR Medicine and its Strong Memorial Hospital for achieving its highest standards of care for stroke, heart failure, and resuscitation.
Strong Memorial Hospital has received the AHA/ASA Get With The Guidelines program’s highest honor, the Stroke Gold Plus Quality Achievement Award for a fifth consecutive year. The hospital was also tapped for the Target: Stroke Honor Roll, which recognizes hospitals that have consistently and successfully reduced door-to-needle time – the window of time between a stroke victim’s arrival at the hospital, the diagnosis of an acute ischemic stroke, and the administration of the clot-busting drug tPA.
“We are proud to earn this recognition, however we continue to work to improve time-to-treatment for people who are suffering a stroke. Early treatment is proven to preserve brain function and enhance recovery for each patient,” said neurologist Curtis Benesch, M.D., M.P.H., medical director of the UR Medicine Comprehensive Stroke Center.
UR Medicine Helps Forge National Stroke Care Guidelines
Friday, March 28, 2014

A new statement from the American Heart Association (AHA) recommends that people recovering from a severe stroke receive tailored and coordinated care that optimizes quality of life and minimizes suffering. The statement -- which was published today in the journal Stroke -- represents the first attempt to establish a fundamental set of recommendations that can help guide physicians, patients, and their families through the difficult decisions that arise from this condition.
The majority of stroke patients require access to some form of palliative care,
said Robert Holloway, M.D., M.P.H., the chair of the Department of Neurology at the University of Rochester School of Medicine and Dentistry. Accomplishing this requires that a hospital's system of stroke care and its team of providers place the patient and their family at the center of the decision-making process and build a plan of care that is based on their values and informed by effective and constant communication.
Stroke Survivors Deserve Team Care
Thursday, March 27, 2014
Palliative care that minimizes suffering and improves quality of life should be provided to patients who've survived a stroke, experts say. The care should be a team effort involving patients, families, stroke specialists and health care providers such as neurosurgeons, neurologists, primary care doctors, nurses and therapists, according to the new scientific statement from the American Heart Association (AHA) and American Stroke Association (ASA).
The majority of stroke patients need access to some form of palliative medicine,
statement lead author Dr. Robert Holloway, chairman of the neurology department at the University of Rochester Medical Center in Rochester,
N.Y., said in an AHA/ASA news release.
The stroke team and its members can manage many of the palliative care problems themselves. It encourages
patient independence and informed choices,
he explained.
UR Medicine Recognized for Stroke Care, Launches Neurocritical Care Program
Tuesday, February 4, 2014
Strong Memorial Hospital has been recognized by The Joint Commission and the American Heart Association/American Stroke Association as a Comprehensive Stroke Center. This designation, which has only been conferred on two other hospitals in New York State, places Strong among an elite group of institutions that provide highly-specialized complex stroke care.
"We are proud that the Joint Commission has recognized our dedicated team of neurologists, neurosurgeons, radiologists, emergency department physicians, nurses, therapists, and staff," said neurologist Curtis Benesch, M.D., M.P.H., the medical director of the URMC Stroke and Cerebrovascular Center. This certification is a testament to their commitment to provide the highest and most comprehensive level of stroke care to our community.
URMC Plays Role in New Epilepsy Technology
Monday, December 2, 2013
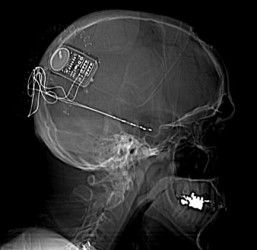
Physicians at the University of Rochester Medical Center (URMC) Strong Epilepsy Center were involved in the recent approval of a new treatment for epilepsy. The implantable medical device - called the Responsive Neurostimulator System (RNS) - monitors brain activity and can detect and counteract seizures.
URMC was one of only 28 sites in the country to conduct clinical trials of RNS, which was developed by the California-based company Neuropace. The research showed that the device decreases the number of monthly seizures by nearly 38 percent. URMC neurologists Michel Berg, M.D. and James Fessler, M.D., and neurosurgeon Web Pilcher, M.D., Ph.D. were involved in the study.
This is the first FDA-approved brain implant for epilepsy that responds to the brain's activity,
said Berg, an associate professor of Neurology. For patients who are unable to control their seizures with medications or are not eligible for resective surgery, this device could provide an important treatment option.
Copper Identified as Culprit in Alzheimer's Disease
Monday, August 19, 2013
Copper appears to be one of the main environmental factors that trigger the onset and enhance the progression of Alzheimer's disease by preventing the clearance and accelerating the accumulation of toxic proteins in the brain. That is the conclusion of a study appearing today in the journal Proceedings of the National Academy of Sciences.
It is clear that, over time, copper's cumulative effect is to impair the systems by which amyloid beta is removed from the brain,
said Rashid Deane, Ph.D., a research professor in the University of Rochester Medical Center Department of Neurosurgery, member of the Center for Translational Neuromedicine, and the lead author of the study. This impairment is one of the key factors that cause the protein to accumulate in the brain and form the plaques that are the hallmark of Alzheimer's disease.
Neurology and Neurosurgery Ranked as One of Best in Nation
Tuesday, July 16, 2013

Chair of Neurology, Robert Holloway, Jr., M.D., M.P.H. and Chair of Neurosurgery, Webster H. Pilcher, M.D., Ph.D.
When US News & World Report's 2014 Best Hospitals guidebook hits newsstands today, a record number of six University of Rochester Medical Center specialties will be ranked among the very best in the nation. That's the highest number of URMC programs ever to earn a seat in the magazine's list of the nation's top 50 in a single year, since US News began ranking hospitals in 1989.
The URMC adult specialties nationally ranked included Neurology and Neurosurgery as the 29th best. URMC's success in the U.S. News rankings reflects the hard work that our faculty and staff have invested to continuously improve quality, patient safety and satisfaction. It also reflects URMC's growing reputation for first-rate care,
said URMC CEO Bradford C. Berk, M.D., Ph.D.
3 Events Offer Hope for People with Brain Tumors
Thursday, April 16, 2009
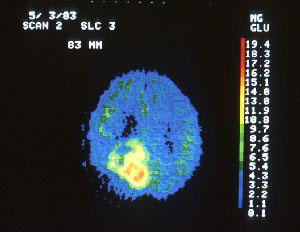
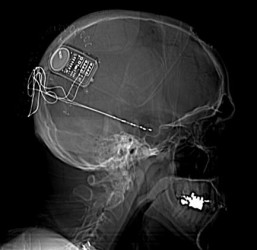
A PET scan allows doctors to see a brain tumor in an elderly man.
People with brain tumors, and those who love and care for them, will observe Brain Tumor Awareness Week with three educational and celebratory events sponsored by the University of Rochester Medical Center and James P. Wilmot Cancer Center.
On Friday, May 1, there will be a seminar for patients, their families, and physicians that focuses on the latest research and treatment approaches in brain and spinal tumors. Then on Thursday, May 7, patients, families and clinicians will gather for the Community Sharing Hope Picnic at Kings Bend Park in Pittsford. And on Saturday, May 9, there will be an education and supportive program for caregivers.
Each year, approximately 500 people with brain tumors are treated at the Medical Center and Wilmot Cancer Center, making it the largest program in the region. The events are offered by the Program for Brain and Spinal Tumors at the Medical Center and the Wilmot Cancer Center.
Rochester Scientist Wins Major Award for Alzheimer’s Research
Wednesday, April 15, 2009
A Rochester researcher whose work has opened up a whole new avenue in Alzheimer’s disease research has received a major prize from the American Academy of Neurology.
Berislav Zlokovic, M.D., Ph.D., director of the Center for Neurodegenerative and Vascular Brain Disorders at the University of Rochester Medical Center, will receive the 2009 Potamkin Prize for Research in Pick’s, Alzheimer's, and Related Diseases during the AAN annual meeting later this month in Seattle.
Zlokovic will split the $100,000 prize with two other researchers, Michael Wolfe, Ph.D., of Brigham and Women’s Hospital and Harvard Medical School, and Robert Vassar, Ph.D., of Feinberg School of Medicine at Northwestern University. The prize, which honors researchers for their work on Alzheimer’s disease and related disorders, will go toward the investigators’ Alzheimer’s research.
Abnormal EKG Can Predict Death in Stroke Patients
Friday, March 20, 2009
People who suffer an ischemic stroke and also have an abnormality in the heart’s electrical cycle are at a higher risk of death within 90 days than people who do not have abnormal electrical activity at the time of emergency treatment, according to new research.
The study also provides a threshold at which the threat of death is highest: QTc intervals greater than 440 milliseconds in women and 438 milliseconds in men have the worst prognosis. The findings are published online March 20, 2009, in the Journal of Stroke and Cerebrovascular Diseases.
Weighing the Options after Life-Altering Stroke
Thursday, March 12, 2009
Choosing to have aggressive brain surgery after suffering a severe stroke generally improves the patients' lives and allows them to live longer, according to research by neurologists at the University of Rochester Medical Center.
The findings should help patients and families put into perspective a decision that is nearly always painful and difficult to make – whether putting a patient through aggressive surgery after a catastrophic stroke is worth it.
For families facing this difficult choice, the more information we can provide, the better for their decision-making,
said neurologist Adam G. Kelly, M.D., who has helped hundreds of families chart a course after severe stroke. Kelly presented the findings last month at the International Stroke Conference in San Diego.
Out of Iraq Emerges Hope for Those with the Severest of Head Injuries
Wednesday, September 24, 2008
There may be more hope than has been recognized for some people with severe brain injuries, according to a U.S. neurosurgeon who earlier this year spent four months in Iraq treating soldiers and civilians. Jason Huang, M.D., this week presented his results from his experience in Iraq at the annual meeting of the Congress of Neurological Surgeons in Orlando, Fla.
Huang discussed blast injuries, a type of wound that has affected thousands of U.S. soldiers and others in Iraq. The term includes injuries caused by roadside bombs or improvised explosive devices (IEDs
), as well as car bombs, suicide bombs, and other blasts.
This is a type of injury unlike anything seen regularly here in the United States,
said Huang, an assistant professor of Neurosurgery at the University of Rochester Medical Center who is also a major in the U.S. Army Reserve.
Here we might see gunshot wounds to the head, or severe injuries from motor vehicle accidents, but we don't see blast injuries, and so neurosurgeons haven't really had much experience treating them. What we're seeing in Iraq is different even from injuries suffered by soldiers in previous wars. The extent of the blast injuries was far worse than I ever would have imagined,
Huang said.
Study of New Epilepsy Treatment Underway at URMC
Saturday, September 15, 2007
The University of Rochester Medical Center is participating in a multi-center study of a new medical device to treat epilepsy. The Rochester study is being overseen by neurologists Michel Berg, M.D. and James Fessler, M.D., and neurosurgeons Web Pilcher, M.D., Ph.D. and Jason Schwalb, M.D.
Uncontrolled seizures related to epilepsy are generally treated with medications,
said Berg, medical director of the Strong Epilepsy Center. However, many individuals treated with medication alone continue to experience seizures or have unacceptable medication side effects. If these patients are not candidates for epilepsy surgery, then options to effectively control their seizures are limited.
Study of New Epilepsy Treatment Underway at URMC
Friday, September 14, 2007
The University of Rochester Medical Center is participating in a multi-center study of a new medical device to treat epilepsy. The Rochester study is being overseen by neurologists Michel Berg, M.D. and James Fessler, M.D., and neurosurgeons Web Pilcher, M.D., Ph.D. and Jason Schwalb, M.D.
Uncontrolled seizures related to epilepsy are generally treated with medications,
said Berg, medical director of the Strong Epilepsy Center. However, many individuals treated with medication alone continue to experience seizures or have unacceptable medication side effects. If these patients are not candidates for epilepsy surgery, then options to effectively control their seizures are limited.
The Responsive Neurostimulator System (RNS) is an implantable device that is designed to suppress seizures in patients with epilepsy before any symptoms appear, much like implantable cardiac pacemakers are intended to detect abnormal heart rhythms and then deliver electrical stimulation to correct them. Neuropace, the California-based developer and manufacturer of the RNS system, is funding the trial. URMC is one of 28 centers across the country testing the new technology.