Pregnancy is a high-risk condition for developing a severe form of COVID-19 disease, with an increased risk for hospitalization, complications and death. More than half of pregnant individuals also fall into another high-priority category, including frontline workers and those with underlying medical conditions. If you get COVID-19 in pregnancy, and develop severe symptoms, you may need to be admitted and/or delivered early.
Since the theoretical risk of fetal harm from mRNA vaccines is very low, the benefits from vaccination likely greatly outweigh these risks in anyone exposed to COVID-19 at work or at home.
The American college of Obstetrics and Gynecology and the Society of Maternal Medicine have more information and similarly recommend that for pregnant individuals, the decision to vaccinate must be left to each patient in consult with their trusted clinician, as well as notes the high risk nature of COVID infection in pregnancy. Learn more about vaccines on the CDC website as well.
Several national leadership organizations in pregnancy and neonatal care including - SMFM, AWHONN, NPWH, and ACNM have put out joint recommendations about COVID-19 and COVID vaccinations in pregnancy, with a great deal of more information about the risks of COVID-19 in pregnancy, and a discussion of the vaccine in pregnancy and lactation. These groups recommend that healthcare workers and others who are considered prioritized for vaccination, such as teachers or first responders, be offered the vaccine even if they pregnant or lactating, and discuss the options with their provider.
There is also no current information about the safety of the new COVID-19 vaccines during breastfeeding. Based upon the limited information that we have; we believe it will be safe for use during breastfeeding. The URMC lactation service has more information about COVID and lactation.
These decisions are complicated, and we understand that you may wish to speak to someone about them directly. Please talk to your obstetrical provider if you would like more information or help with making this decision. The MotherToBaby service has put together more information on vaccination and breastfeeding. They are also happy to speak with you as well, by text, chat, or phone.
Also see Doctors Say It's Safe for Pregnant Women to Take COVID-19 Vaccine, where Dr. Eva Pressman talks with 13 WHAM about the vaccine.
If you do choose to get the vaccine while pregnant or lactating, there is a national registry through the University of Washington to help us learn about the outcomes and safety of the COVID vaccine in pregnancy that you can join and well as one through MotherToBaby. The CDC has a large registry as well—V-SAFE. V-SAFE is a smartphone-based tool that uses text messaging and web surveys to provide personalized health check-ins after you receive a COVID-19 vaccine. Through V-SAFE, you can quickly tell CDC if you have any side effects after getting the COVID-19 vaccine.
Based on the initial V-SAFE data for pregnancy, over 30,000 patient have chosen to receive the COVID vaccine in pregnancy as of 2.16.21. The registry data suggest that the COVID vaccine appears to be very safe in pregnancy, with similar or lower rates of pregnancy complications in those that have been vaccinated compared to those in the general population in the United States.
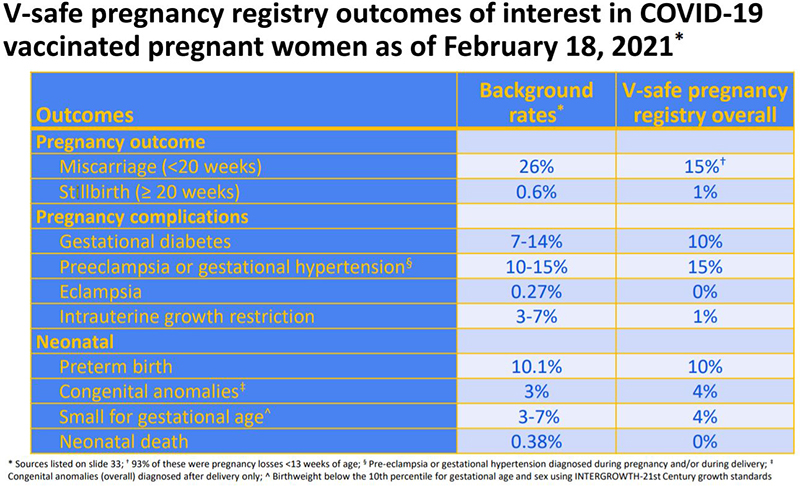
Source: https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-02/28-03-01/05-covid-Shimabukuro.pdf