Research
Clinical Research
Laboratory Research
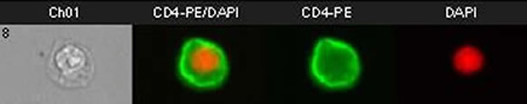
Human T cell stained with anti CD4 antibodies and DAPI nuclear stain. Imaged using the
URMC Flow Cytometry Core Amnis Imagestream Instrument.
The URMC Infectious Disease Division has active laboratory programs in HIV, influenza, RSV and HPV with a focus on vaccine development and testing and translational research. There are research opportunities for undergraduate, graduate and medical students, and postdoctoral fellows. These research efforts have developed in the context of an extraordinarily productive collaborative relationship with investigators in the Center for Vaccine Biology and Immunology (CVBI), the Department of Microbiology an Immunology, the Department of Biochemistry and Biophysics the Department of Biostatistics and Computational Biology and with colleagues in the Division of Allergy, Immunology, and Rheumatology.
The ID Division is also home to the Clinical Trials Processing Lab, directed by Christopher Lane. This lab is a fee-for-service lab that processes blood and tissue samples collected from human clinical trials. If you are conducting a clinical trial that requires laboratory processing or support, please contact Christopher Lane at 276-5574.
The following faculty have laboratories where research opportunities are available:
 John J. Treanor, MD
John J. Treanor, MD
 William Bonnez, MD
William Bonnez, MD
 Edward Walsh, MD
Edward Walsh, MD
Walsh-Falsey Lab
 Ann Falsey, MD
Ann Falsey, MD
Walsh-Falsey Lab
 Angela Ramona Branche, MD
Angela Ramona Branche, MD
 Cynthia L Monaco, MD, PhD
Cynthia L Monaco, MD, PhD