Neuroscience News from the UR Community
20222021202020192018
Mini Strokes Can Cause Brain Damage, Lead To Dementia And Cognitive Impairment: Study
Thursday, December 13, 2012
Chances are if you're a senior managing your health, you've already had a conversation with your doctor about stroke risk. While many patients know the warning signs of stroke -- slurred speech, weakness on one side of the body, coordination problems, double vision, and headaches -- health care providers often fail to educate patients about their risk for silent or mini-strokes,
which can cause progressive, permanent damage and lead to dementia.
A new study published in the Journal of Neuroscience, examined the effects of these so-called mini-strokes. They frequently are not diagnosed or detected by a doctor because a patient does not immediately present with stroke signs. Mini-strokes may lead to permanent neurological damage and increase risk for full blown stroke.
Maiken Nedergaard, MD, lead author of the study and professor of neurosurgery at the University of Rochester Medical Center, says at least half of individuals over the age of 60 will experience one mini-stroke in their lifetime. She calls the prevalence of mini-strokes "an epidemic."
Study Questions Validity of Quality Measure for Stroke Care
Monday, August 27, 2012
One of the key indicators of the quality of care provided by hospitals to acute stroke victims is the percentage of patients who die within a 30-day period. A new study shows that the decisions made by patients and their families to stop care may account for as many as 40 percent of these stroke-related deaths, calling into question whether it is a valid measure of a hospital’s skill in providing stroke care.
The study, which appears today in the journal Neurology, focuses on a quality measure proposed by the federal Centers for Medicaid and Medicare Services called the 30-day risk adjusted stroke mortality. While the measure is being developed as a part of federal health care reform, it is already commonly employed as an indicator of a hospital’s quality of care on websites that evaluate hospital performance.
"It is clear that a significant component of the overall mortality score as currently constructed does not tell the whole story and is predicated on the preference of patients and their families," said University of Rochester Medical Center (URMC) neurologist Adam Kelly, M.D., lead author of the study.
Scientists Discover Previously Unknown Cleansing System in Brain
Wednesday, August 15, 2012
A previously unrecognized system that drains waste from the brain at a rapid clip has been discovered by neuroscientists at the University of Rochester Medical Center. The findings were published online August 15 in Science Translational Medicine.
The highly organized system acts like a series of pipes that piggyback on the brain's blood vessels, sort of a shadow plumbing system that seems to serve much the same function in the brain as the lymph system does in the rest of the body -- to drain away waste products.
"Waste clearance is of central importance to every organ, and there have been long-standing questions about how the brain gets rid of its waste," said Maiken Nedergaard, M.D., D.M.Sc., senior author of the paper and co-director of the University's Center for Translational Neuromedicine. "This work shows that the brain is cleansing itself in a more organized way and on a much larger scale than has been realized previously.
"We're hopeful that these findings have implications for many conditions that involve the brain, such as traumatic brain injury, Alzheimer's disease, stroke, and Parkinson's disease," she added.
New Huntington’s Treatment Shows Promise
Wednesday, July 18, 2012
A new study shows that the compound Coenzyme Q10 (CoQ) reduces oxidative damage, a key finding that hints at its potential to slow the progression of Huntington disease. The discovery, which appears in the inaugural issue of the Journal of Huntington’s Disease, also points to a new biomarker that could be used to screen experimental treatments for this and other neurological disorders.
"This study supports the hypothesis that CoQ exerts antioxidant effects in patients with Huntington’s disease and therefore is a treatment that warrants further study," says University of Rochester Medical Center neurologist Kevin M. Biglan, M.D., M.P.H., lead author of the study. "As importantly, it has provided us with a new method to evaluate the efficacy of potential new treatments."
Huntington’s disease is a genetic, progressive neurodegenerative disorder that impacts movement, behavior, cognition, and generally results in death within 20 years of the disease’s onset. While the precise causes and mechanism of the disease are not completely understood, scientists believe that one of the important triggers of the disease is a genetic "stutter" which produces abnormal protein deposits in brain cells. It is believed that these deposits – through a chain of molecular events – inhibit the cell’s ability to meet its energy demands resulting in oxidative stress and, ultimately, cellular death.
'Goldilocks Effect': Babies Learn When Things Aren't Too Complex, Too Simple
Thursday, May 24, 2012
Not too simple and not too complicated: Babies focus their attention on situations that are just right,
according to a new study published in the journal PLoS ONE.
Researchers from the University of Rochester coined this type of engagement the "Goldilocks effect." They proposed babies take in information that is not too predictable, but not too complicated by focusing on sights, sounds and movements.
The study showed that infants are active seekers of information rather than passive recipients, and they, therefore, adjust how they attend to visual information by avoiding overly simple and overly complex events in their world,
said Richard Aslin, professor of brain and cognitive sciences at the University of Rochester Medical Center and co-author of the study. They seek information that is of intermediate complexity, presumably because that is the best way to learn from the environment.
Grant to Improve Training for Professionals Caring for Those with Alzheimer’s Disease
Tuesday, May 22, 2012
The Finger Lakes Geriatric Education Center (FLGEC) at the University of Rochester Medical Center was awarded grant funds to enhance training and education for professionals who assess and care for people with Alzheimer's Disease.
FLGEC earned a Supplemental Funding Grant for Education from the Health Resources and Services Administration. Funding consists of approximately $135,000 over two years, made possible through the federal National Alzheimer's Project Act. The award will help FLGEC develop additional training that incorporates new materials and information developed under the National Plan to Address Alzheimer's Disease, including guidelines for care and new screening and assessment tools.
FLGEC is led by Jurgis Karuza, Ph.D., is program director, and Thomas Caprio, M.D., M.P.H., Project Co-Director.
University Life Trustee, Neurosciences Benefactor Ernest J. Del Monte Dies
Monday, April 23, 2012
Ernest J. Del Monte, 87, real estate and hotel developer, philanthropist and University of Rochester Life Trustee, died Saturday, April 21, 2012. His generosity to the University of Rochester leaves a legacy of innovation and collaboration to help eradicate brain diseases.
Mr. Del Monte, of Pittsford, was a visionary in business and industry. With a $10 million gift to the University in 2009, he and his wife, Thelma, helped establish the E.J. Del Monte Neuromedicine Institute to expand the study and treatment of Alzheimer's disease, stroke, spinal cord and brain injuries, and brain cancers at the University of Rochester Medical Center.
The gift was the catalyst for the establishment of the Del Monte Neuromedicine Institute, which serves as an umbrella for several vibrant research centers and growing clinical care programs throughout the Medical Center and River Campus. It has also reinvigorated the scientists and physicians who treat patients with neurological conditions.
Ernie was a force of nature who touched so many of our lives at the University. I am proud to have spent time with him and his late wife, Thelma, and continue to be deeply moved by his commitment to the Del Monte Neuromedicine Institute. When I last spoke with him, he was still planning deals, always imaginative, always determined, right up to the end,
said Joel Seligman, president of the University of Rochester.
Autism Research Being Funded Through Novel Platform
Wednesday, April 11, 2012
Stephen McAleavey, Associate Professor in Biomedical Engineering
and Daniel Mruzek, Assistant Professor of the Department of
Behavioral Pediatrics have recently submitted an
Autism project for sponsorship on a new platform called
Innovocracy. The University of Rochester
recently signed up as an Innovocracy Launch Partner and the Autism project has already raised 172% of its funding goal from
individual donors within the first few days. The Innovocracy platform allows the aggregation of small donations to help
propel innovative research in the support of proof-of-concept projects. Supporters include everyone from alumni, friends
and family to the general public interested in autism research. This collaboration was initiated through an undergraduate
Senior Design project, and subsequently received
CTSI pilot funds
for further development and early clinical evaluation.
Once Considered Mainly ‘Brain Glue,’ Astrocytes’ Power Revealed
Thursday, March 29, 2012
A type of cell plentiful in the brain, long considered mainly the stuff that holds the brain together and oft-overlooked by scientists more interested in flashier cells known as neurons, wields more power in the brain than has been realized, according to new research published today in Science Signaling.
Neuroscientists at the University of Rochester Medical Center report that astrocytes are crucial for creating the proper environment for our brains to work. The team found that the cells play a key role in reducing or stopping the electrical signals that are considered brain activity, playing an active role in determining when cells called neurons fire and when they don't.
That is a big step forward from what scientists have long considered the role of astrocytes -- to nurture neurons and keep them healthy.
"Astrocytes have long been called housekeeping cells -- tending to neurons, nurturing them, and cleaning up after them," said Maiken Nedergaard, M.D., D.M.Sc., professor of Neurosurgery and leader of the study. "It turns out that they can influence the actions of neurons in ways that have not been realized."
‘Brain Fog’ of Menopause Confirmed
Wednesday, March 14, 2012
The difficulties that many women describe as memory problems when menopause approaches are real, according to a study published today in the journal Menopause, the journal of the North American Menopause Society.
The findings won't come as a surprise to the millions of women who have had bouts of forgetfulness or who describe struggles with "brain fog" in their late 40s and 50s. But the results of the study, by scientists at the University of Rochester Medical Center and the University of Illinois at Chicago who gave women a rigorous battery of cognitive tests, validate their experiences and provide some clues to what is happening in the brain as women hit menopause.
"The most important thing to realize is that there really are some cognitive changes that occur during this phase in a woman's life," said Miriam Weber, Ph.D., the neuropsychologist at the University of Rochester Medical Center who led the study. "If a woman approaching menopause feels she is having memory problems, no one should brush it off or attribute it to a jam-packed schedule. She can find comfort in knowing that there are new research findings that support her experience. She can view her experience as normal."
Taking another Shot at RAGE to Tame Alzheimer's
Wednesday, March 14, 2012
Benjamin Miller, Ph.D., and Itender Singh, Ph.D.
Researchers have taken another crack at a promising approach to stopping Alzheimer's disease that encountered a major hurdle
last year. In research published this week in the Journal of Clinical Investigation,
scientists have developed a compound that targets a molecular actor known as RAGE,
which plays a central role in mucking up the brain tissue of people with the disease.
Scientists at the University of Rochester Medical Center and the University of Southern California synthesized a compound that stops
RAGE in mice - reversing amyloid deposits, restoring healthy blood flow in the
brain, squelching inflammation, and making old, sick mice smarter. But the scientists caution that the work has a long way to go before it's
considered as a possible treatment in people.
In the latest work, Zlokovic and colleagues screened thousands of compounds for
anti-RAGE activity and identified three that seemed promising. Then the team turned
to chemists Benjamin Miller, Ph.D., and graduate student Nathan Ross. The pair analyzed the compounds' molecular
structures, then used that knowledge to create dozens of candidates likely to have activity against RAGE.
A Step Forward In Effort to Regenerate Damaged Nerves
Tuesday, February 21, 2012
Thriving DRG cells
The carnage evident in disasters like car wrecks or wartime battles is oftentimes mirrored within the bodies of the people involved. A severe wound can leave blood vessels and nerves severed, bones broken, and cellular wreckage strewn throughout the body – a debris field within the body itself.
It's scenes like this that neurosurgeon Jason Huang, M.D., confronts every day. Severe damage to nerves is one of the most challenging wounds to treat for Huang and colleagues. It's a type of wound suffered by people who are the victims of gunshots or stabbings, by those who have been involved in car accidents – or by soldiers injured on the battlefield, like those whom Huang treated in Iraq.
Now, back in his university laboratory, Huang and his team have taken a step forward toward the goal of repairing nerves in such patients more effectively. In a paper published in the journal PLoS One, Huang and colleagues at the University of Rochester Medical Center report that a surprising set of cells may hold potential for nerve transplants.
Nerve Cells Key to Making Sense of Our Senses
Monday, November 21, 2011
The human brain is bombarded with a cacophony of information from the eyes, ears, nose, mouth and skin. Now a team of scientists at the University of Rochester, Washington University in St. Louis, and Baylor College of Medicine has unraveled how the brain manages to process those complex, rapidly changing, and often conflicting sensory signals to make sense of our world.
The study, published online Nov. 20 in Nature Neuroscience, represents the first direct evidence of how the brain combines multiple sources of sensory information to form as accurate a perception as possible of its environment, the researchers report.
The discovery may eventually lead to new therapies for people with Alzheimer's disease and other disorders that impair a person's sense of self-motion, says study coauthor Greg DeAngelis, professor and chair of Brain and Cognitive Sciences at the University of Rochester. This deeper understanding of how brain circuits combine different sensory cues could also help scientists and engineers to design more sophisticated artificial nervous systems such as those used in robots, he adds.
Autistic Children May Have Too Many Brain Cells, Study Says
Tuesday, November 8, 2011
The brains of autistic children have far more neurons in the prefrontal cortex than the brains of kids without autism, finds a new study that could advance research into the disorder. For the first time, we have the potential to understand why autism gets started,
said study author Eric Courchesne, a professor of neurosciences at the University of California, San Diego School of Medicine and director of the Autism Center of Excellence.
The prefrontal cortex is key to complex thoughts and behaviors, including language, social behavior and decision-making. The dorsolateral prefrontal cortex is closely linked with executive function,
including planning, reasoning and very high level cognition,
said Lizabeth Romanski, an associate professor of Neurobiology & Anatomy at the University of Rochester Medical Center, who was not involved with the research. The medial prefrontal cortex is thought to be important to social and other behavior and emotions.
Neurologist’s Talk Aimed at Parkinson’s Patients, Caregivers
Thursday, October 13, 2011
A physician who specializes in treating patients with Parkinson's disease and related disorders will speak about the condition and take questions from patients, family members and caregivers in a free public talk next week.
Michelle Burack, M.D., Ph.D., a neurologist at the University of Rochester Medical Center, will speak from 9:30 to 11 a.m. Thursday, Oct. 20, at Lifetime Care, 3111 S. Winton Road. The discussion is aimed especially at patients who have recently been diagnosed with Parkinson's, along with family members, though all are welcome.
The talk is part of a series of public discussions Burack has initiated across New York State, as part of educational outreach efforts through the Parkinson Support Group of Upstate New York. The talks are a way for Burack, who is part of a medical team that treats hundreds of patients with the disease, to educate people about Parkinson's and at the same time learn more about the disease, enabling her to treat patients more effectively. Three talks per year in the Rochester area are planned.
Precision with Stem Cells a Step Forward for Treating M.S., Other Diseases
Thursday, October 13, 2011
Areas in red indicate mouse brain cells coated with myelin, a crucial substance lacking in patients with M.S.
A diverse group of scientists -- experts in cardiology, neurology, immunology, microbiology and chemistry -- are teaming up to study drugs that show promise in the treatment of dementia for the treatment of an equally debilitating disease -- heart failure. In this case, the connection between the head and the heart lies in a particular enzyme that they believe plays a role in the development of both conditions.
The team, headed by Burns C. Blaxall, Ph.D., Harris A. "Handy" Gelbard, M.D., Ph.D., and Stephen Dewhurst, Ph.D., recently won the largest grant awarded to date by the University's Clinical and Translational Science Institute (CTSI) -- $250,000 over two years. The grant, part of the CTSI's newly initiated Incubator Program, is larger than most awarded by the Medical Center.
Thomas Pearson, M.D., Ph.D., who heads the CTSI and helped develop the new program, says tremendous weight was given to forming new teams that had never worked together before, and for these teams to study things they had never addressed before. The Blaxall/Gelbard/Dewhurst team fit the bill on both counts.
Has Your Brain Already Crystallized?
Tuesday, October 4, 2011
As it turns out, keeping pace in ever-more-electronic world is no small feat for the aging brain. That's because our mental circuitry – the most frequently used neuron pathways, like well-traveled roads – tends to crystallize
into a series of expressways over time. But that doesn't mean paving new paths (by, say, learning in middle age) is a lost cause – it just demands special learning techniques and a little more patience.
That's heartening news for adults who are headed back to school, shifting careers in later life, or simply want to be lifelong learners, says neuropsychologist Dr. Mark Mapstone. In the clip below, he sheds more light on our amazing (and aging) brains.
Stop Stroke Before it Stops You - 4 Things You Should Know
Tuesday, September 27, 2011
Ask any number of men what they think their odds of having a stroke are, and you might find many of them believe stroke is frighteningly unpredictable and can attack like a bolt from the blue – without warning, trailing death and disability in its wake.
That idea is dangerously wrong. The truth is that a stroke is the bullet at the end of a very long barrel and there is a lot you can do to dodge it.
The path to stroke can be started by heart disease – especially if you have an irregular heartbeat. It also can be started by arterial disease – especially if there is a build-up of plaque in the arteries of the neck. The chain of events that begins with cardiovascular disease and ends in stroke can take years, or even decades to evolve. You probably will not know that it is happening.
Need More Memory (No, We’re Not Talking RAM)
Tuesday, September 20, 2011
Searching frantically for misplaced car keys. Fumbling for the name of a new acquaintance. Providing an accurate eye-witness testimony. Treasuring past moments with a loved one lost. What, exactly, is this thing we call “memory”? How do our brains manage to process, store and recall so much sensory footage – even lifeless data, like phone numbers – almost reflexively?
Neuropsychologist Dr. Mark Mapstone co-directs URMC's memory care clinic, which features a team of neurologists, psychiatrists, a geriatrician, a neuropsychologist, a psychometrician (expert in measuring psychological function), a social worker and a nurse practitioner. He weighs in on these and other burning questions in the clip below.
Stem Cell Efforts to Treat Neurological Disease Bolstered With $4.5 Million
Wednesday, September 7, 2011
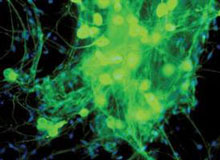
Human oligodendrocytes and astrocytes generated from human neural progenitor cells.
The endeavor to find better treatments or perhaps even one day a cure for a host of debilitating and fatal neurological diseases has been bolstered by an influx of funding from a mix of private and public sources.
he laboratory headed by Steven Goldman, M.D., Ph.D., chair of the Department of Neurology at the University of Rochester Medical Center, has received $4.5 million in new funding to further its efforts to use stem cells and related molecules to treat several feared disorders for which there are currently no cures – including multiple sclerosis, Huntington's disease, and fatal childhood diseases known as pediatric leukodystrophies.
Healthy Living: Batten Disease
Monday, August 29, 2011
Staring at a computer screen wasn't exactly what Nicole Newhouse envisioned for her career. It didn't take long for her to find a subject that sparked a new passion. Newhouse said, You have children that are dying. Point blank, you have children that are dying.
Newhouse is enrolling patients in the first controlled clinical trial for batten disease. We don't have a cure right now. We can't tell parents 'you take this and your child's going to be ok,
said Newhouse.
Batten disease is a neurological disorder that usually appears in children ages four to eight years old. Early symptoms of the disease include sudden vision problems. That's quickly followed by a loss of motor skills, mental impairment and eventually death. Try to imagine what it's like for the parents to watch their child basically dying before their eyes. Over many years, it's the kind of thing that as a physician you see and think you know I want to do something to help,
said Dr. Jonathan Mink, professor in the departments of Neurology, Neurobiology & Anatomy, Pediatrics, and Brain and Cognitive Sciences at the University of Rochester Medical Center.
Two Rochester Scientists among Top Parkinson Researchers
Wednesday, July 13, 2011
Two scientists at the University of Rochester Medical Center are among the world’s top researchers in the area of Parkinson disease, according to a recent study.
Karl Kieburtz, M.D., M.P.H., and Kim Tieu, Ph.D., are among the researchers cited in a recent study published last month in the Journal of Parkinson’s Disease. The study was done by Aaron Sorensen of GE Healthcare and publishing consultant David Weedon.
The study analyzed the number of times a scientist’s work has been cited by other scientists, the amount of new research that the person has published, and the ripple effect of the work in Parkinson disease as well as other areas.
Both Kieburtz and Tieu are among the 100 scientists whose work has been cited most during the last decade by other scientists doing research on the disease. Also on the list is Ira Shoulson, M.D., a former University of Rochester neurologist who is now at Georgetown. Altogether, research by the three was cited more than 6,500 times during the last decade by other scientists.
Neuroscientists Find Famous Optical Illusion Surprisingly Potent
Wednesday, June 29, 2011
Scientists have come up with new insight into the brain processes that cause an age-old illusion, first documented by Aristotle. The illusion is called the Motion Aftereffect by today's scientists, but why does it happen, though? Is it because we are consciously aware that the background is moving in one direction, causing our brains to shift their frame of reference so that we can ignore this motion? Or is it an automatic, subconscious response?
Davis Glasser, a doctoral student in the University of Rochester's Department of Brain and Cognitive Sciences thinks he has found the answer. The results of a study done by Glasser, along with his advisor, Professor Duje Tadin, and colleagues James Tsui and Christopher Pack of the Montreal Neurological Institute, will be published this week in the journal Proceedings of the National Academy of Sciences (PNAS). In their paper, the scientists show that humans experience the Motion Aftereffect even if the motion that they see in the background is so brief that they can't even tell whether it is heading to the right or the left.
Two Defective Proteins Conspire to Impair the Nerve Cell’s ‘Powerhouse’ in Alzheimer Disease
Friday, May 13, 2011
Two proteins that are abnormally modified in the brains of patients with Alzheimer disease collude, resulting in ill effects on the crucial energy centers of brain cells, according to new findings published online in Neurobiology of Aging. The research raises the possibility that pathological forms of two proteins, amyloid beta and tau, which make up the pathological hallmarks of the brains of Alzheimer patients – plaques and tangles – may work in tandem to decrease the survival of brain cells.
The idea that amyloid beta and tau may work together to cause mischief in the brain has been an evolving theme among scientists for a number of years,
said Gail Johnson, Ph.D., professor of Anesthesiology and the corresponding author of the paper. The precise relationship between the two pathologies is unclear, but there may be a synergy between the two when it comes to their effects on mitochondria in Alzheimer disease.
Iron Deficiency Pre-Conception And In Early Pregnancy Harms Developing Brain
Wednesday, March 23, 2011
A mother's iron deficiency early in pregnancy may have a profound and long-lasting effect on the brain development of the child, even if the lack of iron is not enough to cause severe anemia, according to a University of Rochester Medical Center study published in the scientific journal PLoS One.
The results are important because obstetricians might not notice or treat mild or moderate iron deficiency, and therefore the study authors believe their research underscores the need for monitoring a pregnant woman's iron status beyond anemia.
What convinced us to conduct the present study were our preliminary data suggesting that cells involved in building the embryonic brain during the first trimester were most sensitive to low iron levels,
said Margot Mayer-Proschel, Ph.D., the lead researcher and an associate professor of Biomedical Genetics at URMC.
Researchers Focus on Human Cells in Spinal Cord Injury Repair
Wednesday, March 2, 2011
For the first time, scientists discovered that a specific type of human cell, generated from stem cells and transplanted into spinal cord injured rats, provide tremendous benefit, not only repairing damage to the nervous system but helping the animals regain locomotor function as well.
The study, published today in the journal PLoS ONE, focuses on human astrocytes – the major support cells in the central nervous system – and indicates that transplantation of these cells represents a potential new avenue for the treatment of spinal cord injuries and other central nervous system disorders.
We’ve shown in previous research that the right types of rat astrocytes are beneficial, but this study brings it up to the human level, which is a huge step,
said Chris Proschel, Ph.D., lead study author and assistant professor of Genetics at the University of Rochester Medical Center. What’s really striking is the robustness of the effect. Scientists have claimed repair of spinal cord injuries in rats before, but the benefits have been variable and rarely as strong as what we’ve seen with our transplants.
To create the different types of astrocytes used in the experiment, researchers isolated human glial precursor cells, first identified by Margot Mayer-Proschel, Ph.D., associate professor of Genetics at the University of Rochester Medical Center, and exposed these precursor cells to two different signaling molecules used to instruct different astrocytic cell fate – BMP (bone morphogenetic protein) or CNTF (ciliary neurotrophic factor).
Study: African Americans Have Better Stroke Survival Rates
Monday, January 31, 2011
A study published today shows that African Americans have a better survival rate compared to whites after being hospitalized for a stroke. This conclusion contradicts prevailing wisdom and is one piece in a growing body of evidence that points to the important role that patients -- and the decision they and their families make in terms of treatment -- may play on mortality rates.
The study found that -- after adjusting data for variables such as age, socioeconomic status, and risk factors -- that African Americans who were hospitalized for acute ischemic stroke had a significantly lower mortality rate than whites. The survival advantage was most pronounced early after the stroke but persisted for up to one year. The study also found that African Americans were also more likely during their hospitalization to have received more aggressive treatment measures, such as kidney dialysis, a tracheostomy, or cardiopulmonary resuscitation. They were also less likely to use hospice care. These results were published today in the Annals of Internal Medicine.
"These results fly in the face of conventional wisdom that says that black patients with strokes have worse outcomes," said University of Rochester Medical Center neurologist Robert Holloway, M.D., M.P.H. a co-author of the study. "Even though we do not know the exact reasons for these differences, these data highlight the potential importance of treatment intensity, and the expression of patient preference for different treatments on survival and mortality. This is not such a far-fetched idea for physicians who take care of a lot of stroke patients."
Neuroscientist to Discuss Action Video Games as Learning Tool
Monday, January 10, 2011
Cognitive scientist Daphne Bavelier, Ph.D., will discuss her work using video games to explore the remarkable capacity of the brain to adapt as part of a lecture series highlighting biological and biomedical research at the University of Rochester.
Bavelier will discuss her research this Friday, Jan. 14, in the Class of '62 Auditorium (Room G-9425) at the Medical Center. The talk, part of the “Second Friday Science Social” lecture series, is geared mainly to faculty, staff and students at the University, though the general public is welcome as well.
Bavelier, professor of Brain and Cognitive Sciences, is an expert on the brain's ability to learn and adapt to an ever-changing environment. For the past decade, she has employed video games as a way to explore the brain's ability to adapt – a capability crucial for people trying to recover from a stroke or a traumatic brain injury or for people seeking to keep their mind as sharp as possible as they age.
The Pericyte Becomes a Player in Alzheimer’s, Other Neurodegenerative Diseases
Wednesday, November 17, 2010
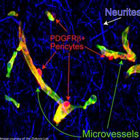
PDGFRβ+ Pericytes
Cells in the brain called pericytes that have not been high on the list of targets for treating diseases like Alzheimer's may play a more crucial role in the development of neurodegenerative diseases than has been realized. The findings, published Nov. 4 in Neuron, cast the pericyte in a surprising new role as a key player shaping blood flow in the brain and protecting sensitive brain tissue from harmful substances.
For 150 years these cells have been known to exist in the brain, but we haven't known exactly what they are doing in adults,
said Berislav Zlokovic, M.D., Ph.D., the neuroscientist who led the research at the University of Rochester Medical Center.
In the most recent findings from Zlokovic's laboratory, the two first authors who contributed equally to the research, graduate student Robert Bell and M.D./Ph.D. and Neuroscience student Ethan Winkler, teased out the role of the pericyte in the process. Pericytes ensheath the smallest blood vessels in the brain, wrapping around capillaries like ivy wrapping around a pipe and helping to maintain the structural integrity of the vessels.
How Some Brain Cells Hook Up Surprises Researchers
Tuesday, November 2, 2010

Marie-Ève Tremblay, Ph.D., and Ania Majewska, Ph.D.
Immune cells known as microglia, long thought to be activated in the brain only when fighting infection or injury, are constantly active and likely play a central role in one of the most basic, central phenomena in the brain -- the creation and elimination of synapses.
The finding, reported in the Nov. 2 issue of PloS Biology, catapults the humble microglia cell from its well-recognized duty of protecting the brain to direct involvement in creating the cellular networks at the core of brain behavior.
When scientists talk about microglia, the talk is almost always about disease. Our work suggests that microglia may actively contribute to learning and memory in the healthy brain, which is something that no one expected,
said Ania Majewska, Ph.D., assistant professor in the Department of Neurobiology & Anatomy who led the work.
The group's paper, co-authored by post-doctoral associate, Marie-Ève Tremblay, Ph.D., is a remarkably detailed look at how brain cells interact with each other and react to their environment swiftly, reaching out constantly to form new links or abolish connections.
Rochester Helps Lead Global Parkinson’s Study
Wednesday, October 6, 2010
Patients, doctors and nurses in Rochester will be a key part of a major national research study initiated by the Michael J. Fox Foundation to identify biomarkers to track the progression of Parkinson's disease in a precise way that is impossible to do today.
The study, known as the Parkinson's Progression Markers Initiative, seeks to fill a crucial gap: While doctors can generally predict the course that the disease takes in patients, there is no reliable, objective way to actually measure how the disease is progressing. A measure known as a biomarker, based on a biological measure that would be consistent among all patients, would help researchers measure the effectiveness of current treatments on their patients.
A reliable biomarker is also a critical tool to have in hand for scientists trying to identify new drugs to treat the disease. Currently there is no known biomarker for Parkinson's disease.
The study of approximately 600 people around the world will include up to 30 people at the University of Rochester Medical Center, which is one of 18 participating sites worldwide. The Rochester site is led by neurologist Irene Richard, M.D.
URMC Named Batten Disease Center of Excellence
Wednesday, May 12, 2010
The largest Batten Disease research and support organization in North America named the University of Rochester Medical Center as a Batten Disease Center of Excellence today. The Ohio-based organization, Batten Disease Support and Research Association, has chosen URMC because of its comprehensive services for patients and its long clinical and research history with the disease.
Batten Disease is a rare neurodegenerative syndrome that erupts with little warning. It first steals sight, then cripples cognitive and motor capacities, and while different variations of the disease brings a difference age of onset and progression, it is, ultimately, terminal. The most common form is juvenile, in which symptoms begin between 5 and 8 years of age. There are between 500 and 1,000 people with Batten Disease in the United States and only a few thousand in the world.
"Finding treatment with a comprehensive team that has experience with the disease is incredibly hard for families," said Jonathan Mink, M.D., Ph.D., chief of Child Neurology and professor of Neurology, Neurobiology & Anatomy and Pediatrics at URMC. "The Batten Disease Support and Research Association is hoping to streamline families' search for expertise by endorsing centers like ours."
Drug Shows Promise for Huntington’s Disease
Monday, February 8, 2010
An early stage clinical trial of the experimental drug dimebon (latrepirdine) in people with Huntington's disease appears to be safe and may improve cognition. That is the conclusion of a study published today in the Archives of Neurology.
This is the first clinical trial that has focused on what is perhaps the most disabling aspect of the disease,
said University of Rochester Medical Center neurologist Karl Kieburtz, M.D., the lead author of the study. While more investigation needs to be done, these results are encouraging and show, for the first time, a statistically significant benefit in terms of improved cognitive function in patients with Huntington's disease.
Huntington's disease is a progressive neurodegenerative disorder that impacts movement, behavior, cognition, and generally results in death within 20 years of the disease's onset. The disease steadily erodes a person's memory and their ability to think and learn. Over time, this cognitive impairment contributes to the loss of the ability to work and perform the activities of daily life. There are no treatments currently available that effectively alter the course of the disease or improve cognition.
New Multiple Sclerosis Drug has URMC Ties
Friday, January 22, 2010
The Food and Drug Administration has approved the drug fampridine-SR for the treatment of multiple sclerosis. Researchers at the University of Rochester Medical Center (URMC) have been evaluating the effects of the drug in MS for more than 10 years– it is the first medication shown to enhance some neurological functions in people with the disease – and their efforts helped pave the way for today’s action by the FDA.
“This is a good day for people who suffer from multiple sclerosis,” said Andrew Goodman, M.D., chief of the URMC Multiple Sclerosis Center. “Physicians will now have a new tool at their disposal that complements existing disease modifying therapies. For some patients, this drug will be a way to improve walking and help regain some independence in their daily lives.”
UR Study Reveals Chemo’s Toxicity to Brain, Possible Treatment
Thursday, December 17, 2009
Researchers have developed a novel animal model showing that four commonly used chemotherapy drugs disrupt the birth of new brain cells, and that the condition could be partially reversed with the growth factor IGF-1.
Published early online in the journal Cancer Investigation, the University of Rochester Medical Center study is relevant to the legions of cancer survivors who experience a frustrating decline in cognitive function after chemotherapy treatment, known as chemo brain.
"It is not yet clear how our results can be generally applied to humans but we have taken a very significant step toward reproducing a debilitating condition and finding ways to treat it," said Robert Gross, M.D., Ph.D., professor of Neurology and of Pharmacology and Physiology at URMC and principal investigator of the study.
Protein Regulates Movement of Mitochondria in Brain Cells
Monday, June 15, 2009
Scientists have identified a protein in the brain that plays a key role in the function of mitochondria – the part of the cell that supplies energy, supports cellular activity, and potentially wards off threats from disease. The discovery, which was reported today in the Journal of Cell Biology, may shed new light on how the brain recovers from stroke.
Understanding the molecular machinery that helps distribute mitochondria to different parts of the cell has only recently begun to be understood,
said University of Rochester Medical Center neurologist David Rempe, M.D., Ph.D., the lead author of the study. We know that in some disease states that mitochondria function is modified, so understanding how their activity is modulated is important to understanding how the brain responds to a pathological state.
Poor Sleep Quality Leads to Poorer Prognosis after Stroke
Tuesday, April 28, 2009
Stroke victims tend to do worse if they also have diagnosed or undiagnosed obstructive sleep apnea prior to having the stroke, according to a study presented April 28, 2009, at the American Academy of Neurology (AAN) annual meeting in Seattle.
Latha Stead, M.D., professor and chair of the Department of Emergency Medicine at the University of Rochester Medical Center, and professor of Neurosurgery, reported the findings at AAN, along with several other stroke studies measuring the factors that lead to a poor prognosis.
We know that obstructive sleep apnea has been linked to a multitude of cardiovascular problems, yet it is concerning that the vast majority of cases remain undiagnosed,
Stead said. In the context of recovering from a stroke, sleep apnea can have a serious impact, and for that reason we encourage people to become more aware of obstructive sleep apnea and to get treatment.
3 Events Offer Hope for People with Brain Tumors
Thursday, April 16, 2009
A PET scan allows doctors to see a brain tumor in an elderly man.
People with brain tumors, and those who love and care for them, will observe Brain Tumor Awareness Week with three educational and celebratory events sponsored by the University of Rochester Medical Center and James P. Wilmot Cancer Center.
On Friday, May 1, there will be a seminar for patients, their families, and physicians that focuses on the latest research and treatment approaches in brain and spinal tumors. Then on Thursday, May 7, patients, families and clinicians will gather for the Community Sharing Hope Picnic at Kings Bend Park in Pittsford. And on Saturday, May 9, there will be an education and supportive program for caregivers.
Each year, approximately 500 people with brain tumors are treated at the Medical Center and Wilmot Cancer Center, making it the largest program in the region. The events are offered by the Program for Brain and Spinal Tumors at the Medical Center and the Wilmot Cancer Center.
Rochester Scientist Wins Major Award for Alzheimer's Research
Wednesday, April 15, 2009
A Rochester researcher whose work has opened up a whole new avenue in Alzheimer's disease research has received a major prize from the American Academy of Neurology.
Berislav Zlokovic, M.D., Ph.D., director of the Center for Neurodegenerative and Vascular Brain Disorders at the University of Rochester Medical Center, will receive the 2009 Potamkin Prize for Research in Pick's, Alzheimer's, and Related Diseases during the AAN annual meeting later this month in Seattle.
Astrocytes Help Separate Man from Mouse
Monday, March 23, 2009
A type of brain cell that was long overlooked by researchers embodies one of very few ways in which the human brain differs fundamentally from that of a mouse or rat, according to researchers who published their findings as the cover story in the March 11 issue of the Journal of Neuroscience.
Scientists at the University of Rochester Medical Center found that human astrocytes, cells that were long thought simply to support flashier brain cells known as neurons that send electrical signals, are bigger, faster, and much more complex than those in mice and rats.
"There aren’t many differences known between the rodent brain and the human brain, but we are finding striking differences in the astrocytes. Our astrocytes signal faster, and they’re bigger and more complex. This has big implications for how our brains process information," said first author Nancy Ann Oberheim, Ph.D., a medical student who recently completed her doctoral thesis on astrocytes.
URMC Leads Study for New Treatment for Tourette’s
Tuesday, December 2, 2008
The University of Rochester Medical Center is leading a multi-center clinical research study of a new experimental treatment for Tourette’s syndrome. The study will examine whether or not a drug that alters the chemical activity in the brain can alleviate the symptoms of the disease.
Tourette’s syndrome (TS) is a neurological disorder characterized by multiple, repeated tics. These tics generally consist of abrupt and involuntary vocal outbursts or muscular jerks. Symptoms usually begin at an early age and can increase in frequency and severity over time. Many individuals with TS have a mild form of the disease and do not require medical intervention unless the tics interfere with normal daily function. Patients with more severe forms of TS are currently treated with various antipsychotic drugs.
While the precise mechanism that causes Tourette’s is unknown, we have long observed that the neuro-chemical dopamine is overly active in individuals with the disease,
said URMC neurologist Roger Kurlan, M.D., the study’s principal investigator. This chemical imbalance in the brain may play a role in the disease and, consequently, the drugs that are currently used to treat the disease are known to suppress dopamine production. However, these drugs are also associated with severe side effects that often deter their use.
Researchers Identify Toehold for HIV’s Assault on Brain
Friday, November 14, 2008
Scientists have unraveled in unprecedented detail the cascade of events that go wrong in brain cells affected by HIV, a virus whose assault on the nervous system continues unabated despite antiviral medications that can keep the virus at bay for years in the rest of the body.
The new research reveals key steps taken in the brain by Tat, a protein that is central to HIV’s attack on cells called neurons. Researchers discovered the receptor that Tat uses to attack neurons, and they were able to reverse the effects of Tat in the laboratory by blocking the receptor.
The discovery of a major molecular player in the process opens up a new avenue for researchers to explore in their efforts to prevent or treat HIV’s neurological effects, for which there is no currently approved treatment. Researchers say that much of the molecular action that underlies HIV’s attack on the brain also occurs in other diseases, such as Parkinson’s and Alzheimer’s diseases, and that the results spell progress for those conditions as well.
The team from the University of Rochester Medical Center and other institutions published its results online Nov. 13 in the journal PloS One.
Alzheimer's Gene Slows Brain's Ability to Export Toxic Protein
Thursday, November 13, 2008

A ring of amyloid in the wall of an arteriole
in the brain of a patient who had Alzheimer's disease
(Courtesy of James M. Powers, M.D.)
The only known genetic risk factor for Alzheimer's disease slows down the brain's ability to export a toxic protein known as amyloid-beta that is central to the damage the disease causes, scientists have found.
The research, published Nov. 13 by the Journal of Clinical Investigation, provides new clues into the workings of a protein known as apolipoprotein E4, or ApoE4. People who carry two copies of the gene have roughly eight to 10 times the risk of getting Alzheimer's disease than people who do not.
The new results are in line with a body of research amassed over the last 15 years by the leader of the team, Berislav Zlokovic, M.D., Ph.D., of the University of Rochester Medical Center, that blood circulation plays a key role in the disease. His team has identified much of the molecular machinery that allows amyloid-beta to sidestep the body's safeguards and enter the brain, and he has discovered molecules that falter when the toxic protein accumulates in the brain.
Our latest findings help explain one of the major risk factors for Alzheimer's disease,
said Zlokovic. ApoE4 changes the brain's ability to rid itself of amyloid-beta. It's becoming more and more apparent that the brain's ability to clear out amyloid-beta, through the vascular system and across the blood-brain barrier, is central to the development of Alzheimer's disease.
Brain Tumor Care, Treatment in Spotlight
Thursday, April 24, 2008
Patients, physicians, and those caring for loved ones with brain tumors will have an opportunity to attend two full days of programs hosted by health care professionals from the University of Rochester Medical Center. The efforts, co-sponsored by the James P. Wilmot Cancer Center, are offered through the recently enhanced brain tumor treatment program at the University, where approximately 500 brain tumor patients are treated each year.
A seminar Saturday, April 26, will focus on people caring for patients with brain tumors. One week later, on Friday, May 2, another full-day session is geared toward patients, their families, and physicians, covering the latest research and treatment approaches in brain and spinal tumors.
Promising Parkinson's Finding Spurs New Clinical Study
Tuesday, April 15, 2008
The progression of Parkinson’s disease is slower in patients who have high blood levels of urate, a close chemical cousin of the molecule that causes gout, researchers have found. The finding could lead to a way to predict how a given patient with the disease will fare, and it opens the door to a new approach for treating or preventing the disease.
The findings were made public - posted online by the Archives of Neurology on April 14 - the same day that the Michael J. Fox Foundation announced a new study aimed at slowing the disease by continuing the research in people. The foundation is funding a $5.6 million study, the largest award in the foundation’s history, to investigate the potential of boosting urate levels to slow or stop the disease.
The project is being led by physicians at Harvard and Massachusetts General Hospital together with neurologists at the University of Rochester Medical Center.
Sleep Chemical Central to Effectiveness of Deep Brain Stimulation
Monday, December 24, 2007
A brain chemical that makes us sleepy also appears to play a central role in the success of deep brain stimulation to ease symptoms in patients with Parkinson's disease and other brain disorders. The surprising finding is outlined in a paper published online Dec. 23 in Nature Medicine.
The work shows that adenosine, a brain chemical most widely known as the cause of drowsiness, is central to the effect of deep brain stimulation, or DBS. The technique is used to treat people affected by Parkinson's disease and who have severe tremor, and it's also being tested in people who have severe depression or obsessive-compulsive disorder.
Patients typically are equipped with a "brain pacemaker," a small implanted device that delivers carefully choreographed electrical signals to a very precise point in the patient's brain. The procedure disrupts abnormal nerve signals and alleviates symptoms, but doctors have long debated exactly how the procedure works.
"Certainly the electrical effect of the stimulation on neurons is central to the effect of deep brain stimulation," said Maiken Nedergaard, M.D., Ph.D., the neuroscientist and professor in the Department of Neurosurgery who led the research team. "But we also found a very important role for adenosine, which is surprising."
Copper Damages Protein that Defends Against Alzheimer’s
Wednesday, November 7, 2007
The research by neuroscientists at the URMC was presented at the annual meeting of the Society for Neuroscience in San Diego Nov. 3-7. The work was highlighted as part of a press conference on potential environmental influences on Alzheimer's disease.
The team found that copper damages a molecule known as LRP (low-density lipoprotein receptor-related protein), a molecule that acts like an escort service in the brain, shuttling amyloid-beta out of the brain and into the body. The molecule's role in Alzheimer's was revealed more than a decade ago by another author of the work, Berislav Zlokovic, M.D., Ph.D., professor of Neurosurgery and Neurology and director of the Frank P. Smith Laboratory for Neuroscience and Neurosurgery Research. Zlokovic is widely recognized for demonstrating that blood vessels, blood flow, and the blood-brain barrier are central to the development of Alzheimer's disease.
Study of New Epilepsy Treatment Underway at URMC
Friday, September 14, 2007
The University of Rochester Medical Center is participating in a multi-center study of a new medical device to treat epilepsy. The Rochester study is being overseen by neurologists Michel Berg, M.D. and James Fessler, M.D., and neurosurgeons Web Pilcher, M.D., Ph.D. and Jason Schwalb, M.D.
Uncontrolled seizures related to epilepsy are generally treated with medications,
said Berg, medical director of the Strong Epilepsy Center. However, many individuals treated with medication alone continue to experience seizures or have unacceptable medication side effects. If these patients are not candidates for epilepsy surgery, then options to effectively control their seizures are limited.
The Responsive Neurostimulator System (RNS) is an implantable device that is designed to suppress seizures in patients with epilepsy before any symptoms appear, much like implantable cardiac pacemakers are intended to detect abnormal heart rhythms and then deliver electrical stimulation to correct them. Neuropace, the California-based developer and manufacturer of the RNS system, is funding the trial. URMC is one of 28 centers across the country testing the new technology.
Alzheimer’s Project Focuses on Role of Brain Inflammation
Thursday, August 30, 2007
Scientists at the University of Rochester Medical Center have received $1.37 million to continue their work looking at some of the earliest events that occur at the start of Alzheimer's disease - a condition that now generally goes undetected until the death of key brain cells has been underway for decades.
The team led by William Bowers, Ph.D., associate professor of Neurology and a scientist in the Center for Neural Development and Disease, is focusing on the role of inflammation in the evolution of the disease. Just as rheumatoid arthritis can ravage the body's joints because of the inflammation it causes, scientists are realizing that the same thing happens to the brain in patients with Alzheimer's disease. The brain can be under assault for decades as the body attempts to fend off some perceived threat.
Draining Away Brain's Toxic Protein to Stop Alzheimer's
Monday, August 13, 2007
Scientists are trying a plumber's approach to rid the brain of the amyloid buildup that plagues Alzheimer’s patients: Simply drain the toxic protein away.
That’s the method outlined in a paper published online August 12th by Nature Medicine. A team of scientists from the University of Rochester Medical Center, led by neuroscientist Berislav Zlokovic, M.D., Ph.D., show how the body's natural way of ridding the body of the substance is flawed in people with the disease. Then the team demonstrated an experimental method in mice to fix the process, dramatically reducing the levels of the toxic protein in the brain and halting symptoms. The team is now working on developing a version of the protein that could be tested in people with the disease.
Brain Inflammation May Be Friend, Not Foe, For Alzheimer’s Patients
Monday, June 4, 2007
In the June 1st issue of the Journal of Clinical Investigation, a team of scientists from the University of Rochester Medical Center shows that a key inflammatory regulator, a known villain when it comes to parsing out damage after a stroke and other brain injuries, seems to do the opposite in Alzheimer's disease, protecting the brain and helping get rid of clumps of material known as plaques that are a hallmark of the disease.
Speedsters’ Traffic Fines Fund New Research on Spinal Cord Injury
Friday, August 25, 2006
More than a dozen Rochester scientists seeking ways to reverse or lessen the effects of paralysis and other effects of spinal cord injury will begin new projects and continue promising research, thanks to motorists in New York State who push the gas medal a little too far.
Three research projects at the University of Rochester Medical Center are among the programs funded this year through the Spinal Cord Injury Research Program run by the New York State Department of Health. The program, created in 1998, uses fines paid by speeding motorists to fund research into spinal cord injury, whose number-one cause nationwide is motor vehicle accidents. In Rochester this year the grants are going to Roman Giger, Ph.D.; Maiken Nedergaard, M.D., Ph.D.; and Mark Noble, Ph.D.
Novel Stem Cell Technology Leads to Better Spinal Cord Repair
Thursday, April 27, 2006
Researchers believe they have identified a new way, using an advance in stem-cell technology, to promote recovery after spinal cord injury of rats, according to a study published in today’s Journal of Biology. Scientists from the New York State Center of Research Excellence in Spinal Cord Injury showed that rats receiving a transplant of a certain type of immature support cell from the central nervous system (generated from stem cells) had more than 60 percent of their sensory nerve fibers regenerate. Just as importantly, the study showed that more than two-thirds of the nerve fibers grew all the way through the injury sites eight days later, a result that is much more promising than previous research. The rats that received the cell transplants also walked normally in two weeks.
These studies provide a way to make cells do what we want them to do, instead of simply putting stem cells into the damaged area and hoping the injury will cause the stem cells to turn into the most useful cell types,
explains Mark Noble, Ph.D., co-author of the paper, professor of Genetics at the University of Rochester, and a pioneer in the field of stem cell research. It really changes the way we think about this problem.
The breakthrough is based on many years of stem cell biology research led by Margot Mayer-Proschel, Ph.D., associate professor of Genetics at the University of Rochester. In the laboratory, Mayer-Proschel and colleagues took embryonic glial stem cells and induced them to change into a specific type of support cell called an astrocyte, which is known to be highly supportive of nerve fiber growth. These astrocytes, called glial precursor-derived astrocytes or GDAs, were then transplanted into the injured spinal cords of adult rats. Healing and recovery of the GDA rats was compared to other injured rats that received either no treatment at all or treatment with undifferentiated stem cells.
Blood Flow in Brain Takes a Twist, Affecting Views of Alzheimer’s
Friday, January 6, 2006
New findings that long-overlooked brain cells play an important role in regulating blood flow in the brain call into question one of the basic assumptions underlying today's most sophisticated brain imaging techniques and could open a new frontier when it comes to understanding Alzheimer's disease.
In a paper to appear in the February issue of Nature Neuroscience and now available on-line, scientists at the University of Rochester Medical Center demonstrate that star-shaped brain cells known as astrocytes play a direct role in controlling blood flow in the brain, a crucial process that allows parts of the brain to burst into activity when needed. The finding is intriguing for a disease like Alzheimer's, which has long been considered a disease of brain cells known as neurons, and certainly not astrocytes.
"For many years, astrocytes have been considered mainly as housekeeping cells that help nourish and maintain a healthy environment for neurons. But it's turning out that astrocytes may play a central role in many human diseases," said neuroscientist Maiken Nedergaard, M.D., Ph.D., who has produced a string of publications fingering astrocytes in diseases like epilepsy and spinal cord injury.
New Findings About Brain's 'Compass' Offer Clues About Alzheimer's
Thursday, March 28, 2002
A tiny section of the brain that is ravaged by Alzheimer's disease is more important for our ability to orient ourselves than scientists have long thought, helping to explain why people with the disease become lost so easily. The findings by neuroscientists at the University of Rochester Medical Center are reported in the March 29 issue of Science.
Neurologist Charles Duffy, M.D., Ph.D., previously discovered that a small section of brain tissue slightly above and behind the ear - known as the medial superior temporal area (MST) - acts much like a compass, instantly updating your mental image of your body's movements through space. In new research, Duffy and graduate student Michael Froehler show that the MST acts not only as a compass but also as a sort of biological global positioning system, providing a mental map to help us understand exactly where we are in the world and how we got there.
Road Skills Hint At "Motion Blindness" Of Alzheimer's
Thursday, January 31, 2002
Doctors have added to the evidence that patients with Alzheimer's disease lose their way not simply because their memory is failing but because they are subject to a unique form of brain damage that causes symptoms doctors call "motion blindness." Some of the new data comes from driving tests of a small number of patients, where researchers have linked the condition to the loss of one specific driving skill: the ability to stay in one's lane while driving.
While it's obvious that people with Alzheimer's disease are losing their memory, that's only part of the reason why they become lost,
says neurologist Charles Duffy, M.D., Ph.D., who leads the research team at the University of Rochester Medical Center. These patients also lose their ability to perceive their own motion. That's ultimately what puts them at much greater risk than others of becoming lost.