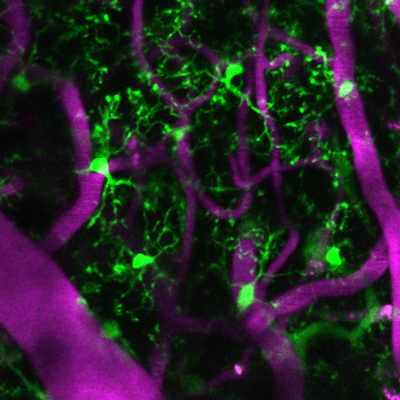
Living microglia, genetically marked to glow green, in the cerebral cortex with magenta colored blood vessels from a mouse treated with URMC-099.
A new study published in the Journal of Neuroinflammation found that prophylactic treatment with URMC-099 -- a "broad spectrum" mixed-lineage kinase 3 inhibitor -- prevents neuroinflammation-associated cognitive impairment in a mouse model of orthopedic surgery-induced perioperative neurocognitive disorders (PND).
PND, a new term that encompasses postoperative delirium, delayed neurocognitive recovery, and postoperative neurocognitive disorder, is the most common complication after routine surgical procedures, particularly in the elderly. Following surgery, such as hip replacement or fracture repair, up to 50 percent of patients experience cognitive disturbances like anxiety, irritability, hallucinations, or panic attacks, which can lead to more serious complications down the line. Currently, there are no FDA-approved therapies to treat it.
Developed in the laboratory of Harris A. "Handy" Gelbard, M.D., Ph.D., director of the Center for Neurotherapeutics Discovery at the University of Rochester Medical Center, URMC-099 inhibits damaging innate immune responses that lead to inflammation in the brain and accompanying cognitive problems. Using animal models of diseases like HIV-1-associated neurocognitive disorders, Alzheimer's disease and multiple sclerosis, Gelbard has shown that the compound blocks enzymes called kinases (such as mixed lineage kinase type 3, or MLK3) that respond to inflammatory stressors inside and outside cells.
Gelbard and Niccolò Terrando, Ph.D., director of the Neuroinflammation and Cognitive Outcomes laboratory in the Department of Anesthesiology at Duke University Medical Center, used an orthopedic surgery mouse model that recapitulates features of clinical procedures such as a fracture repair or hip replacement, which are often associated with PND in frail subjects. In a pilot experiment, they treated one group of these mice with URMC-099 before and after surgery, and another group prior to surgery only. Gelbard and Terrando's teams, including first author Patrick Miller-Rhodes, a senior pre-doctoral student in the Neuroscience Graduate Program working in the Gelbard lab at URMC, measured the following:
- How the surgery affected the central nervous system and the immune cells (microglia) that reside there was evaluated using stereology and microscopy.
- Surgery-induced memory impairment was assessed using the "What-Where-When" and Memory Load Object Discrimination tasks.
- The acute peripheral immune response to surgery was assessed by cytokine/chemokine profiling and flow cytometry.
- Long-term fracture healing was assessed in fracture callouses using micro-computerized tomography and histomorphometry analyses.
- For additional details see the "Materials and Methods" section of the study
The team found that the surgery disrupted the blood brain barrier and activated microglia (a first line immune responder present in the inflamed brain), which led to impaired object place and identity discrimination when the mice were subject to the "What-Where-When" and Memory Load Object Discrimination tasks. Both URMC-099 dosing methods prevented the surgery-induced microgliosis (increase in the number of activated microglia) and cognitive impairment without affecting fracture healing.
"A major concern regarding the use of anti-inflammatory drugs for PND is whether they will affect fracture healing. We found that our preventive, time-limited treatment with URMC-099 didn't influence bone healing or long-term bone repair," said Gelbard and Terrando, professor of Neurology, Neuroscience, Microbiology and Immunology, and Pediatrics at URMC and associate professor of Anesthesiology at Duke University Medical Center, respectively. "These findings of improvement in cognition and normal fracture healing provide compelling evidence for the advancement of URMC-099 as a therapeutic option for PND."
"Right now we have nothing to treat this condition," said Mark A. Oldham, M.D., assistant professor in the department of Psychiatry at URMC who treats patients with PND. "We work hard to provide good medical care, including helping people sleep at night and making sure they are walking, eating and drinking, but it isn't clear that these efforts have any meaningful long-term impact."
According to Oldham, recent studies that track patients following an episode of PND show that many of them don't resolve completely, and that they have a new cognitive baseline after delirium.
"It is increasingly an accepted fact that after delirium, people have suffered some kind of neurological insult, which leaves them cognitively or functionally worse off than before the incident," he noted.
Next steps for the research include identifying definitive mechanisms for pain modulation, immune cell trafficking and neuro-immune characterization in PND. Gelbard and Terrando are tackling some of these questions with funds from the National Institutes of Health (RO1 AG057525). The current study was also funded by multiple grants from the NIH (P01MH64570, RO1 MH104147, RO1 AG057525 and F31 MH113504). The University of Rochester has four issued U.S. patents and multiple issued patents in foreign countries covering URMC-099.