Curriculum
Curriculum
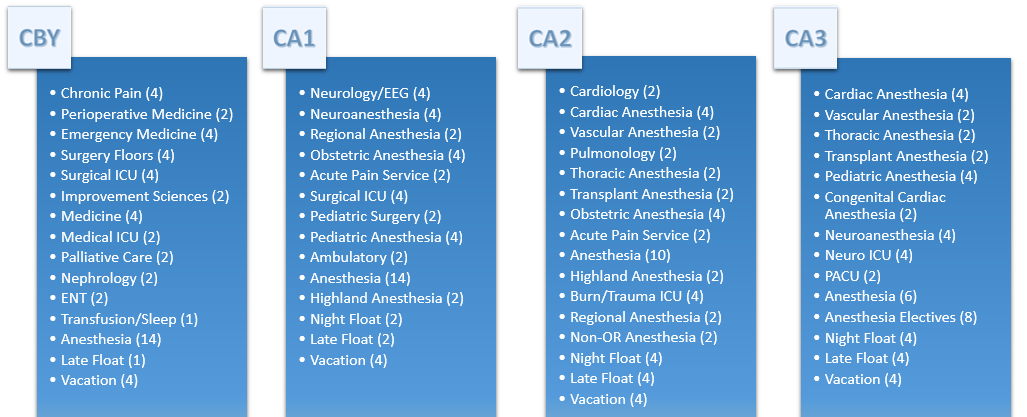
One of the single greatest recent innovation in our residency program was the introduction of an Integrated (Categorical) Residency Program in Anesthesiology and Perioperative Medicine in 2011. Despite what programs will tell you, few offer the truly integrated experience that we initiated. Our residents join the department as PGY1s (Clinical Base Year, CBY), orient to clinical anesthesia in either September or January of CBY, and complete deliberately scheduled and appropriately juxtaposed “floor” rotations during their CA1 and 2 years. For example, residents complete two weeks of cardiology before the cardiac anesthesia rotation. Similar rotations are paired with the neurologic, obstetric, and pediatric anesthesia subspecialties.
Sample Schedule: