What is Asthma?
Asthma is a common chronic (long term) lung disease affecting over 25 million Americans. The airways react to different triggers (allergens and irritants) and become swollen and inflamed. The muscles around the airways tighten and there is increased mucus production. All of these changes make the airways narrow. This makes it hard for air to go in and out of the lungs.
What causes asthma?
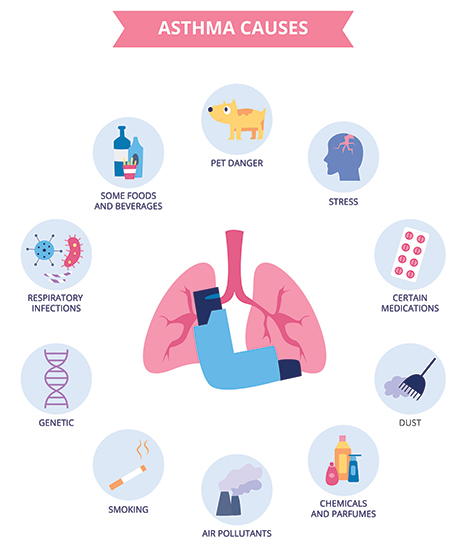 Experts don't know the exact cause of asthma but it is thought to be a combination of genes and environmental factors. Asthma can be inherited, or may occur without a family history of asthma or allergies. It often presents early in childhood but can also develop later in life. In addition to genetics, the environment, infections and body’s immune responses also play a role.
Experts don't know the exact cause of asthma but it is thought to be a combination of genes and environmental factors. Asthma can be inherited, or may occur without a family history of asthma or allergies. It often presents early in childhood but can also develop later in life. In addition to genetics, the environment, infections and body’s immune responses also play a role.
Exercise causes symptoms in many people with asthma. Symptoms can occur during or shortly after exercise. In some people, stress or strong emotions can also trigger asthma symptoms.
Other common asthma triggers include:
Allergens
- Pollens (trees, grasses, and weeds)
- Mold
- Pets
- Dust and dust mites
- Cockroaches
- Mice
Respiratory problems
- Nasal allergies
- Sinus infections
- The flu
- Viral infections, including the common cold
Irritants
- Strong odors from perfumes, household cleaners, cooking fumes, paints, and varnishes
- Chemicals (gases, fumes)
- Air pollution
- Changing weather conditions (temperature, barometric pressure, humidity, and strong winds)
- Smoke (tobacco-inhaled or secondhand)
Medicines
- Aspirin
- NSAIDs (nonsteroidal anti-inflammatory drugs) such as ibuprofen
Several other medical conditions can also worsen asthma symptoms including acid reflux, depression, obesity, sleep apnea and sinus disease.
What are the symptoms of asthma?
Common asthma symptoms include:
- Shortness of breath
- Chest tightness
- Wheezing or a whistling sound when breathing
- Cough
Symptoms can be severe during an ‘asthma attack’. If you experience any of these symptoms, you should seek emergent medical care.
- Breathing becomes harder and may hurt
- Talking becomes difficult because of shortness of breath
- Coughing, wheezing and chest tightness can make you feel anxious or scared
How is asthma diagnosed?
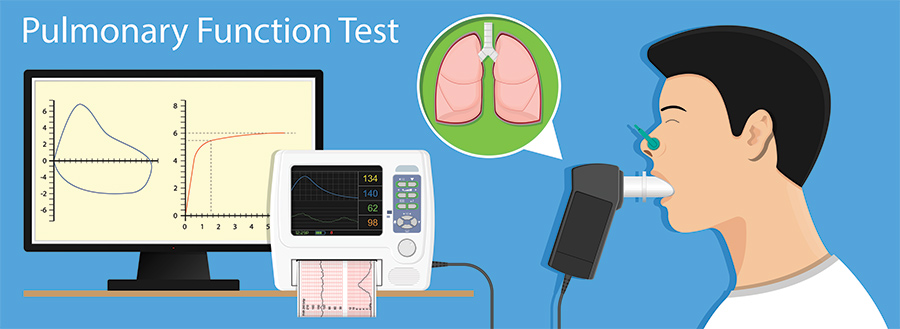
Your healthcare provider will take your health history and give you a physical exam. You may also have other tests including lung function, blood and allergy testing.
An important test when evaluating asthma is spirometry. A spirometer is a device used to find out how well the lungs are working. It measures the amount and speed of air breathed out.
How is asthma treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
There is no cure for asthma. It can often be controlled by staying away from triggers and by taking medicines as prescribed by your healthcare provider.
Monitoring your symptoms is a key part of asthma care. So is knowing what to do if symptoms get worse. Discuss an Asthma Action Plan with your provider.
Medicines for asthma
The two types of asthma medicines are long-acting (controller) and short-acting (reliever or rescue) medicines. Controller medicines are taken on a regular basis and work to control inflammation and keep your airways open. They help prevent symptoms. Reliever or rescue medicines are short-acting and calm asthma symptoms fast. But their effect only lasts for a short time.
Your healthcare provider will regularly check and adjust your medicines as needed.
Controller medicines
At first, it may take a few weeks for long-term control medicines to work. You must take these medicines on a regular basis. These medicines include:
- Inhaled corticosteroids. These medicines reduce or prevent airway swelling and inflammation.
- Long acting bronchodilators. These medicines relax muscles around the airways.
- Leukotriene modifiers. These medicines block the action of certain chemicals (leukotrienes). These chemicals cause airway inflammation and narrowing.
- Biologics. This medicines are usually given as an injection in moderate to severe asthma when regular controller medications are not effective. They work by blocking proteins and receptors in the body that cause inflammation and asthma attacks.
Reliever or rescue medicines
These medicines are short-acting bronchodilators, such as albuterol, that quickly relax the muscles around the airways. But the relief only lasts about 2 to 3 hours.
Living with asthma
Staying away from triggers is key in managing asthma. Triggers may be allergens, irritants, other health problems, exercise, medicines, and strong emotions. The following can help you limit your exposure:
Allergies
- Dust. Dust is the most common year-round allergen. The allergy is caused by tiny dust mites. Dust mites are found in mattresses, carpets, and fabric-covered (upholstered) furniture such as sofas and chairs. They live best in warm, humid conditions. It's important to limit your exposure. Take extra care in the bedroom. Put dust mite covers on your mattress, box spring, and pillows.
- Pollens. You may be allergic to pollen. If so, during pollen season keep all car and house windows closed. Use air conditioning. If you are outside, shower, wash your hair, and change clothes when you go inside.
- Pets. Pets that have fur or feathers often cause allergies. If you have pets, try not to touch them. If you do pet or handle them, wash your hands afterward. Keep pets off your bed and out of your bedroom. Have someone brush and bathe your pet often.
- Mold and mildew. These can trigger asthma. When outside, stay away from damp, shady areas. Use exhaust fans when cooking or bathing. Keep indoor humidity below 45%. And drain and clean your dehumidifier often.
Exercise
Exercise is a common asthma trigger. But don't limit sports or exercise unless a healthcare provider tells you to. Exercise is good for your health and lungs. Swimming, golf, and karate are good choices if you have asthma. Always warm up before exercise. And cool down after. Ask your provider about using your quick-relief medicine before starting exercise.
Irritants
If you smoke, quit.
Stay away from smoke. Don’t use wood stoves or kerosene heaters. Also stay away from strong perfumes, cleaning products, fresh paint, and other things with strong odors.
Medicines
Some medicines can make asthma symptoms worse. Talk with your provider about your asthma history and medicine use.
Other health problems
Some health problems can make it harder to control asthma. These include:
- Respiratory infections such as colds and the flu
- GERD (gastroesophageal reflux) and heartburn
- Being overweight
- Sleep apnea
- Depression
Work with your provider to treat any of these problems.
Strong emotions
The strong feelings that go with laughing and crying can trigger asthma symptoms. You can learn how to better manage your emotions.
Key points about asthma
- Asthma is a long-term (chronic) lung disease.
- Triggers irritate sensitive airways. This makes it hard to breathe.
- Staying away from triggers is an important part of treatment.
- Long-term medicines control symptoms. They are taken on a regular basis, even when you feel well.
- Rescue medicines provide quick symptom relief but the effects are short-lasting.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.