Sports Medicine
Make Appointments & Get Care
What is Sports Medicine?
UR Medicine Sports Medicine offers the latest in medical and surgical care to prevent, evaluate, treat, and rehabilitate injuries for both recreational and competitive athletes of all ages.
Our team also helps people with active jobs who suffer the same type of injuries and need the same care, and those who simply want to exercise and move better.

World-class Care
Our Saunders Center for Orthopaedics & Physical Performance, located at Marketplace Mall, combines the latest in care, research and education under one roof to create a center unlike any other in the Northeast.
Schedule an appointment with a provider.
Call (585) 275-5321UR Medicine's Approach
We work closely with you to decide which treatment options are right for you. Using advanced testing procedures to understand the full extent of your injury, we can decide which approach will have the best outcome for you:
- Conservative treatments: Rest, medication, and physical therapy are often the most effective ways to treat an injury.
- Injection therapy: Some injuries respond well to medication applied directly at the point of injury. Our doctors use ultrasound to guide them to the exact right spot.
- Minimally invasive surgery: Using a tiny camera and light slipped through a small incision, our surgeons can see inside your injured joint. They watch their progress on a big screen while they repair torn tendons and ligaments, reshape bones, or remove bone spurs or fragments of cartilage.
- Complex surgery: When a major injury requires it, our surgeons use the most advanced techniques to repair and rebuild bones and joints or replace joints.
UR Medicine Orthopaedics & Physical Performance offers preventative treatment to make sure you won’t reinjure yourself. We also provide many specialty programs to help you perform better in your sport or activity while avoiding common injuries.
What Sets Us Apart?
Our injury prevention programs help people of all ages develop safer habits, whether in organized sports, recreational sports, or while exercising. Many injuries are preventable when adjusting inadequate physical conditioning, poor technique, or over-training or over-playing in a single sport.
UR Medicine is a proud participant in the Stop Sports Injury Campaign to help keep kids in the game for life, targeting the sports that have the highest rates of overuse and trauma injuries.
We also offer Fitness Science, a research-based program to help people optimize their performance. Doctors and experts who have treated and trained every level of athlete developed Fitness Science around strength training, nutrition, sport psychology, and data analysis.
Other sports-specific efforts include concussion injury prevention, a running clinic, ACL and spine injury prevention, and more.
Because of our expertise, we're the official sports medicine provider for athletes from most of the area high schools, and we’re the preferred providers for athletes from many local colleges and professional teams.
of 3
-
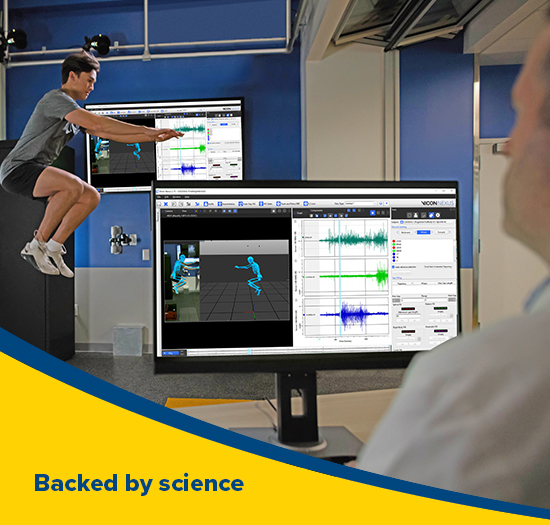
Image: Our new Motion Labs use computer and sensor technology to study, analyze, and enhance human motion. Learn how our labs are improving the diagnosis and treatment for patients with mobility restrictions, recovering from injury, or those looking to improve and enhance their athletic performance.
-

Image: Take your game to the next level with our integrative approach to sports performance. Through strength training, nutritional counseling, sports psychology and data analysis we help players of all ages train smarter and move better.
-

Image: With many convenient locations both in Rochester and the region, access to expert orthopaedic care and rehabilitation is closer than ever. Explore the many places we see patients and the exceptional providers at our affiliate hospitals.
Locations
View All LocationsWe serve you in the Rochester metropolitan area and surrounding region.
View All Locations5 locations
South Pointe Landing
10 South Pointe Landing, Suite 100
Rochester, NY 14626
Platinum Office Complex
2064 Fairport Nine Mile Point Road, Suite 100
Penfield, NY 14526
Strong West Annex, Building D
156 West Avenue
Brockport, NY 14420
St. James Hospital
7309 Seneca Road North, Suite 107
Hornell, NY 14843
Marketplace
10 Miracle Mile Drive
Rochester, NY 14623




