News
20242023202220212020
Subscribe to Neuroscience LISTSERV
Researchers find neurons work as a team to process social interactions
Monday, November 27, 2023
Researchers have discovered that a part of the brain associated with working memory and multisensory integration may also play an important role in how the brain processes social cues. Previous research has shown that neurons in the ventrolateral prefrontal cortex (VLPFC) integrate faces and voices—but new research, in the Journal of Neuroscience, shows that neurons in the VLPFC play a role in processing both the identity of the “speaker” and the expression conveyed by facial gestures and vocalizations.
“We still don’t fully understand how facial and vocal information is combined and what information is processed by different brain regions,” said Lizabeth Romanski, PhD, associate professor of Neuroscience at the Del Monte Institute for Neuroscience at the University of Rochester and senior author of the study. “However, these findings confirm VLPFC as a critical node in the social communication network that processes facial expressions, vocalizations, and social cues.”
Also featured on NeuroscienceNews.com
Read More: Researchers find neurons work as a team to process social interactionsPulling the Plug on Brain Injury
Wednesday, November 15, 2023
Manipulating Fluid Flows Could Save Lives, Improve Recovery Post-TBI
Cerebral edema, the dangerous brain swelling that occurs after traumatic brain injury (TBI), can increase risk of death tenfold and significantly worsen prospects for recovery in brain function. In extreme cases, surgeons will remove a portion of the skull to relieve pressure, but this has significant risks and is not viable for the vast majority of TBI cases. Physicians have very few tools at their disposal that are effective in treating cerebral edema, which is one of the leading causes of in-hospital deaths and is associated with long-term neurological disability.
New research appearing today in the journal Nature could change all that, showing that a cocktail of drugs already approved to treat high blood pressure quickly reduces brain swelling and improves outcomes in animal models of brain injury.
“Our research shows that cerebral edema is the consequence of impaired fluid flow through the glymphatic system and its associated lymphatic drainage,” said Maiken Nedergaard, MD, DMSc, co-director of the University of Rochester Center for Translational Neuromedicine and senior author of the study. “This impairment is under adrenergic control, and can therefore be rescued pharmacologically by broadly inhibiting adrenergic receptors. Because these drugs are already being used clinically and have observed neurological benefits, there is the potential to move quickly to clinical studies to confirm these findings.”
The glymphatic system holds key to relieving brain pressure
The glymphatic system was first described by Nedergaard’s lab in 2012 as the brain’s unique waste removal process. Since then, a growing understanding of the mechanics of the system–aided by advanced imaging technologies and AI-driven models of fluid dynamics—has allowed researchers to better predict and manipulate the movement of cerebrospinal fluid (CSF) in the central nervous system. This research has opened new possibilities to treat Alzheimer’s and other neurological disorders and more effectively deliver and distribute drugs in the central and peripheral nervous system, including the inner ear.
The new study points to the potential to repurpose the glymphatic system to act as an emergency pressure release valve. Cerebral edema is a common consequence of moderate and severe cases of TBI. “In other parts of the body, edema helps with tissue repair, but because of the skull, the brain has limited capacity for expansion. As a result, pressure increases, blood supply decreases, and debris and toxic proteins are trapped at the injury site, compounding the damage and impairing recovery,” said Rashad Hussain, PhD, an assistant professor in the Center for Translational Neuromedicine and first author of the study.
Read More: Pulling the Plug on Brain Injury2023 GEPA Award Recipients
Thursday, October 19, 2023
Several of the NGP students were recently selected for a number of the annual GEPA awards. Historically, our students have done quite well and this year is no exception. Four of our students were in the mix again laying claim to four of the awards with monetary prizes ranging from $500 - $1000. If you run into Aiesha, Amelia, Nicole, or Linh, please congratulate them, or better yet send them an email on a job well done and for keeping NGP in the spotlight. Here are a list of the awards:
| Student Award Recipients |
| Aiesha Anchan |
Graduate Alumni Fellowship Award |
| Amelia Hines |
Merritt and Marjorie Cleveland Fellowship |
| Nicole Popp |
Irving L. Spar Fellowship Award |
| Linh Le |
Outstanding Student Mentor Award |
4 NGP Faculty are also receiving Faculty and Staff Teaching Mentoring Awards as part of the GEPA awards this year. When you see any of these outstanding faculty members, make sure to also congratulate them on these recognitions. Without them, our NGP students would not be as exveptional for all these years.
| Faculty and Staff Teaching & Mentoring Award Recipients |
| Ania Majewska |
Graduate Student Society Advocacy Award |
| Nathan Smith |
Graduate Student Society Advocacy Award |
| Marissa Sobolewski |
Outstanding Graduate Student Teacher Award |
| Pat White |
Outstanding T32 Program Director Award |
These awards will be presented at the Graduate Education and Postdoctoral Affairs Awards and Philosophy Meeting on Monday, October 30, 2023 at 3:00 pm in the Flaum Atrium. We hope you make an effort to attend to support our students as well as the others receiving awards.
URMC Selected for NIH Initiative to Map Connections in the Brain
Tuesday, September 26, 2023
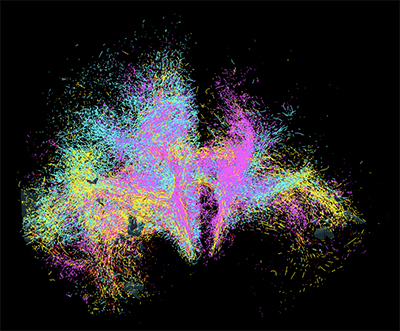 Goal is to Develop Cutting-Edge Tools to Image Neural Networks in Unprecedented Detail
Goal is to Develop Cutting-Edge Tools to Image Neural Networks in Unprecedented Detail
Scientists at the University of Rochester Medical Center are joining research teams across the globe to develop next-generation tools for visualizing connections in the human brain. Imaging and understanding the brain’s intricate circuitry at the cellular and microscopic level will advance new approaches to treat brain disorders like Tourette’s syndrome, Parkinson’s disease, and obsessive-compulsive disorder.
The research is supported by the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies® Initiative, or The BRAIN Initiative®. Principal investigator Suzanne Haber, PhD, professor of Pharmacology and Physiology at URMC, will lead a team of scientists with co-principal investigators Anastasia Yendiki of Massachusetts General Hospital and Elizabeth Hillman of Columbia University.
Haber’s lab will launch the team’s efforts by providing the “ground truth”—animal tracing data that is considered the gold standard for understanding the complex connectivity of the human brain.
“We can’t develop tools without a guide to start with, just like you can’t navigate the ocean without a map,” noted Haber, who is also a professor of Neuroscience, Brain and Cognitive Science, and Psychiatry. “Once we identify how axons traverse the brain in animal models, we use that information to develop tools to accurately track connections in the human brain. These novel technologies for imaging axonal projections will increase our understanding of the circuitry and cellular mechanisms that underlie brain abnormalities.”
Today, diffusion MRI (dMRI) is used to examine the connectivity and functional networks in the human brain. However, this is an indirect method with inherent problems, particularly in specific situations that make it difficult to accurately follow the axons. This leads to many false positives and false negatives.
 Haber says the time is right for this initiative. “We’ve seen so many exciting developments in optics and engineering over the past few years…the field has really exploded,” she notes. “We’re excited to be part of the team that’s pushing the boundaries to better understand the circuitry in humans. Ultimately, we hope this work sets the stage for the creation of more accurate diagnostics and therapeutics for brain diseases.”
Haber says the time is right for this initiative. “We’ve seen so many exciting developments in optics and engineering over the past few years…the field has really exploded,” she notes. “We’re excited to be part of the team that’s pushing the boundaries to better understand the circuitry in humans. Ultimately, we hope this work sets the stage for the creation of more accurate diagnostics and therapeutics for brain diseases.”
Haber’s work, which will be funded by $1.5 million from NIH over five years, is part of the center for Large-scale Imaging of Neural Circuits (LINC). In addition to the University of Rochester, Massachusetts General Hospital and Columbia University, the LINC project includes collaborators from Brigham and Women’s Hospital, Harvard University, Massachusetts Institute of Technology, University College London, and Weill Cornell Medicine.
The BRAIN Initiative is a partnership between federal and non-federal partners, with the NIH taking the leading role in achieving the goal of revolutionizing our understanding of the human brain by accelerating the development of innovative neurotechnologies. The program is made up and managed by 10 NIH institutes and centers whose missions and current research portfolios complement the goals of the BRAIN Initiative. The initial round of awards is projected to total $150 million over 5 years, with a large portion of the funds dedicated to tool development.
Fellowship awards and training grant appointments
Monday, August 28, 2023
John (Jay) Gonzalez-Amoretti (Snyder Laboratory)
Received an F31 award from the National Eye Institute for his research proposal titled “Characterizing Population Dynamics of Prefrontal Cortex which Govern the Modulation of Visual Processing”
Caitlin Sharp (Suarez-Jimenez Lab)
Has been selected to receive a fellowship from the AR/VR PhD training program to pursue her research characterizing how trauma exposure effects location-specific reward learning.
Mariah Marrero (Gelbard Lab) & Dominic Bunn (Johnson Lab)
Both were accepted into the University of Rochester Aging and Alzheimer’s Disease Training Program (UR-AADTP)
Niki Lam (1st year NGP) & Nicole Popp (1st Year NGP)
Niki and Nicole were appointed to the Neuroscience T32 Training Grant
Abigail Alpers (Hewitt/Gomez-Ramirez Labs) & Daulton Myers (Mitchell/Wang Labs)
Abi and Daulton were reappointed to the Neuroscience T32 Training Grant
Debra Cory-Slechta Explains How Wildfire Smoke and Air Pollution can Harm the Brain
Thursday, August 3, 2023
In an interview with Rick Woychik, director of the National Institute of Environmental Health Sciences, the professor of Environmental Medicine shares how research into how fine air particles impact the brain is transforming our understanding of neurodegenerative and neurodevelopmental disorders. Woychik interviewed Cory-Slechta after seeing her presentation at the first Human Health and the Environment Research Symposium at the Medical Center in June, where he was a guest speaker.
Read More: Debra Cory-Slechta Explains How Wildfire Smoke and Air Pollution can Harm the BrainURMC researcher receives $8.3 million to study chronic pain and the brain
Wednesday, July 19, 2023
Understanding the role of chronic pain in the brain could transform treatment and care for a condition that inflicts more than 20 percent of US adults. Paul Geha, MD, associate professor of Psychiatry has been studying the correlation between brain structure and chronic pain and was recently awarded $8.3 million from the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) to continue this work in understanding the link between pain and the brain.
His previous research found a possible explanation to why people with chronic pain often struggle with their weight. The research published in PLOS ONE suggests that circuitry in the brain responsible for motivation and pleasure is impacted when someone experiences pain, changing their brain’s response to fat and brain scans showed disrupted satiety signals.
“Our ongoing research focuses on unraveling the mechanisms underlying pain perception in the brain, as well as utilizing brain circuitries to gain insights into the pathophysiology of chronic pain. Additionally, we aim to develop quantitative biomarkers that can be derived from natural language processing of patients' pain narratives and multimodal brain imaging,” said Geha. “These biomarkers hold the potential to predict clinical outcomes in patients, including response to analgesics or the long-term persistence or remission of pain.”
Read More: URMC researcher receives $8.3 million to study chronic pain and the brainTrading Sickness for Health: Swapping Brain Cells Points to New Huntington's Therapies
Monday, July 17, 2023
New research appearing in the journal Nature Biotechnology answers important questions about the viability of treatments that seek to replace diseased and aged cells in the central nervous system with healthy ones. Its findings have implications for a number of neurological and psychiatric disorders—including Huntington’s disease, amyotrophic lateral sclerosis (ALS), and schizophrenia—that have been linked to glia, a population of cells that support brain health and function.
“A broad variety of disorders we associate with neuronal loss now appear to be caused by dysfunctional glial cells,” said Steve Goldman, MD, PhD, co-director of the Center for Translational Neuromedicine at the University of Rochester lead author of the new study. “This makes these diseases attractive targets for stem and progenitor cell-based therapies.”
The new study describes the ability of human glial progenitor cells–precursor cells that can give rise to both astrocytes and oligodendrocytes, the two major types of glia—to compete with one another in the adult brain, and the competitive advantage of young and healthy cells over aged and diseased cells.
Read More: Trading Sickness for Health: Swapping Brain Cells Points to New Huntington's TherapiesAn Unexpected Doorway into the Ear Opens New Possibilities for Hearing Restoration
Wednesday, June 28, 2023
An international team of researchers led by the co-director of the Center for Translational Neuromedicine developed a new method to deliver drugs into the inner ear. It harnesses the natural flow of fluids in the brain and employs a little-understood back door into the cochlea.
Read More: An Unexpected Doorway into the Ear Opens New Possibilities for Hearing RestorationAnders Jahre Main Award for Medical Research given to Maiken Nedergaard
Tuesday, June 13, 2023
The professor of Neurology and co-director of the Center for Translational Neuromedicine at the University of Rochester and University of Copenhagen received the award from the University of Oslo. Nedergaard was recognized for her research on astrocytes and the glymphatic system, which "has far-reaching implications both for understanding how the brain normally works and what goes wrong when the brain is affected by disease."
Read More: Anders Jahre Main Award for Medical Research given to Maiken NedergaardA chance observation finds potential hearing biomarker for Alzheimer’s disease
Wednesday, June 7, 2023
Science lends itself to questions, changing hypotheses, and chance findings. Recently, in the White Lab at the Del Monte Institute for Neuroscience at the University of Rochester, Neuroscience graduate student Daxiang Na was reviewing data for one project but instead uncovered something unexpected. He discovered that where plaques associated with Alzheimer’s disease are found in the brain may contribute to hearing loss.
Na was conducting hearing tests on mice with amyloid beta, the main component of protein plaques and tangles found in Alzheimer’s. While looking at two different transgenic mouse models of the disease, he found for one model, called 5xFAD, the older mice had hearing changes similar to what is found in people with Alzheimer’s disease. The other model did not demonstrate these hearing changes, nor did younger mice in the 5xFAD group.
“It was a chance observation,” said Na, who is first author of a paper with these findings in Frontiers in Neuroscience. “Both mouse models had amyloid beta protein, but where we found the plaque varied, and that may be why hearing loss varied across the groups.”
Researchers found that the brains of older mice from both models had plaques in the hippocampus and auditory cortex. But the brain of mice with hearing changes also had a small amount of plaque on the auditory brainstem, suggesting this area may be sensitive to disruption from plaque found in Alzheimer’s. Researchers discovered that the plaque reduced the brainstem’s ability to coordinate responses to sound.
“This may explain why Alzheimer’s patients have auditory symptoms,” said Patricia White, PhD, professor of Neuroscience and senior author of the study. “We think the location of plaques may be more important to hearing decline. It could be a potential biomarker to track disease progression because it could be assessed with amyloid PET imaging. Our data also suggest that regular auditory Brainstem Response assessments could help with diagnosis.”
Read More: A chance observation finds potential hearing biomarker for Alzheimer’s diseaseResearch finds prediction may be key to eye-and-hand coordination
Monday, June 5, 2023
Have you ever made a great catch—like saving a phone from dropping into a toilet or catching an indoor cat from running outside? Those skills—the ability to grab a moving object—takes precise interactions within and between our visual and motor systems. Researchers at the Del Monte Institute for Neuroscience at the University of Rochester have found that the ability to visually predict movement may be an important part of the ability to make a great catch—or grab a moving object.
“We were able to develop a method that allowed us to analyze behaviors in a natural environment with high precision, which is important because, as we showed, behavioral patterns differ in a controlled setting,” said Kuan Hong Wang, PhD, a Dean’s Professor of Neuroscience at the University of Rochester Medical Center. Wang co-led the study out today in Current Biology with Jude Mitchell, PhD, assistant professor of Brain and Cognitive Sciences at the University of Rochester. “Understanding how natural behaviors work will give us better insight into what is going awry in an array of neurological disorders.”
Read More: Research finds prediction may be key to eye-and-hand coordinationResearchers: Early alcohol exposure does not change connection between brain’s immune system and neurons that send information related to functions like balance and memory (UPDATE)
Monday, May 8, 2023
Research out of the Majewska Lab at the Del Monte Institute for Neuroscience at the University of Rochester continues to show the brain’s immune system does not play a significant role in the neurological damage that occurs in fetal alcohol spectrum disorders (FASD).
A new study out in Frontiers in Neuroscience investigated the interaction between microglia and Purkinje neurons—the neurons responsible for sending information from the cerebellum. Researchers found mice exposed to ethanol during development had no differences in microglia movement or structure and only subtle changes in the interaction between microglia and Purkinje neurons. “It appears that developmental ethanol exposure has little effect on microglia later in life,” said MaKenna Cealie, a Neuroscience graduate student in the lab and first author of the paper. “We believe examining other cell types and their interactions may be an important direction for future FASD studies to take.”
Other authors include the senior author Ania Majewska, PhD, Linh Le, Erik Vonkaenel, and Matthew McCall, PhD, of the University of Rochester Medical Center, and James Douglas and Paul Drew, PhD, of the University of Arkansas Medical Center.
The research was supported by the National Institutes of Health (NIH), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and the University of Rochester Intellectual and Developmental Disabilities Research Center (UR-IDDRC).
Read More: Researchers: Early alcohol exposure does not change connection between brain’s immune system and neurons that send information related to functions like balance and memory (UPDATE)Halting the Rise of Parkinson’s
Monday, April 24, 2023
Quality of life, health, and longevity are being increasingly tied to someone’s zip code rather than their genetic code. Cancer, heart disease, neurodegenerative disorders, and even our ability to fight infection are linked to the myriad of chemicals we are exposed to, often unwittingly, over the course of our lives. The University of Rochester’s leadership in the field of environmental medicine stretches back to toxicology research programs developed at the University under the Manhattan Project. These programs also served as the basis for the formation of a NIEHS Center of Excellence in environmental toxicology and health that is one of the oldest in the country celebrating 50 years of sustained funding. This foundation and the decades of work that followed—coupled with the recognition that the public health threat requires a collaborative commitment to research, education, and community engagement—led to the creation of the new Institute for Human Health and the Environment.
Paige Lawrence, PhD, the Wright Family Research Professor and chair of the Department of Environmental Medicine, is the founding director of the new Institute. “Genetics only explaining 10 to 15 percent of human health, which leaves the rest to the environment,” said Lawrence. “If we really want to have an impact on health, environmental influences need to be front and center.”
The new Institute will help power a team of neurologists, neuroscientists, toxicologists, epidemiologists, and researchers at the University of Rochester who are examining the impact of environmental chemical exposure on the brain. One disease in particular stands out. Parkinson’s is the fastest growing neurodegenerative disease in the world, outpacing even Alzheimer’s, and a growing number of scientists are linking the disease’s rise to air pollution, pesticides, and a ubiquitous chemical pollutant.
Up the nose it goes
Air pollution is associated with many health problems, including asthma, heart disease, stroke, low birth weight, and inflammation. While epidemiological studies have hinted at the link between air pollution and neurological disorders like Parkinson’s and Alzheimer’s, the route these chemicals use to make their way into the brain, and the damage caused once there, was until recently poorly understood.
“We’ve known that air pollution has effects on the heart and the lung for a very long time, but it's really only been in about the past ten years that attention has been directed to its effects on the brain,” said Debbie Cory-Slechta, PhD, a professor of Environmental Medicine, Neuroscience, and Public Health Sciences. Cory-Slechta’s colleagues at the University of Rochester, Guenter Oberdoerster, PhD, and Alison Elder, PhD, were among the first to show that ultra-fine air pollution particles, called PM0.1, are able to hitch a ride directly into the brain via the nasal passage and olfactory nerves, bypassing the brain’s normal defenses.
Read More: Halting the Rise of Parkinson’sIan Fiebelkorn finds rhythmic brain activity helps to maintain temporary memories
Monday, April 24, 2023
New research shows that rhythmic brain activity is key to temporarily maintaining important information in memory. Researchers at the Del Monte Institute for Neuroscience at the University of Rochester published these findings today in Current Biology that found brain rhythms—or patterns of neuronal activity—organize the bursts of activity in the brain that maintain short-term connections.
“The thought has been that the temporary storage of important information is linked to neurons in the brain that just fire away, retaining that information until it is no longer needed. Recent research has shown that it might not be such persistent brain activity that matters most for the temporary storage of information, but rather a short-term strengthening of the connections between neurons that are representing the information. Our research shows that brain rhythms are organizing these transient bursts over time,” said Ian Fiebelkorn, PhD, assistant professor of Neuroscience and senior author of the study. “The rhythmic coordination of brain activity over time is important because it allows overlapping populations of neurons to store different pieces of information at the same time.”
Fiebelkorn’s previous research around how the brain processes external information—like when navigating Times Square in New York City—made a similar discovery. He and fellow researchers found that brain rhythms help to coordinate different functions associated with either sampling presently important information or shifting to another source of information. In this context, brain rhythms help to balance focus on the task at hand with being prepared for the unexpected.
Read More: Ian Fiebelkorn finds rhythmic brain activity helps to maintain temporary memories2023 Edward Peck Curtis Award Recipient - Linh Le
Friday, April 14, 2023
The Edward Peck Curtis Awards for graduate student teaching are given to a small number of full-time graduate students who have a role in undergraduate education. Recipients have assisted in undergraduate instruction, and have had significant face-to-face interaction with undergraduates in the classroom or laboratory.
Winners are selected by the vice provost and University dean of graduate studies based on nominations from individual departments or undergraduate student groups.
If you have questions about the award, please contact the Office of Graduate Education
Congratulations Linh!!!
Possible ‘steps’ to revealing super-agers
Thursday, April 13, 2023
On the quest for the proverbial fountain of youth, scientists have long looked for evidence of super-agers—people whose brain ages slower than their body. Researchers at the Del Monte Institute for Neuroscience at the University of Rochester have found older adults whose brain performance improves when they combine a cognitive task with walking.
“Identifying super-agers will leverage what we understand about the brain and aging,” said Eleni Patelaki, a Biomedical Engineering PhD student at the University of Rochester Medical Center and first author of the paper out today in NeuroImage. “But this is difficult to do because, in this case, there was no external evidence of this ability, and people are unaware that their brain is working differently.
Walking and doing exposes brain flexibility
Researchers had the participants complete the same cognitive task while sitting and while walking. The 37 men and women, ages 62 to 79, scored similarly while sitting. When the same group repeated the test while walking, researchers found some individuals improved their cognitive performance. Researchers used Mobile Brain/Body Imaging (MoBI) to observe these changes and measure how the brain responded to the dual task. “We think this brain activity might constitute signatures of ‘super-aging,” said Patelaki. “We were able to find seven people, and now that we know where and how to look in the brain to find these super-agers, we can find more.”
The participants whose cognition improved while walking showed that their brain was able to adapt to and improve at the task—it had flexible usage of certain frontal resources. But those same people lost their flexibility in using the rest of their neural resources, similar to their peers who did not improve at the task while walking. This suggests that the brain’s ability to adapt or its flexibility in reallocating neural resources while walking might be an important factor in protecting cognition as we age.
Read More: Possible ‘steps’ to revealing super-agersThe stars in the brain may be information regulators
Friday, March 31, 2023
URMC researcher, Nathan A. Smith,MS, PhD, explores how astrocytes may be a key player in the brain’s ability to process external and internal information simultaneously. He argues research on these cells is necessary to understand their role in the process that allows a person to have an appropriate behavioral response and also the ability to create a relevant memory to guide future behavior.
Read More: The stars in the brain may be information regulatorsIron & the brain: Where and when neurodevelopmental disabilities may begin during pregnancy
Monday, March 6, 2023
Study finds possible cellular origin for impairments associated with gestational iron deficiency
The cells that make up the human brain begin developing long before the physical shape of the brain has formed. This early organizing of a network of cells plays a major role in brain health throughout the course of a lifetime. Numerous studies have found that mothers with low iron levels during pregnancy have a higher risk of giving birth to a child that develops cognitive impairments like autism, attention deficit syndrome, and learning disabilities. However, iron deficiency is still prevalent in pregnant mothers and young children.
The mechanisms by which gestational iron deficiency (GID) contributes to cognitive impairment are not fully understood. The laboratory of Margot Mayer- Proschel, PhD, a professor of Biomedical Genetics and Neuroscience at the University of Rochester Medical Center, was the first to demonstrated that the brains of animals born to iron-deficient mice react abnormally to excitatory brain stimuli, and that iron supplements giving at birth does not restore functional impairment that appears later in life. Most recently, her lab has made a significant progress in the quest to find the cellular origin of the impairment and have identified a new embryonic neuronal progenitor cell target for GID. This study was recently published in the journal Development.
“We are very excited by this finding,” Mayer-Proschel said, who was awarded a $2 million grant from the National Institute of Child Health & Human Development in 2018 to do this work. “This could connect gestational iron deficiency to these very complex disorders. Understanding that connection could lead to changes to healthcare recommendations and potential targets for future therapies.”
Read More: Iron & the brain: Where and when neurodevelopmental disabilities may begin during pregnancySmall, involuntary eye movements help us see a stable world
Thursday, February 23, 2023
Our eyes are never at rest. Instead, they remain in motion, even between our voluntary gaze shifts, through fixational eye movements—small, continuous movements of the eye that we are not aware of making.
Scientists have long sought to understand how we humans can perceive the world as stable as our eyes are constantly moving. Past research has suggested that, in the intervals between voluntary gaze shifts, the human visual system builds a picture of a stable world by relying solely on sensory inputs from fixational eye movements. According to new research by a team at Rochester, however, there may be another contributing factor.
In a paper published in Nature Communications, the researchers—including Michele Rucci, a professor of brain and cognitive sciences and, and first author Zhetuo Zhao, a PhD student in Rucci’s lab—report that the visual system not only receives sensory inputs from fixational eye movements but also possesses knowledge of the motor behavior involved in those movements.
Read More: Small, involuntary eye movements help us see a stable worldCan hearing loss be reversed? Research in Patricia White's lab reveals clues that could regrow the cells that help us hear
Monday, February 13, 2023
Taking a bite of an apple is considered a healthy choice. But have you ever thought about putting in earplugs before your favorite band takes the stage?
Just like your future body will thank you for the apple, your future ears (specifically your cochlear hair cells) will thank you for protecting them. The most common cause of hearing loss is progressive because these hair cells—the primary cells to detect sound waves—cannot regenerate if damaged or lost. People who have repeated exposure to loud noises, like military personnel, construction workers, and musicians, are most at risk for this type of hearing loss. But, it can happen to anyone over time (even concert goers).
On the other hand, birds and fish can regenerate these hair cells, and now researchers at the Del Monte Institute for Neuroscience are getting closer to identifying the mechanisms that may promote this type of regeneration in mammals, as explained in research recently published in Frontiers in Cellular Neuroscience.
 “We know from our previous work that expression of an active growth gene, called ERBB2, was able to activate the growth of new hair cells (in mammals), but we didn’t fully understand why,” said Patricia White, PhD, professor of Neuroscience and Otolaryngology at the University of Rochester Medical Center. The 2018 study led by Jingyuan Zhang, PhD, a postdoctoral fellow in the White lab at the time, found that activating the growth gene ERBB2 pathway triggered a cascading series of cellular events by which cochlear support cells began to multiply and activate other neighboring stem cells to become new sensory hair cells.
“We know from our previous work that expression of an active growth gene, called ERBB2, was able to activate the growth of new hair cells (in mammals), but we didn’t fully understand why,” said Patricia White, PhD, professor of Neuroscience and Otolaryngology at the University of Rochester Medical Center. The 2018 study led by Jingyuan Zhang, PhD, a postdoctoral fellow in the White lab at the time, found that activating the growth gene ERBB2 pathway triggered a cascading series of cellular events by which cochlear support cells began to multiply and activate other neighboring stem cells to become new sensory hair cells.
Read More: Can hearing loss be reversed? Research in Patricia White's lab reveals clues that could regrow the cells that help us hearResearchers identify neurons that "learn" to smell a threat
Tuesday, January 24, 2023
Whether conscious of it or not, when entering a new space, we use our sense of smell to assess whether it is safe or a threat. In fact, for much of the animal kingdom, this ability is necessary for survival and reproduction. Researchers at the Del Monte Institute for Neuroscience at the University of Rochester are finding new clues to how the olfactory sensory system aids in threat assessment and have found neurons that “learn” if a smell is a threat.

Julian Meeks, PhD
“We are trying to understand how animals interact with smell and how that influences their behavior in threatening social and non-social contexts,” said Julian Meeks, PhD, principal investigator of the Chemosensation and Social Learning Laboratory. “Our recent research gives us valuable tools to use in our future work and connects specific sets of neurons in our olfactory system to the memory of threatening smells.”
Read More: Researchers identify neurons that "learn" to smell a threatKerry O'Banion speaks with Medical News Today
Wednesday, January 18, 2023
Gut-brain connection: 3 fatty acids may be linked to tau-mediated damage
As the prevalence of Alzheimer’s disease (AD) continues to increase, the search for ways to treat and prevent it is ever more pressing. Newly licensed treatments, such as aducanumab and lecanemab, that clear beta-amyloidTrusted Source from the brain are a positive development, but they are expensive and controversial.
Many researchers are now focusing on other areas, one of which is the effect of the microbiomeTrusted Source — microbes, particularly bacteria, that inhabit the gut — on neurodegenerative disorders.
. "There is growing recognition of a gut-brain axis and evidence that the microbiome of individuals varies with disease status," said O'Banion. "The biggest issue is understanding whether gut changes are due to disease or contribute to disease (or both)."
Read More: Kerry O'Banion speaks with Medical News TodayMaiken Nedergaard's lab just discovered a new part of the brain's waste disposal system
Thursday, January 5, 2023
New Scientist, January 5
The new structure is a fourth membrane, lying on top of the innermost membrane, called the subarachnoid lymphatic-like membrane (SLYM). The SLYM hadn’t been noticed before, partly because the membrane disintegrates when the brain is removed from the skull in post-mortems, says Maiken Nedergaard, a professor of neurology and of neurosurgery and codirector of the Center for Translational Neuromedicine, who helped discover the structure. It is also too thin to be seen in living people via brain-scanning machines.
Read More: Maiken Nedergaard's lab just discovered a new part of the brain's waste disposal systemNewly Discovered Anatomy Shields and Monitors Brain
Thursday, January 5, 2023
From the complexity of neural networks to basic biological functions and structures, the human brain only reluctantly reveals its secrets. Advances in neuro-imaging and molecular biology have only recently enabled scientists to study the living brain at level of detail not previously achievable, unlocking many of its mysteries. The latest discovery, described today in the journal Science, is a previously unknown component of brain anatomy that acts as both a protective barrier and platform from which immune cells monitor the brain for infection and inflammation.
The new study comes from the labs of Maiken Nedergaard, co-director of the Center for Translational Neuromedicine at University of Rochester and the University of Copenhagen and Kjeld Møllgård, M.D., a professor of neuroanatomy at the University of Copenhagen. Nedergaard and her colleagues have transformed our understanding of the fundamental mechanics of the human brain and made significant findings in the field of neuroscience, including detailing the many critical functions of previously overlooked cells in the brain called glia and the brain’s unique process of waste removal, which the lab named the glymphatic system.
“The discovery of a new anatomic structure that segregates and helps control the flow of cerebrospinal fluid (CSF) in and around the brain now provides us much greater appreciation of the sophisticated role that CSF plays not only in transporting and removing waste from the brain, but also in supporting its immune defenses,” said Nedergaard.
The study focuses on the series of membranes that encase the brain, creating a barrier from the rest of the body and keeping the brain bathed in CSF. The traditional understanding of what is collectively called the meningeal layer identifies the three individual layers as dura, arachnoid, and pia matter.
Read More: Newly Discovered Anatomy Shields and Monitors Brain