Tendon Regeneration
 Tendon injuries heal in a fibrotic manner via chronic deposition of excessive, disorganized extracellular matrix. Myofibroblasts are a critical driver of fibrosis in many tissues, and emerging evidence demonstrates myofibroblast heterogeneity. That is, myofibroblasts with unique molecular profiles that correspond to changes in myofibroblast function. Importantly, the fibroblast lineage from which myofibroblasts are derived also plays a major role in dictating myofibroblast function. However, very little is known about myofibroblast dynamics during fibrotic tendon healing, including their fibroblast/tenocyte-lineage, how their functions change over time, what the molecular profiles of these different myofibroblast subtypes are, and how myofibroblasts interact with other cells, such as macrophages, to mediate healing and fibrosis.
Tendon injuries heal in a fibrotic manner via chronic deposition of excessive, disorganized extracellular matrix. Myofibroblasts are a critical driver of fibrosis in many tissues, and emerging evidence demonstrates myofibroblast heterogeneity. That is, myofibroblasts with unique molecular profiles that correspond to changes in myofibroblast function. Importantly, the fibroblast lineage from which myofibroblasts are derived also plays a major role in dictating myofibroblast function. However, very little is known about myofibroblast dynamics during fibrotic tendon healing, including their fibroblast/tenocyte-lineage, how their functions change over time, what the molecular profiles of these different myofibroblast subtypes are, and how myofibroblasts interact with other cells, such as macrophages, to mediate healing and fibrosis.
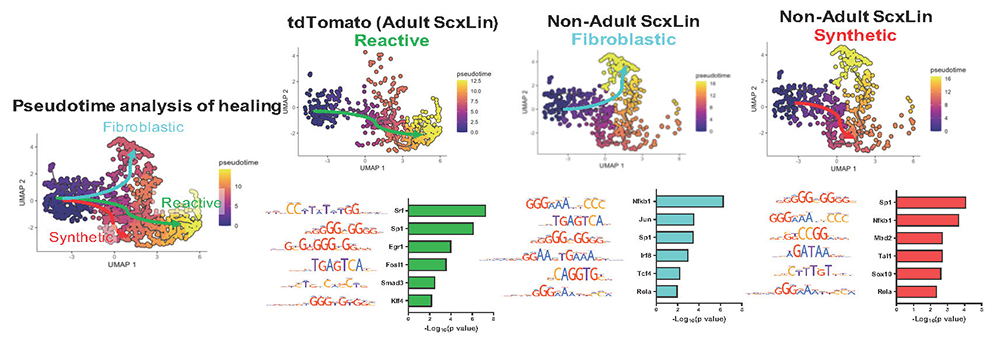
We have identified Scleraxis-lineage and S100a4-lineage cells as the predominant myofibroblast precursor populations during tendon healing. Interestingly, depletion of S100a4-cells impairs early tendon healing, while Scx-cell depletion improves late tendon healing suggesting these cells may give rise to functionally distinct myofibroblast populations. In addition, our preliminary data identifies macrophages as a critical driver of the tenocyte-myofibroblast transition, and we observed prolonged macrophage presence during late healing, concomitant with NFB-mediated pro-survival signaling in myofibroblasts. These data are consistent with a pro-fibrotic feedback loop between macrophages and myofibroblasts to sustain fibrosis in many tissues.
The primary goals of are studies are to: 1) Define the temporal and tenocyte lineage-dependent immunophenotype of myofibroblasts during fibrotic tendon healing. 2) Establish the requirement for extrinsic macrophages in fibrotic healing via modulation of the tenocyte-myofibroblast transition and test the translational potential of inhibiting macrophage recruitment. 3) Demonstrate that disrupting myofibroblast survival or macrophage persistence inhibits sustained fibrosis and promotes regenerative tendon healing. Successful completion of these studies will establish myofibroblast lineage, molecular profile and activation mechanisms over time during fibrotic healing and define disruption of persistent myofibroblasts and macrophages as a novel means to improve tendon healing.