Airway Inflammation and Lung Function in Asthma
For reasons that are not entirely clear, patients with asthma develop deleterious immune responses to otherwise innocuous substances, like allergens, that result in tissue inflammation and airway hyperreactivity. Patients with asthma are also more susceptible to infections with respiratory viruses, that can lead to prolonged loss of asthma control. Many pathologic immune responses in asthma are “type 2”, that is they are characterized by aberrant production of the Th2-type cytokines IL-4, IL-5 and IL-13 by CD4+ T cells and innate lymphoid cells. I began my career by studying how the innate and adaptive immune systems interact to generate type 2 immune responses. Currently a major emphasis of my research lab is to study respiratory-virus induced epithelial barrier dysfunction, that may be associated with virally-induced asthma exacerbations.
I am also a practicing physician and see outpatients with severe asthma at the Mary Parkes Asthma Center. We are currently enrolling subjects in different studies investigating new ways to diagnose asthma, as well as new treatment options for patients with asthma.
If you are a patient interested in participating in a clinical research study: Clinical Research Information
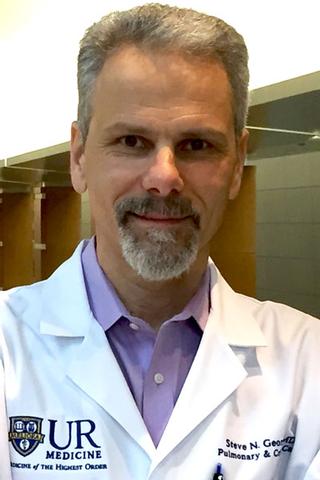
Steve N. Georas, M.D.
Principal Investigator
Publications
View All Publications- PrecISE- A Biomarker Stratified Adaptive Trial of 5 Interventions in Severe Asthma: Final Protocol and the Baseline Cohort.; The Journal of allergy and clinical immunology. 2026 Feb 16.
- Targeted treatment in asthma - opportunities and challenges.; The journal of allergy and clinical immunology. In practice. 2025 Nov 26.
- Is Tissue the Issue When It Comes to Severe Asthma?; Chest; Vol 167(4), pp. 911-913. 2025 Apr.
News
Affiliations
- Medicine
- Environmental Medicine
- Microbiology & Immunology
- Center for Inhalation and Flavoring Toxicological Research (CIFT)
- Environmental Health Sciences Center
- Lung Biology and Disease Program
- NIH T32 Training Grant in Immunology
- Pulmonary T32 Training Grant
- Immunology, Microbiology, and Virology Ph.D. Program
- PhD Program in Pathology - Cell Biology of Disease
- Toxicology Ph.D. Program
- Translational Biomedical Science Ph.D. Program
- Program for Advanced Immune Bioimaging
April 30, 2025
Eric Merrell Publishes Editorial in Chest
December 24, 2024
Ugly Sweaters Take Center Stage at Pulmonary and Critical Care Celebration
October 17, 2024
Pulmonary Division Excels at CHEST Conference in Boston
July 12, 2024
New Grant Will Boost Training in Lung Disease Research
Contact Us
Georas Lab
KMRB 2-9816C
601 Elmwood Ave
Rochester, NY 14642
(585) 273-1114


