University of Rochester Neurobiologist Suzanne Haber Elected to National Academy of Medicine
Saturday, October 18, 2025
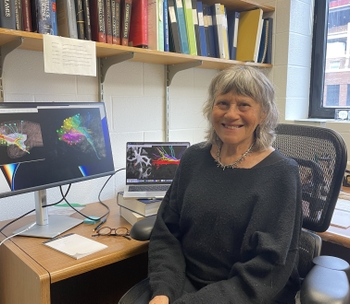
Suzanne N. Haber, PhD
Suzanne N. Haber, PhD, an internationally recognized scientist whose work has transformed our understanding of the brain networks that play a central role in many mental health disorders, including obsessive compulsive disorder (OCD) and depression, has been elected to the National Academy of Medicine (NAM). Recognized as one of the highest accolades in health and medicine, the distinction acknowledges Haber’s significant contributions to the fields of neuroscience and psychiatry over the past 40 years.
Dean’s professor in the Department of Pharmacology and Physiology at the University of Rochester School of Medicine & Dentistry, Haber is a biological map maker, charting the brain regions and circuits that regulate motivation, cognition, and motor control. Through anatomical studies and the use of advanced imaging techniques she’s identified abnormalities in brain circuitry that contribute to neurological and mental health disorders ranging from schizophrenia and OCD to post-traumatic stress disorder, addiction, and depression.
Leader of the National Institutes of Health-funded Silvio O. Conte Center for Basic and Translational Mental Health Research at the University of Rochester, Haber partners with scientists and physicians from institutions across the country to turn her findings on circuit dysfunction into treatments that can improve people’s lives. She’s currently using circuitry models to determine which circuits physicians should target for deep brain stimulation and transcranial magnetic stimulation therapy to be most effective for individuals with OCD, depression, and addiction.
“Suzanne’s research is highly translational,” said Steve Dewhurst, PhD, vice president for Research at the University of Rochester. “Her broad knowledge of brain networks, including the so-called ‘OCD network’, combined with the expertise of state-of-the-art imaging specialists and physicians attuned to patient needs, creates an ideal foundation for understanding how the OCD network regulates brain function in both health and disease. It also sets the stage for the development of innovative treatment strategies. This recognition is a testament to her remarkable insight and collaborative nature.”
Read More: University of Rochester Neurobiologist Suzanne Haber Elected to National Academy of MedicineCongratulations Michael Malloy on receiving a F31 Predoctoral Fellowship from the National Institutes of Health!
Tuesday, September 30, 2025
Michael Malloy, 4th year graduate student in the laboratory of Dr. Craig Morrell was awarded a three-year NIH F31 Predoctoral Fellowship entitled, “Myb regulation of megakaryocyte immune differentiation”. 
Project Summary
Lung megakaryocyte (Mk) derived platelets have been described throughout the past century. Our laboratory previously reported that lung Mks are transcriptionally distinct from bone marrow (BM) Mks and have an immune differentiated phenotype and functions. A recent manuscript from our lab discovered that lung Mks originate from the BM and a developmentally distinct population migrate to the lung. Part of our lab’s current efforts seek to identify the developmental cues and molecular mediators that facilitate the differentiation of Mks fated to stay in the BM or become immune differentiated and travel to the lung. As part of these efforts, I identified a novel mediator of Mk immune differentiation, the proto-oncogene Myb, that regulates the immune phenotype of Mks in both the BM and lung. My work has now found that the majority of BM, but not lung Mks, express the transcription factor, Myb, that may limit Mk immune differentiation, impacting the functions of both lung vs BM derived platelets.
Amy Hong Receives the Connie Eaves Award!
Saturday, September 27, 2025
 Cih-Li (Amy) Hong, 3rd year graduate student in the laboratory of Dr. Shu-Chi (Allison) Yeh was awarded First Prize receiving the Connie Eaves Award for the 2025 ISEH New Investigator Lecture at the Annual ISEH meeting, titled, “Local Bone Remodeling Shapes Hematopoietic Stem Cell (HSC)- Macrophage Interactions and Compartmentalized HSC Expansion under Inflammatory Stress”. Amy gave a 10-minute presentation, followed by a 3-minute Q&A session.
Cih-Li (Amy) Hong, 3rd year graduate student in the laboratory of Dr. Shu-Chi (Allison) Yeh was awarded First Prize receiving the Connie Eaves Award for the 2025 ISEH New Investigator Lecture at the Annual ISEH meeting, titled, “Local Bone Remodeling Shapes Hematopoietic Stem Cell (HSC)- Macrophage Interactions and Compartmentalized HSC Expansion under Inflammatory Stress”. Amy gave a 10-minute presentation, followed by a 3-minute Q&A session.

Amy Hong Selected for the 2025 ISEH Technology and Travel Grant
Saturday, September 27, 2025
Cih-Li (Amy) Hong, 3rd year graduate student in the laboratory of Dr. Shu-Chi (Allison) Yeh was selected for the 2025 ISEH Technology and Travel Grant at the Annual ISEH meeting. Amy presented a 10-minute talk, followed by a 30-minute discussion panel in the session titled, “New Investigatory Technology Session – Latest Advances in Imaging Technologies”.

Amy Hong Awarded the 2025 ISEH PMW Poster Prize!
Wednesday, September 24, 2025
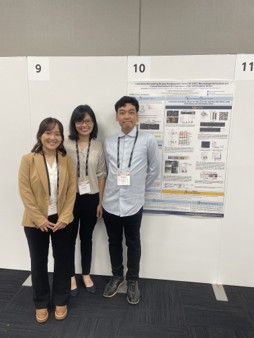 Cih-Li (Amy) Hong, 3rd year graduate student in the laboratory of Dr. Shu-Chi (Allison) Yeh was awarded the 2025 ISEH PMW Poster Prize for her poster presentation at the Annual ISEH pre-meeting, titled, “Local Bone Remodeling Shapes Hematopoietic Stem Cell (HSC)- Macrophage Interactions and Compartmentalized HSC Expansion under Inflammatory Stress”.
Cih-Li (Amy) Hong, 3rd year graduate student in the laboratory of Dr. Shu-Chi (Allison) Yeh was awarded the 2025 ISEH PMW Poster Prize for her poster presentation at the Annual ISEH pre-meeting, titled, “Local Bone Remodeling Shapes Hematopoietic Stem Cell (HSC)- Macrophage Interactions and Compartmentalized HSC Expansion under Inflammatory Stress”.
Congratulations to Amy Hong for receiving a Wilmot Predoctoral Cancer Research Fellowship!
Tuesday, July 1, 2025
 Amy Hong, CMPP 2nd year graduate student in the laboratory of Dr. Shu-Chi Yeh was awarded a two-year Wilmot Predoctoral Cancer Research Fellowship entitled, "Macrophage-Hematopoietic Stem Cell Interaction Regulating Clonal Competition and Progression of Clonal Hematopoiesis".
Amy Hong, CMPP 2nd year graduate student in the laboratory of Dr. Shu-Chi Yeh was awarded a two-year Wilmot Predoctoral Cancer Research Fellowship entitled, "Macrophage-Hematopoietic Stem Cell Interaction Regulating Clonal Competition and Progression of Clonal Hematopoiesis".
Project Summary
Clonal hematopoiesis of indeterminate potential (CHIP) is driven by mutated hematopoietic stem cells (HSCs) that are granted with a competitive advantage and expand disproportionately in the bone marrow. Aging-induced inflammation is known to be a major driver for selection of CHIP clones. For this reason, it is crucial to understand mechanisms to maintain HSC fitness while suppressing mutant clone expansion under inflammatory conditions. Our preliminary data revealed that HSCs within a subset of marrow cavities that lack bone resorption activity stayed solitary despite activation from various inflammatory stresses including aging. These results suggest the existence of a protective microenvironment in the non-resorptive (NR) cavities that shelters HSCs under systemic inflammation and may protect them from aging-induced inflammation. My goal in this work is to investigate spatial heterogeneity of cavity resident macrophages that regulates clonal competition and progression of clonal hematopoiesis leveraging intravital microscopy.
Congratulations to Dr. Lily Cisco for winning the Postdoctoral Best Poster Award at the 36th Annual Genetics Day
Monday, April 28, 2025
 Lily Cisco, Ph.D., Postdoctoral Fellow in the laboratory of John D. Lueck, Ph.D. has earned the Genetics Day Poster Prize–Postdoctoral Category at the 36th Annual Genetics Day Poster Competition, titled, “Treatment of a severe DM1 mouse model with verapamil, amlodipine, and ranolazine”.
Lily Cisco, Ph.D., Postdoctoral Fellow in the laboratory of John D. Lueck, Ph.D. has earned the Genetics Day Poster Prize–Postdoctoral Category at the 36th Annual Genetics Day Poster Competition, titled, “Treatment of a severe DM1 mouse model with verapamil, amlodipine, and ranolazine”.
Genetics Day is designed to not only showcase the current year’s genetics research but also provide a platform for trainees to present their data and interact with scientists throughout the URMC community. The events that take place during Genetics Day include talks by faculty and trainees, trainee poster session, and keynote lecture.
Congratulations to John Conduah of the Onukwufor lab for receiving both a Dekiewiet Summer Research Fellowship and Schwartz Discover Grant
Thursday, April 10, 2025

These awards will fund John’s summer research project and help elucidate how interactions between Cd, Pb and Fe contribute to mechanisms of acute metal toxicity and liver mitochondrial dysfunction.
Congratulations to Michael Malloy as the recipient of a two-year Predoctoral Fellowship from the American Heart Association
Wednesday, January 1, 2025
 Michael Malloy, 3rd year graduate student in the laboratory of Dr. Craig Morrell was awarded a two-year American Heart Association Predoctoral Fellowship entitled, “Myb regulation of megakaryocyte immune differentiation”.
Michael Malloy, 3rd year graduate student in the laboratory of Dr. Craig Morrell was awarded a two-year American Heart Association Predoctoral Fellowship entitled, “Myb regulation of megakaryocyte immune differentiation”.
Project Summary
Lung megakaryocyte (Mk) derived platelets have been described throughout the past century. Our laboratory previously reported that lung Mks are transcriptionally distinct from bone marrow (BM) Mks and have an immune differentiated phenotype and functions. A recent manuscript from our lab discovered that lung Mks originate from the BM and a developmentally distinct population migrate to the lung. Part of our lab’s current efforts seek to identify the developmental cues and molecular mediators that facilitate the differentiation of Mks fated to stay in the BM or become immune differentiated and travel to the lung. As part of these efforts, I identified a novel mediator of Mk immune differentiation, the protooncogene Myb, that regulates the immune phenotype of Mks in both the BM and lung. My work has now found that the majority of BM, but not lung Mks, express the transcription factor, Myb, that may limit Mk immune differentiation, impacting the functions of both lung vs BM derived platelets.
Congratulations to Nada Ahmed Selim on receiving the Predoctoral Fellowship from the American Heart Association!
Wednesday, January 1, 2025
 Nada Ahmed Selim, 4th year graduate student in the laboratory of Dr. Andrew Wojtovich was awarded a two-year American Heart Association Predoctoral Fellowship entitled, “Optogenetic regulation of mitochondria to improve ischemiareperfusion injury outcomes”.
Nada Ahmed Selim, 4th year graduate student in the laboratory of Dr. Andrew Wojtovich was awarded a two-year American Heart Association Predoctoral Fellowship entitled, “Optogenetic regulation of mitochondria to improve ischemiareperfusion injury outcomes”.
Project Summary
Mitochondria coordinate metabolism, ATP synthesis, and cell death, and their function is essential for neuronal survival and post-stroke recovery. Mitochondria are powered by the electron transport chain (ETC), which creates an electrochemical protonmotive force (PMF) across the inner mitochondrial membrane that drives oxidative phosphorylation to generate ATP. The PMF is essential for neuronal function, and its disruption adversely affects neurons through poorly understood mechanisms. PMF responds rapidly to energy demands and stress, signaling metabolic needs. During ischemia-reperfusion (IR) injury, the PMF decreases and then is restored upon reperfusion. The rapid change in PMF during IR is associated with numerous pathological events at the mitochondrial level, such as excessive production of reactive oxygen species (ROS), calcium overload, and subsequent initiation of cell death cascades.