Training Program Serves as Pipeline for Medical Technologists
In an effort to combat a statewide shortage of licensed laboratory technologists, the School of Medicine and Dentistry began offering the clinical/medical technology advanced certificate – or “med tech” program two years ago as a way to “grow our own” medical technologists.
URMC Has Strong Showing at USCAP 2019 Meeting
The Department of Pathology and Laboratory Medicine at URMC was well represented at the 2019 meeting of the U.S. and Canadian Academy of Pathology (USCAP) in National Harbor, MD.
Alumni Q&A: Jaclyn Cappel
Cappel is currently based out of Williamsport Regional Medical Center, Williamsport, PA.
Alumni Q&A: Tara Mahar, M.D.
Dr. Tara Mahar is the chief medical examiner for the Erie County Department of Health, in Buffalo. She attended medical school at the University and graduated from Pathology residency in 2011. In addition to her role as the M.E. she is a clinical assistant professor of Pathology and Anatomical Sciences at the University of Buffalo’s Jacobs School of Medicine.
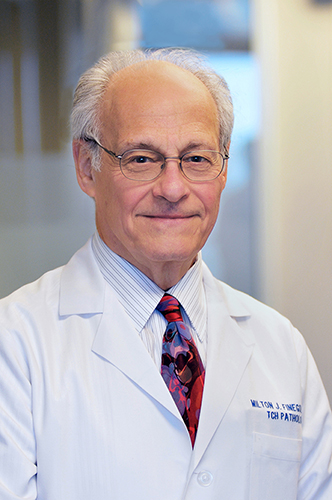
Alumni Gift to Fund New Pediatric Pathology Fellowship at URMC
A $1 million gift from Milton Finegold, M.D., an alumnus of the University of Rochester School of Medicine and Dentistry, will support a new pediatric pathology fellowship.