Case of the Month: Abdominal Pain, Bloody Bowel Movements
By Phoenix D. Bell, MD, Michael G. Drage, MD, PhD, Aaron R. Huber, DO
Clinical History
A 24-year-old male presented to the emergency department with a one week history of worsening abdominal pain (10/10), bloody bowel movements, and one episode of non-bloody emesis. Eight months earlier, he presented to the emergency department with abdominal pain, unintentional weight loss, and 12 episodes of dark brown bowel movements with intermittent blood and mucus, of mildly increased frequency (2-3x/day as baseline 1-2x/day). Abdominal ultrasound showed a mildly dilated CBD (0.7cm) and his liver function tests were elevated (AST 298, ALT 254, and ALK 742).
Two weeks later he underwent liver biopsy/MRCP, which revealed mild chronic portal inflammation, bile duct disarray, and ductular reaction, concerning for primary sclerosing cholangitis (PSC) or primary biliary cholangitis (PBC) and he was started on ursodiol. One month later, he underwent colonoscopy due to concern for PSC and the potential for inflammatory bowel disease (IBD). Colonoscopy showed pan-colitis with diffuse erythema, edema, and friability of the right colon. Colonic biopsies revealed markedly active chronic colitis. The patient was diagnosed with primary sclerosing cholangitis (PSC) and ulcerative colitis (UC) and started on mesalamine; however, three weeks later he presented again for continued abdominal cramping and little to no improvement in his bowel movements. He was started on azathioprine and prednisone. One month later, he was hospitalized for abdominal pain and an abdominal CT revealed mural thickening, mucosal enhancement, hyperemia, and small free fluid involving the cecum, ascending colon, descending colon, and sigmoid colon, consistent with UC. Additionally, there was inflammation of the terminal and distal ileum. He was started on Humira and instructed to continue mesalamine and azathioprine with a follow-up appointment in 6 weeks.
Past Medical History??
PSC, UC, GERD, ADHD
Recent History
Two weeks prior to his recommended follow-up appointment, the patient presented to the emergency department with the abovementioned symptoms (one week history of worsening abdominal pain, bloody bowel movements, and one episode of non-bloody emesis). The patient was sent for an abdominal CT, which showed an acute UC flare involving the entire colon. Additionally, a bacterial polymerase chain reaction panel was sent and came back positive for Salmonella. The patient was started on a two-week course of Ciprofloxacin; however, his symptoms (10-15 bowel movements/day) failed to improve. The patient elected to undergo a subtotal colectomy with end ileostomy.
Pathology?
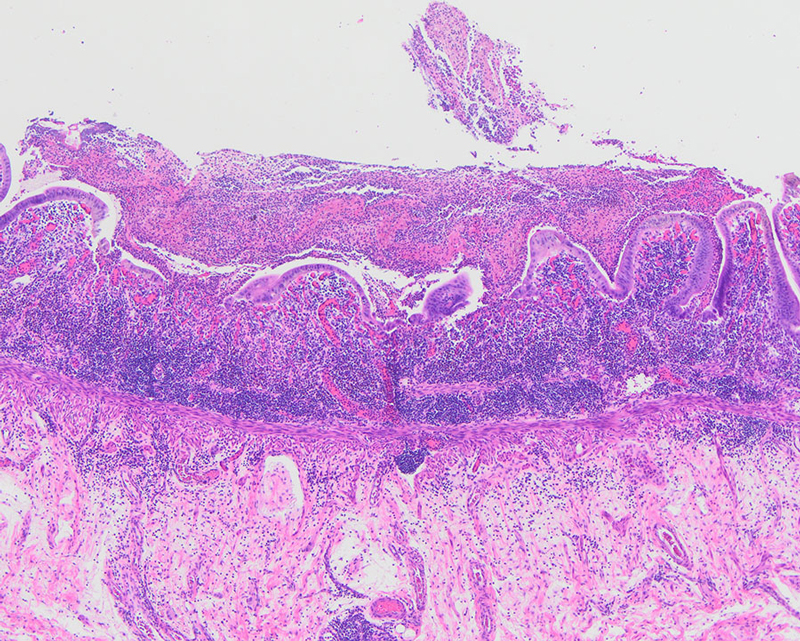
Gross examination of the resection specimen showed diffuse membranous adhesions on the serosal surfaces. The small bowel mucosa was dark red, hemorrhagic, and granular with focal areas of friability. The colonic mucosa was dark red, hemorrhagic, and diffusely ulcerated with tan plaque-like material in the cecum and ascending colon (Figure 1). Histologic examination demonstrated severe active chronic ileitis with ulceration (Figure 2) and diffuse, severe active chronic colitis with ulceration (Figure 3).