Case of the Month: Hematemesis
By Phoenix Bell, MD, MS and Aaron Huber, DO
Clinical History
A 55-year-old female presented to the emergency department complaining of four episodes of hematemesis with “large blood clots” over three hours. Earlier that day, she had an outpatient esophagogastroduodenoscopy (EGD), which demonstrated diminished rugal folds in the proximal stomach and biopsies of the body were taken.
Past Medical History
The patient’s past medical history includes MGUS, vertigo, hyperlipidemia, cholelithiasis, and acute pancreatitis. Her family history is noncontributory. She is a never smoker and denies any history of alcohol or illicit drug use.
Recent History
The patient had a positive fecal occult blood test (FOBT) and was sent for a second EGD, which showed no old or fresh blood, no clots, and biopsy sites in the healing stage. Chest x-ray was negative and no further imaging was performed. The patient was admitted for hematemesis and decreasing hemoglobin and hematocrit in the setting of recent EGD.
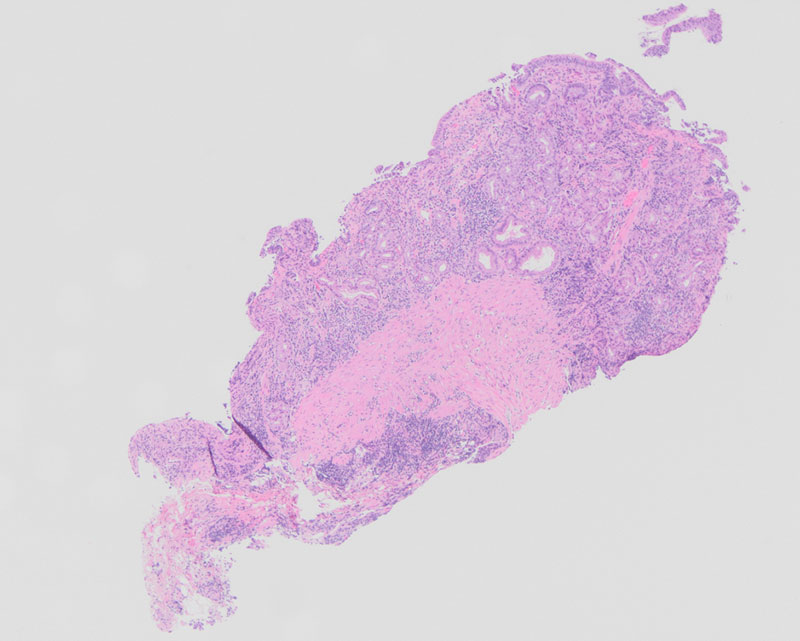
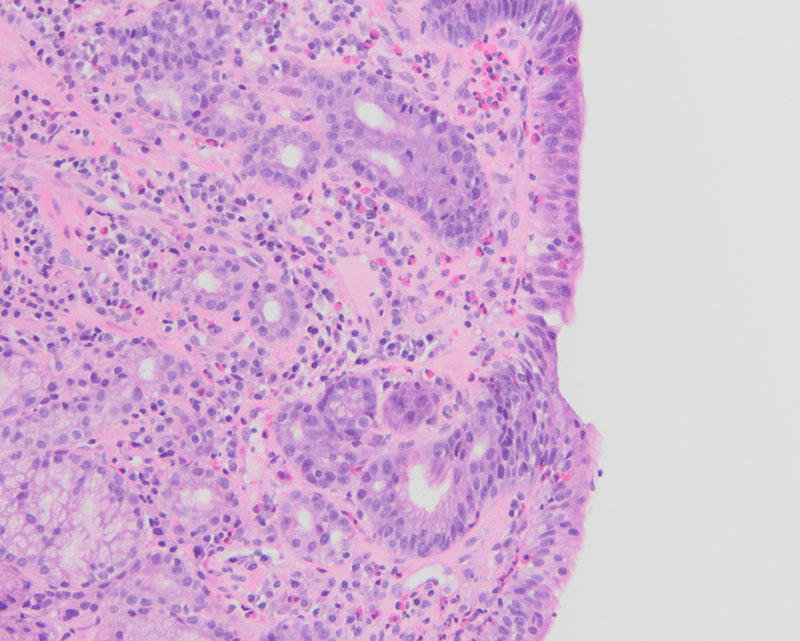
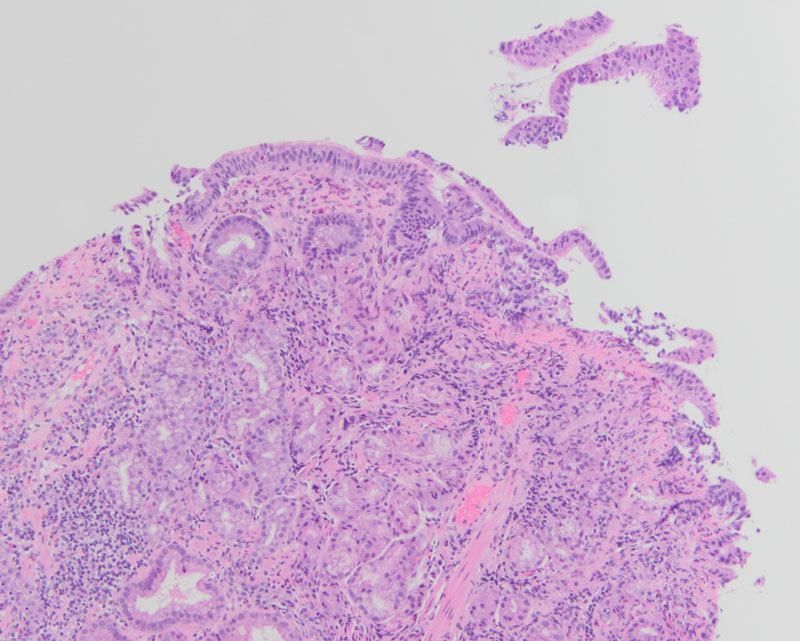
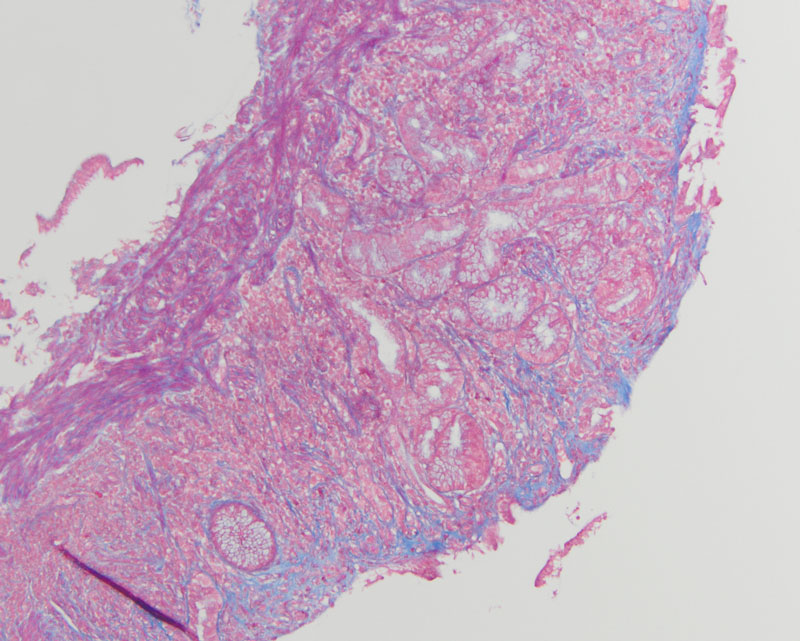
Upon histologic evaluation, low-power magnification revealed gastric mucosa with increased inflammation within the lamina propria, sloughing of the surface epithelium, and surface epithelial damage (Figure 1). On high-power magnification, there was a thickened layer of subepithelial collagen with increased plasma cells, intraepithelial lymphocytes, and eosinophils (Figure 2). Additionally, there was atrophy of the oxyntic mucosa and pyloric gland metaplasia (Figure 3). Trichrome highlighted the thickened subepithelial collagen table (Figure 4). The dense chronic inflammation within the mucosa demonstrated a mixed population of T cells (CD3+, CD5+) and B cells (CD20+), while the lymphoid cells demonstrated no aberrant expression of cyclin D1. An immunohistochemical stain for Helicobacter pylori was negative.