Case of the Month: Vaginal Bleeding
Case Author: Aaron Huber, D.O.
Clinical History
A middle-aged woman presented to her gynecologist with vaginal bleeding and anemia.
Past Medical History
The patient was being followed as an outpatient for a large uterus with suspected leiomyomata, anemia, vitamin D deficiency, and gastroesophageal reflux disease.
Recent History
She was sent from the gynecologist to the emergency department after pelvic examination revealed a large amount of organized clot (estimated 500 milliliters) as well as active bleeding. The plan was to perform uterine artery embolization to control the bleeding. However, a computed tomography scan with angiography of the abdomen and pelvis demonstrated diffuse hepatic metastases, bibasilar pulmonary metastases, as well as uterine and cervical enlargement.
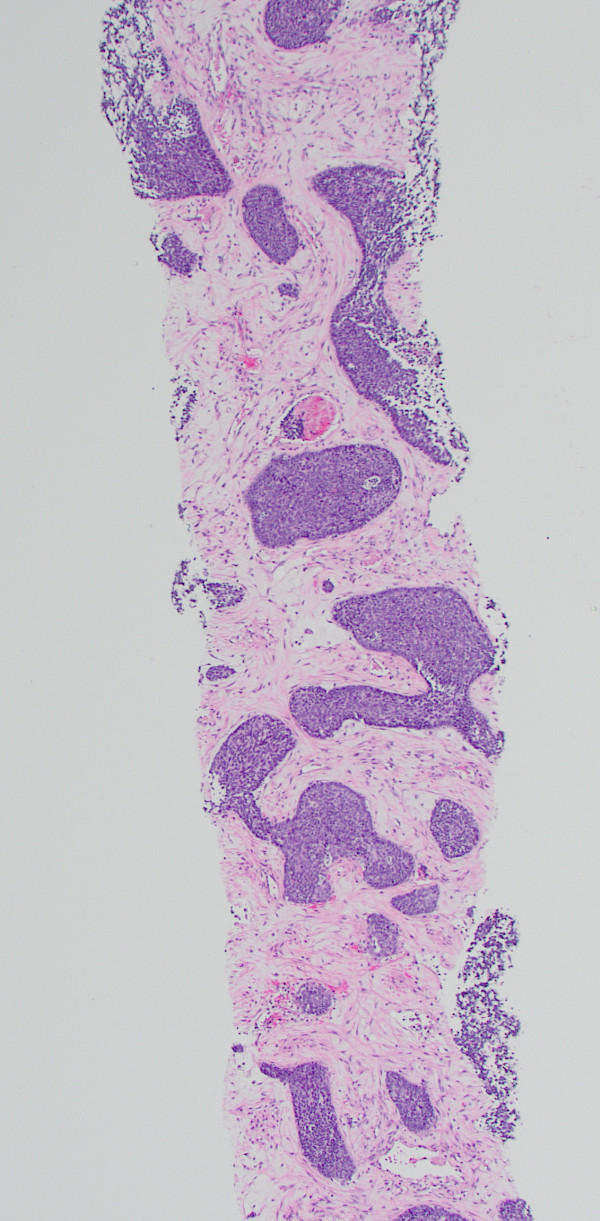
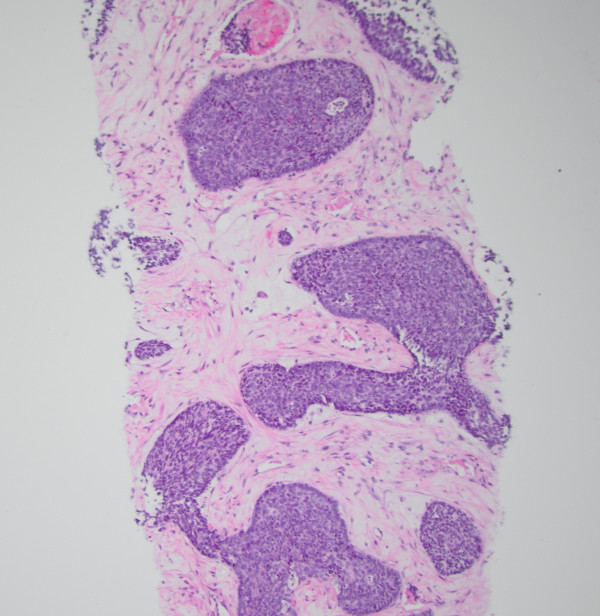
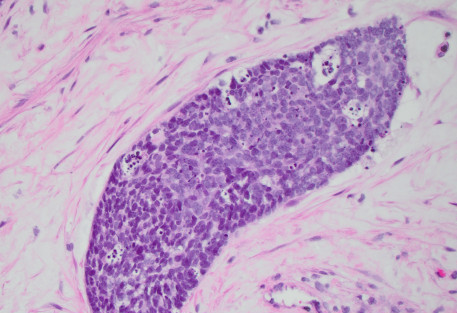
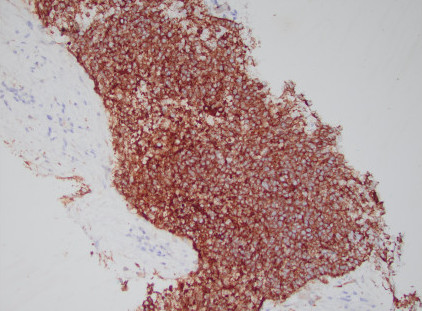
A liver biopsy was performed. H&E-stained sections of the liver biopsy demonstrated nests of malignant cells with scant cytoplasm and hyperchromatic, round nuclei. Numerous apoptotic bodies were seen (Figures 1, 2, and 3). Immunohistochemical stains were performed and the neoplastic cells were positive for cytokeratin AE1/AE3 (Figure 4), CD99, p16 (Figure 5), and INSM1 (focally positive). The neoplastic cells were negative for synaptophysin, chromogranin, and p40. High-risk human papillomavirus (HPV) in situ hybridization stain was positive. The Ki-67 labeling index was over 90% of the neoplastic cells. A concurrent biopsy of the uterine cervix was performed and had similar morphology to the liver lesion.