McMurray Named Associate Director of Pathology Graduate Program
Helene McMurray, Ph.D., has been named the new associate director of the Cell Biology of Disease (Pathology) Graduate Program at the University of Rochester, which became effective in March.
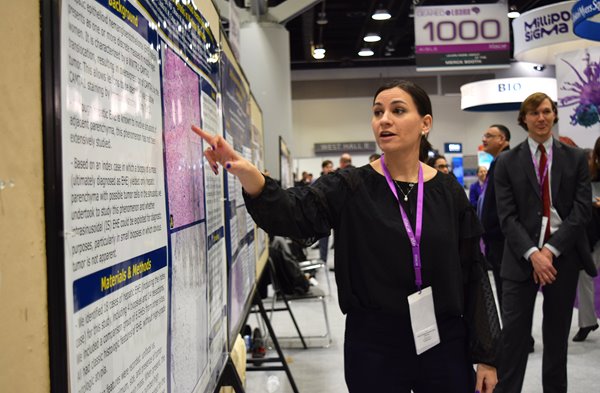
USCAP 2018 Meeting Recap
The Department of Pathology and Laboratory Medicine at URMC was well represented at the annual meeting of the U.S. and Canadian Academy of Pathology (USCAP) in Vancouver, BC, Canada March 17-23.
URMC Pathology Welcomes 2018 Residents and Fellows
The University of Rochester Medical Center's Pathology Residency Program is pleased to announce its new class of residents, starting July 1, 2018.
Catch URMC at the USCAP 2018 Meeting
Members of the University of Rochester Medical Center’s Department of Pathology & Laboratory Medicine will present abstracts at the 2018 meeting of the United States and Canadian Academy of Pathology (USCAP). The meeting will be held March 17-23 in Vancouver, BC, Canada.
Below is a schedule of events that include URMC faculty and residents. We are pleased to again host a cocktail reception for alumni and friends at the conference on Monday, March 19 (details below).
After Maria: Rebuilding Continues in Dominica
Nearly five months have passed since Hurricane Maria struck the island of Dominica, yet most of its residents still can’t turn their lights on.