News
20242023202220212020
Maiken Nedergaard receives Nakasone Award
Wednesday, May 1, 2024

Maiken Nedergaard, a professor of neurology, has been recognized by the International Human Frontier Science Program Organization with its 2024 Nakasone Award for her “groundbreaking discovery and exploration” of the glymphatic system, the brain’s unique waste removal system, and the role that sleep plays in its function.
Nedergaard is codirector of the Center for Translational Neuromedicine, which maintains research facilities at the University of Rochester Medical Center and the University of Copenhagen. In 2012, her lab first described the glymphatic system, a previously unknown network of channels that piggybacks on blood vessels. The system is used to transport cerebrospinal fluid deep into brain tissue and flush away toxic waste, including beta amyloid and tau, two proteins associated with Alzheimer’s disease.
New Art Space in Neurology Embraces Diversity and Equity
Monday, April 22, 2024

The Department of Neurology has opened the doors on a new art gallery that will feature diverse artistic voices. Under the stewardship of noted Rochester artist Shawn Dunwoody, the Unity Gallery will leverage art to provoke thought, encourage dialogue, and celebrate the voices, minds, and faces that shape the community and medicine.
“The population of the United States is not adequately represented in the field of medicine,” said Blanca Valdovinos, MD, associate chair of Diversity, Equity, Inclusion, and Justice for the Department who helped lead efforts to create the new gallery. “The Unity Gallery is designed to be a focal point where faculty, staff, residents, and visitors encounter a visual narrative that embodies the inclusivity and diversity integral to the Department's identity and represents the commitment to creating an environment where everyone feels a sense of belonging.”
The Unity Gallery is in Department of Neurology’s Joynt Corridor located in 5.4300 in Strong Memorial Hospital and is open to visitors from 11:00 AM to 4:00 PM on weekdays. The works can also be viewed virtually on the Unity Gallery website.
“Art opens ourselves up to more perspectives, to more cultures, broader ways of thinking about things, and it can build critical thinking skills,” said Bob Holloway, MD, MPH, chair of the Department of Neurology. “Art can build empathy with people, and those are very humanistic traits that not only make us better people, but it can also make us better physicians. Our primary job is to make people feel seen, feel heard, understand their perspectives, walk in their shoes, and then we can partner with them better.”
Read More: New Art Space in Neurology Embraces Diversity and EquityDavid Gill to Lead Cognitive and Behavioral Neurology
Monday, April 1, 2024

David Gill, MD, has been appointed chief of the Division of Cognitive and Behavioral Neurology at the University of Rochester Medical Center (URMC). A highly respected local clinician and academic, Gill returns to the institution where he completed his residency and fellowship training and assumes his new position effective April 1, 2024.
‘Working in collaboration with our colleagues in Psychiatry, Dave has an exciting vision for the future of dementia care in our community,” said Robert Holloway, MD, MPA, chair of URMC Department of Neurology. “He will help grow the Memory Care Program, improve access to cutting-edge treatments for patients and families in a socially responsible manner, and expand training opportunities to increase the numbers of providers that care for patients with cognitive disorders, specifically in the Rochester area.”
Gill will work with the teams in the Alzheimer’s Disease Care, Research and Education (AD-CARE) Program, the Del Monte Neurosciences Institute, and the University of Rochester Aging Institute to support and help grow basic science and clinical research programs in the field of cognitive disorders. Gill will also build upon his existing relationships in the community to advance education for patients and caregivers through partnerships with Lifespan, the Alzheimer’s Association, and other community groups.
Read More: David Gill to Lead Cognitive and Behavioral NeurologyJamie Capal Tapped as New Head of Child Neurology
Friday, February 9, 2024
 Jamie Capal, MD, has been selected the next chief of the Division of Child Neurology at the University of Rochester Medical Center (URMC) and Golisano Children’s Hospital. Capal—who specializes in intellectual and developmental disabilities—joins a program that has, though more than 50 years of clinical innovation and research, transformed care for children with neurological disorders.
Jamie Capal, MD, has been selected the next chief of the Division of Child Neurology at the University of Rochester Medical Center (URMC) and Golisano Children’s Hospital. Capal—who specializes in intellectual and developmental disabilities—joins a program that has, though more than 50 years of clinical innovation and research, transformed care for children with neurological disorders.
“Jamie has an exciting vision to lead our pre-eminent program in Child Neurology to even greater heights,” said Bob Holloway, MD, MPH, chair of the Department of Neurology. “She will use her prior experiences to mentor faculty, providers, trainees, and staff to build and support successful teams around the many priority programs within the division and across the Medical Center. She will also play an instrumental role in intellectual and developmental disabilities research and the growth of our rare disease and gene therapy clinical trials operations.”
Capal will hold the Frederick A. Horner, MD, Endowed Distinguished Professorship in Pediatric Neurology and will also have an appointment in the Department of Pediatrics. She will also serve as co-director of the Human Clinical Phenotyping and Recruitment Core of the University of Rochester Intellectual Developmental Disability Research Center (UR-IDDRC). She will start her new position on July 1, 2024
“Intellectual and development disabilities are one of the cornerstones of the University’s neuroscience research enterprise, and we are only one of a handful of institutions that hold the three major federally-funded centers of excellence in research, training, care, and community partnership in this field,” said John Foxe, PhD, director of the University of Rochester Del Monte Institute for Neuroscience and co-director of the UR-IDDRC. “These are some of the most complex and challenging diseases in all of medicine, and Dr. Capal’s clinical research experience will enable us to continue to build bridges between the research and clinical programs, and ultimately improve care.”
Read More: Jamie Capal Tapped as New Head of Child NeurologyCalcium Channel Blockers Key to Reversing Myotonic Dystrophy Muscle Weakness, Study Finds
Tuesday, January 2, 2024
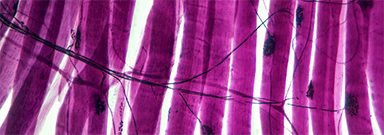 New research has identified the specific biological mechanism behind the muscle dysfunction found in myotonic dystrophy type 1 (DM1) and further shows that calcium channel blockers can reverse these symptoms in animal models of the disease. The researchers believe this class of drugs, widely used to treat a number of cardiovascular diseases, hold promise as a future treatment for DM1.
New research has identified the specific biological mechanism behind the muscle dysfunction found in myotonic dystrophy type 1 (DM1) and further shows that calcium channel blockers can reverse these symptoms in animal models of the disease. The researchers believe this class of drugs, widely used to treat a number of cardiovascular diseases, hold promise as a future treatment for DM1.
“The main finding of our study is that combined calcium and chloride channelopathy is highly deleterious and plays a central role in the function impairment of muscle found in the disease,” said John Lueck, PhD, an assistant professor at the University of Rochester Medical Center (URMC) in the Departments of Pharmacology and Physiology, and Neurology. “Our research also suggests that muscle impairment in DM1 is potentially mitigated by common clinically available calcium channel blockers and that calcium channel modulation is a potential therapeutic strategy.” Lueck is lead author of the study, which appears in the Journal of Clinical Investigation.
Toxic RNA disrupts muscle function
Myotonic dystrophy is one of the most common forms of muscular dystrophy. People with the disease have muscle weakness and prolonged muscle tensing (myotonia), making it difficult to relax muscles after use. The disease also affects the eyes, heart, and brain, leading eventually to difficulty walking, swallowing, and breathing.
More than 20 years ago, URMC neurologist Charles Thornton, MD, and others uncovered how a genetic flaw–a trinucleotide repeat expansion that results in thousands of repetitions of code on a segment of chromosome 19–gives rise to DM1. This repeat expansion, which grows longer over time, results in the creation of abnormal RNA which accumulates in the nucleus of cells and interferes with the normal processing of many other RNAs. Thornton is a co-author of the current study and the research was a collaboration between the Lueck and Thornton labs.
Read More: Calcium Channel Blockers Key to Reversing Myotonic Dystrophy Muscle Weakness, Study FindsResident Interviews
Monday, January 1, 2024
The Department of Neurology would like to welcome residency applicants, interviewing on Monday, January 8th
Child Neurology Applicants
Naomi Cohen – The University of Texas Southwestern Medical School
Micailya Hall – Eastern Virginia Medical School
Melissa Huberman – University of Miami
Lucy Laura Olivieri – University of New England
Adryanna Tucker – Edward Via College of Osteopathic Medicine
Resident Interviews 12-18-23
Tuesday, December 12, 2023
The Department of Neurology would like to welcome residency applicants, interviewing on Monday, December 18th
Adult Neurology Applicants
Adedayo Adegbile – Khalifa University College of Medicine & Health Sciences
Brittany Calkins – University of Missouri-Columbia School of Medicine
Kurtis Chien-Young – Boston University School of Medicine
Zoya Gurm – Wayne State University School of Medicine
Mohamad Hamze – University of Vermont
Caitlyn Kelly – Louisiana State University School of Medicine in New Orleans
Justin Kosman – Geisinger Commonwealth School of Medicine
Rachel Simon – Geisinger Commonwealth School of Medicine
From lab to life-changer: URMC neuromuscular researchers pave the way for gene therapy revolution
Monday, October 30, 2023
 Myotonic dystrophy type 2 (DM2), a rare form of muscular dystrophy, can trace its origins to a meeting three decades ago in the Garvey Room on the fifth floor of Strong Memorial Hospital. Present at the regular gathering of neuromuscular researchers were Robert (Berch) Griggs, MD, and Richard Moxley, MD, two of the founding fathers of the University of Rochester Medical Center (URMC) Department of Neurology, and Charles Thornton, MD.
Myotonic dystrophy type 2 (DM2), a rare form of muscular dystrophy, can trace its origins to a meeting three decades ago in the Garvey Room on the fifth floor of Strong Memorial Hospital. Present at the regular gathering of neuromuscular researchers were Robert (Berch) Griggs, MD, and Richard Moxley, MD, two of the founding fathers of the University of Rochester Medical Center (URMC) Department of Neurology, and Charles Thornton, MD.
As was a common practice, a patient with a puzzling case joined the group that day. This individual demonstrated the well-established clinical symptoms of myotonic dystrophy but did not possess the genetic flaw associated with the disease. The question put to those in the room was whether this case–one of a growing number identified via a new genetic test—was a completely new disease, a flaw with the test, or something else. “There was a vigorous debate and a wager that involved a six-pack of beer,” said Griggs. “But no one can recall who was on the winning side of the argument and whether beer ever changed hands.”
In 1994, Griggs, Moxley, and Thornton published descriptions of three of these cases in the Annals of Neurology, thereby becoming the first to describe DM2. It was proposed at the time that the new disease be named for the trio, but they declined in recognition of other scientific teams around the globe that were arriving at the same conclusions, and the disease eventually came to be known as DM2.
Read More: From lab to life-changer: URMC neuromuscular researchers pave the way for gene therapy revolutionFDA approves Duchenne Muscular Dystrophy treatment following clinical trial at URMC
Thursday, June 22, 2023

On Thursday, the FDA approved the first gene therapy for Duchenne Muscular Dystrophy (DMD) and it did it based in part on research that was conducted right here in Rochester.
A number of young boys with DMD participated in phase three of the clinical trial at URMC for a therapy called Elevidys.
Elevidys was grated accelerated approval for pediatric patients aged four and five with DMD. One of the families who participated in the trial says since their son’s infusion in January they’ve seen remarkable progress.
Charlie Prior was diagnosed with DMD at age three. DMD almost exclusively impacts boys and in the past, most have lost the ability to walk by the time they become teenagers.
That’s why Charlie’s parents were eager to join the Elevidys trial. Dr. Emma Ciafaloni has been leading it at URMC.
“This has been in the making for a very long time,” she previously explained to News10NBC. “And so that’s the exciting part of this is really trying to replace the broken gene and make the proteins that are missing — unlike other treatments that we have that are more like may be symptomatic treatments.”
Charlie had an infusion in January that his mom believes was the treatment.
“About eight weeks later, he was able to fully dress himself independently, put on his own shoes, I saw him hop on a swing and just start swinging, jumping and even now he’s able to jump in a pool — which is awesome. Oh, and he is snapping his fingers,” Cheryl Prior tells News10NBC.
Read More: FDA approves Duchenne Muscular Dystrophy treatment following clinical trial at URMCPalliative Care: Creating a New Model to Address Suffering for Neurological Illnesses
Wednesday, June 21, 2023

Neurologic illnesses, including Alzheimer’s, brain cancer, amyotrophic lateral sclerosis (ALS) and stroke, are among the most dreaded illnesses in medicine and leading causes of disability and death worldwide. Despite the huge burden of suffering these patients and families face, palliative care is not routinely offered and is used far less than in other illnesses.
In a review commissioned by the journal Lancet Neurology, an international team of experts argue that current models of care do not adequately address the needs of people living with neurologic illness. They propose a new evidence-based framework for early and ongoing palliative care approaches employed by multiple members of the health care team to improve quality of life for individuals with neurological disorders and their families.
“Suffering is the fundamental concern of palliative care. To improve care we must address the total pain of neurologic illness -- not just physical pain, but also psychological, social, and spiritual distress,” said University of Rochester Medical Center neurologist Benzi Kluger, MD, lead author of the article produced by members of the International Neuropalliative Care Society. “This model of care seeks to screen for and prevent suffering by integrating an early approach to palliative care, with neurologists, and other clinicians who care for people with neurological illnesses incorporating a palliative care approach from day one.”
Nearly all neurological diseases cause a wide range of symptoms, including pain, fatigue, and memory loss. Depression, anxiety, social isolation, and loss of independence are also common. Family members typically are the primary at-home caregivers and over time can struggle with the emotional impact of seeing a loved one suffer as well as with the social, financial and physical impact of providing care.
Read More: Palliative Care: Creating a New Model to Address Suffering for Neurological Illnesses Leading by Example: How the University of Rochester’s Neuropalliative Care Service Expands Treatment Possibilities
Friday, June 2, 2023
 With few neuropalliative care services available in the US, the University of Rochester stands as a prime example of how a successful program can transform patient care. Palliative care is a specialty of medicine that aims to improve quality of life for individuals with serious or advanced medical conditions by assessing and managing symptoms, establishing goals of care, providing support to caregivers, and engaging in advance care planning discussions.1 Since the turn of the century, neuropalliative care has become an emerging subspecialty that serves as a unique piece of the wider care paradigm, to the point that formal organizations, fellowship programs, and care centers have been established, and a greater number of clinicians have begun to implement aspects of this model in their own care regimens.
With few neuropalliative care services available in the US, the University of Rochester stands as a prime example of how a successful program can transform patient care. Palliative care is a specialty of medicine that aims to improve quality of life for individuals with serious or advanced medical conditions by assessing and managing symptoms, establishing goals of care, providing support to caregivers, and engaging in advance care planning discussions.1 Since the turn of the century, neuropalliative care has become an emerging subspecialty that serves as a unique piece of the wider care paradigm, to the point that formal organizations, fellowship programs, and care centers have been established, and a greater number of clinicians have begun to implement aspects of this model in their own care regimens.
Headed by Benzi Kluger, MD, MS, the Neurology Supportive and Palliative Care Service at the University of Rochester stands as one of those few established neuropalliative care programs in the United States. Kluger, who also serves as a professor in the Department of Neurology and Department of Medicine, was recruited to the facility in 2020 from the University of Colorado to build upon previous work in developing models of neuropalliative care for Parkinson disease (PD) and other neurodegenerative illnesses.
"The key is to have at least 1 person who’s a strong champion for the cause," Kluger told NeurologyLive®. "If there’s that person and they’re willing to be creative and persistent, then I think success is inevitable. In my work at Colorado and Rochester, as well as lessons I learned from Janis Miyasaki, MD, MED, FRCPC, FAAN—who started one of the first clinics in Canada—having a team with complimentary skill sets is important."
Miyasaki, an esteemed leader in neurology, initiated the first neurologist-led palliative care clinic at the University of Toronto in 2007.2 Since then, she has spread her wisdom to several other neurologists and movement disorder specialists interested in starting their own clinics, and has established herself as one of the leading voices in the realm of neuropalliative care.
At the University of Rochester, one of the core aspects of the neuropalliative care service is treating the total pain of illness—meaning not just the physical and mental symptoms, but also the psychological, social, and spiritual aspects of what a patient and their family are going through. The faculty is comprised of several different subspecialties, including those who work as administrators, community and patient advocates, and registered nurses. In addition, there are numerous physicians and advanced practice providers on-staff who have backgrounds in palliative care as well as in neuromuscular disorders, movement disorders, stroke, memory care, general neurology, child neurology, and neuro-oncology.3
There are several social work and spiritual/family support staff members in the program, including chaplains and mental health therapists, such as Sue Ouellette, PhD. Ouellette, who’s been with the program for several years a chaplain, is also a licensed marriage and family therapist, with a special interest in working with individuals with disabilities and their families. She is fluent in American Sign Language (ASL) and conducts sessions in ASL when appropriate.
Read More: Leading by Example: How the University of Rochester’s Neuropalliative Care Service Expands Treatment PossibilitiesTelemedicine Extends Reach of Stroke and Neurological Care
Wednesday, April 19, 2023
UR Medicine neurologists are now providing remote acute and inpatient neurological care for 16 hospitals across upstate New York, creating one of the more comprehensive hub-and-spoke networks in the nation.
“We are able to provide acute neurologic consultations for any patient who presents to any UR Medicine hospital, as well as some of our important partner institutions,” said Adam Kelly, MD, director of Teleneurology and Regional Development for the Department of Neurology. “While some neurology programs provide remote consultations for patients in emergency departments, our team continues to follow patients longitudinally while they remain in the hospital. This is a major accomplishment that would not be possible without the hard work and dedication of a team of staff and providers, both at Strong Memorial and our affiliate hospitals, who are committed to the concept of delivering virtual care in our region.”
24/7 Telestroke Care
UR Medicine telestroke program has existed for several years but grew substantially in 2018-2019 from a partnership to provide telestroke care to the Bassett Healthcare Network. Curtis Benesch, MD, the medical director of the UR Medicine Comprehensive Stroke Center, led this initial effort prior to handing off directorship to Kelly in 2019. The program consists of a dedicated team of stroke specialists who are available 24/7 to interact with patients and families and consult with medical providers via phone or video.
Read More: Telemedicine Extends Reach of Stroke and Neurological CareAppointment of Dr. Blanca Valdovinos as Associate Chair of Diversity, Equity, Inclusion, and Justice
Friday, April 7, 2023
Dr. Blanca Valdovinos has been appointed as the Associate Chair of Diversity, Equity, Inclusion, and Justice (DEIJ) in the Department of Neurology. Dr. Valdovinos is an Assistant Professor of Neurology who completed her undergraduate degree at Cornell and then completed her Medical Degree and Neurology Residency at the University of Rochester. She furthered her training in Rochester by completing a Movement Disorders fellowship and joined as faculty in 2020.
Dr. Valdovinos has had an early, impressive impact. She has completed the American Academy of Neurology (AAN) Diversity Leadership Program and is the Co-Director of the Parkinson’s Foundation Center of Excellence. In 2020, she established the Spanish Language Neurology Clinic, which has seen over 250 new Spanish speaking patients during its first two years. She is active in the Hispanic community in Rochester and has worked closely with Ibero, an agency that advocates for Hispanics and the underserved. She has given talks in Spanish on neurologic disorders at Ibero’s Centro De Oro (Spanish language day program) and is a member of its Community Advisory Board whose goal is to educate community members on how research is conducted while developing trust. Recently, Dr. Valdovinos was appointed as a member of the Editorial Board of Brain & Life en Español, the patient and care partner-oriented magazine published by the AAN.
She is a UR Medicine Geriatrics Faculty Scholar and has presented her work for local and national audiences. She is a frequent contributor to PBS and local radio shows and participates on national committees to guide research with a focus on Hispanic patients and caregivers with memory disorders. She was the education program director and speaker for the course Parkinson’s Disease: Assessment and Management at the AAN annual meeting in 2022. Her passion and strong track record of mentoring will enable her to build partnerships and excel in this role.
Dr. Valdovinos will Co-Chair the Department’s Inclusion, Diversity, Equity, Antiracism, and Social Justice (IDEAS) Council with focused attention on 1) Enhancing Climate: transparency, education and awareness initiatives, 2) Learner and Workforce Development, and 3) Advocacy, Outreach and Community Initiatives. Dr. Nimish Mohile has served in this capacity for the past six years, literally defining the role of Diversity Officers within the Department of Neurology, while also leading national DEIJ efforts within our American Academy of Neurology. Nimish, along with Chennel Andersen, have been instrumental in leading our DEIJ efforts, most notably during the early phases of the pandemic where they prioritized and launched our Department’s Equity and Anti-Racism Action plan. Nimish will continue in his role as Associate Chair for Career Development and Leadership, spearheading innovative programs for faculty, trainees, and members of our clinical and academic teams. I am grateful for his past and continuing partnership.
Dr. Valdovinos will advance the Department’s vision and mission and provide leadership across all axes of inequity, across all missions, and across all intersectional measures of diversity. She will advance the evolution and implementation of the Department’s Equity and Anti-racism initiatives, and ensure goal alignment with the five pillars of the URMC’s Equity and Anti-Racism Action Plan: Build, Recruit, Nurture, Exemplify, Engage.
While we have made some progress in advancing equity and inclusion, we still have a long way to go. We have a committed group of DEIJ champions across our department who participate in multiple initiatives within our IDEAS council. Dr. Valdovinos has the ambition, curiosity, and courage to help us chart a continued, focused course of advocacy and change in the years ahead.
Dr. Emma Ciafaloni has been appointed as Associate Chair of Research in Neurology
Friday, April 7, 2023
Dr. Emma Ciafaloni has been appointed as the Associate Chair of Research in the Department of Neurology. Dr. Ciafaloni is the Robert C. and Roslayne H. Griggs Professor in Experimental Therapeutics of Neurological Disease and Professor of Neurology, Pediatrics and Obstetrics & Gynecology.
Dr. Ciafaloni completed her Medical Degree and Neurology Residency training in Milan, Italy, and then undertook a neuromuscular research fellowship at Columbia University and furthered her Neurology Residency training and Neuromuscular/Electromyography Fellowship training at Duke University, before joining the faculty in 2002. She is a nationally and internationally recognized neurologist, a pre-eminent scholar and clinical trialist, a world authority on integrated care delivery for pediatric neuromuscular disorders, and a leading educator of the next generation of clinician-investigators. She has played a leading role on issues relating to gender in neurology and neurologic disorders affecting women.
She is an inspirational team leader and the Director of the Pediatric Neuromuscular Disorders Program, one of the most exciting, academic programs at the University. She has been PI on many multi-site clinical trials for pediatric and adult diseases and understands the challenges related to the feasibility of designing and implementing complex clinical trials. She also has a strong understanding of what is important to patients and their families, and what strategies work best for successful and diverse recruitment. In 2022, she completed a sabbatical at Oxford University to study gene therapy application to muscle diseases, how to advance the case for newborn screening in DMD, and how to best translate new, complex gene-based treatments from research into the clinic setting and maximize equitable access. She is passionate about mentoring and to pass her experiences forward by developing career pathways for junior faculty.
Dr. Ciafaloni will bring this experience and passion to provide leadership and oversight in the administration of the Department of Neurology’s research mission. She will oversee the Department’s research operations, Chair a re-vitalized Neurology Research Committee (and set a vision and strategy for this work), serve as a role model and provide research career guidance to junior faculty, and lead several new and exciting initiatives.
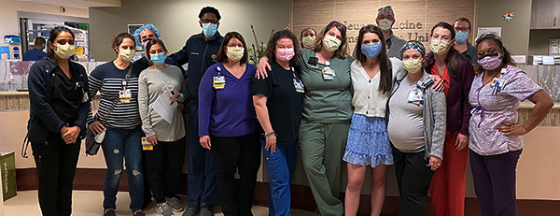
Inpatient Length of Stay Reduction - Gold Award for Team Excellence
Thursday, February 2, 2023
 The URMC inpatient Neurology and Imaging Science departments were recently honored with the Gold Award for Team Excellence by the Greater Rochester Quality Council for a project which saved over 150 admissions from the ED and reduced inpatient length of stay. The GRQC, an affiliate of the Greater Rochester Chamber of Commerce, recognizes teams from a wide range of industries that are committed to quality and performance excellence.
The URMC inpatient Neurology and Imaging Science departments were recently honored with the Gold Award for Team Excellence by the Greater Rochester Quality Council for a project which saved over 150 admissions from the ED and reduced inpatient length of stay. The GRQC, an affiliate of the Greater Rochester Chamber of Commerce, recognizes teams from a wide range of industries that are committed to quality and performance excellence.
This collaboration implemented efforts to reduce a patient’s hospital stay when awaiting an MRI prior to discharge and to prevent unnecessary admissions from the ED beginning in February of 2021 Prior to the launch, data showed that patients who were medically ready for discharge waited an average of two to three additional days in the hospital for an MRI, and many patients were admitted for the sole purpose of an expedited MRI. For improved resource utilization, efforts were made to convert inpatient MRI appointments for patients who could safely be discharged home to urgent outpatient MRI visits.
The project team evaluated inpatient populations that could safely be discharged with their MRI study converted to an outpatient order and developed an alternative workflow whereby the ordering provider could indicate to the MRI team when a patient was considered appropriate for discharge and place a STAT outpatient order for expedited imaging at one of our Ambulatory sites. These efforts have resulted in 532 fewer bed days required for the targeted patient population. This further resulted in our ability to care for 93 incrementally more patients. Tracking shows this project has had a positive financial impact to date of over $465,000. The project is ongoing, and remains extremely successful.
NINDS Delegation Tours Neurology Research and Education Programs in Zambia
Wednesday, January 18, 2023

A team from the National Institutes of Neurological Disorders and Stroke (NINDS) has travelled to Zambia and met with U.S. and Zambian researchers and clinicians who have been building a decades-long partnership to address the neurological burden of diseases like cerebral malaria, HIV, and stroke.
The constellation of research, education, and clinical activities that the NINDS team reviewed during their visit owe their origin to partnerships first formed by University of Rochester Medical Center (URMC) neurologist Gretchen Birbeck, M.D., back in 1994. Birbeck’s research in sub-Saharan Africa, primarily Zambia, aims at identifying risk factors and effective treatments for the neurological problems common in resource-limited tropical settings. She also see patients in Zambia, where she spends five to six months per year, and serves as the director for Chikankata's Epilepsy Care Team in Zambia's rural Southern Province and principal for the Neurology Research Office at the University Teaching Hospital (UTH) in Zambia’s capital, Lusaka.
In partnership with the Zambian Ministry of Health, UTH, the University of Zambia, Johns Hopkins University, Harvard University, Michigan State University, and other institutions, these efforts have grown to include a wide range of complementary neurological research, training, and care programs based in Zambia. The Neurology Research Office established by Birbeck on the main UTH campus serves as hub for many of these efforts, which have received more than $15 million in funding from the National Institutes of Health and other organizations and foundations over the past 29 years.
Read More: NINDS Delegation Tours Neurology Research and Education Programs in ZambiaUR Nursing Professor, Alum Earns American Heart Association Award
Tuesday, November 8, 2022
 A Doctor of Nursing Practice (DNP) alumna who led an initiative to improve the transition of ischemic stroke care from hospital to home is now being recognized nationally for her work.
A Doctor of Nursing Practice (DNP) alumna who led an initiative to improve the transition of ischemic stroke care from hospital to home is now being recognized nationally for her work.
Ann Leonhardt-Caprio, DNP, RN, ANP-BC, FAHA, program coordinator of the Comprehensive Stroke Center at Strong Memorial Hospital and an assistant professor at the School of Nursing, has been named the recipient of the American Heart Association (AHA) Council on Cardiovascular and Stroke Nursing’s 2022 Stroke Article of the Year Award.
Leonhardt-Caprio’s award-winning article, “A Multi-Component Transition of Care Improvement Project to Reduce Hospital Readmissions Following Ischemic Stroke,” was originally published in the April 2022 issue of The Neurohospitalist.
“I’m so honored to have been chosen for the Article of the Year award,” said Leonhardt-Caprio. “The fact that this work is being recognized on a national level is really special.”
Co-authors of the article include School of Nursing faculty members Craig Sellers, PhD, RN, AGPCNP-BC, GNP-BC, FAANP; Elizabeth Palermo, DNP, RN, ANP-BC, ACNP-BC; Thomas Caprio, MD, Chief Medical Officer for UR Medicine Home Care; and Robert Holloway, MD, MPH, Chair of the Department of Neurology at the University of Rochester School of Medicine and Dentistry.
Leonhardt-Caprio accepted the award over the weekend at the AHA’s Scientific Sessions in Chicago, and will also speak at the State of the Science Stroke Nursing Symposium in February.
Read More: UR Nursing Professor, Alum Earns American Heart Association AwardChildren with HIV at Greater Risk for Impaired Neurological Development
Thursday, October 13, 2022
New research in Zambia finds that children infected with HIV are significantly more likely to do worse in neurological assessments despite having well-controlled HIV disease, suggesting that they may struggle with cognitive and mental health issues. However, the research also indicates that early intervention – in the form of better nutrition and antiretroviral therapies – may help close the gap.
“HIV remains a major global health burden and children who are exposed to the virus during childbirth are known to be at greater risk for neurocognitive and psychiatric problems, like depression, as they age,” said David Bearden, M.D., assistant professor of Neurology and Pediatrics at the University of Rochester Medical Center (URMC) and senior author of the study, which appears in the Journal of Acquired Immune Deficiency Syndromes. “This research is an attempt to understand if these problems persist and become more pronounced over time, and whether we can predict who will do well cognitively and who will not.”
The study is the most recent example of a decades-long collaboration involving an international team of researchers. Since 1994, URMC neurologist Gretchen Birbeck, M.D., has partnered with the government of Zambia and clinicians and researchers with the University Teaching Hospital (UTH) in Lusaka, Zambia to study neurological problems associated with infectious diseases like HIV and malaria, which remain major public health problems in sub-Saharan Africa.
Read More: Children with HIV at Greater Risk for Impaired Neurological DevelopmentDr. Schifitto Will Explore COVID’s Potential Link to Dementia
Wednesday, August 31, 2022
There is concern in the scientific community that COVID infection may accelerate cognitive decline in older adults, resulting in a wave of dementia cases in the coming years as the population ages. A new $3.7 million grant from the National Institutes of Aging will allow researchers to more precisely understand how the virus triggers damage in the brain and the long-term impact on cognitive performance.
“Given the high rate of COVID world-wide and aging, the possible added toll to the existing burden of dementia could increase exponentially in the near future,” said University of Rochester Medical Center (URMC) neurologist Giovanni Schifitto M.D., the principal investigator of the new study. “We need to better understand the burden and progression of cognitive decline and the mechanisms by which this occurs. This will help point the way to new interventions designed to forestall the onset of dementia in these individuals.”
The new study will involve a multidisciplinary team of URMC neurologists, infectious disease experts, radiologists, and computer scientists, including Nasir Uddin, Ph.D., Meera Singh, Ph.D., Miriam Weber, Ph.D., Henry Wang, M.D., Ph.D., Hongmei Yang, Ph.D., and Angela Branche, M.D.
Several reports have highlighted the presence of cognitive and psychiatric symptoms associated with COVID infection, particularly in older adults who experienced moderate to severe infection. Other studies suggest that the COVID virus can damage the endothelial cells that line blood vessels through both direct infection and the resulting immune response.
The brain is supplied with blood by a vast network of microscopic vessels. The integrity of this microvasculature declines as we age, compromising the integrity of the blood brain barrier and leaving the brain vulnerable to infection, inflammation, and damage from the immune system. The fear is that the damage caused to blood vessels by COVID infection could speed this process up, increasing risk for cerebral small vessel disease (CSVD), which is associated with cognitive decline and ultimately dementia.
The new study will recruit 300 volunteers 65 and older who had a severe enough COVID infection that it required hospitalization, excluding individuals who required intensive care and had to be placed on a ventilator. Participants will be followed for two years with neurocognitive evaluations, advanced quantitative neuroimaging that will search for changes in white matter, blood flow, and the integrity of blood vessel, and blood biomarkers of inflammation and brain injury.
At-Home Sensors Can Spot Parkinson’s Disease
Tuesday, August 23, 2022
 A new study shows that a device that passively monitors breathing during sleep can not only detect Parkinson’s, but also track the progression of the disease over time. The researchers used an artificial intelligence tool to sift through mountains of data from study participants to find patterns that identify the disease and determine severity.
A new study shows that a device that passively monitors breathing during sleep can not only detect Parkinson’s, but also track the progression of the disease over time. The researchers used an artificial intelligence tool to sift through mountains of data from study participants to find patterns that identify the disease and determine severity.
“I like to compare our understanding of Parkinson’s to a street lamp in the night; we only get a glimpse of the disease when patients visit clinic. Moreover, the methods we use to track the disease over time are subjective,” said Ray Dorsey, M.D., a professor of Neurology at the University of Rochester Medical Center (URMC) and co-author of the study. “As a result, we have a very limited insight into how Parkinson's disease impacts people's daily lives. This study shows that remote monitoring has the potential to identify individuals with Parkinson’s and create an objective measure of severity and progression. This could be a powerful tool to detect the disease early and conduct research more efficiently.”
The research, which appears in the journal Nature Medicine, was led by Dina Katabi, Ph.D., a professor of Electrical Engineering and Computer Science at MIT. Katabi worked closely with researchers at the URMC Center for Health + Technology (CHeT), including Dorsey and Chris Tarolli, M.D., an assistant professor of Neurology. This study is one of several projects supported by CHeT that are exploring new ways to harness remote monitoring, smart phones, smart watches, and other technologies to improve care and advance research in Parkinson’s and other diseases. The study also included researchers from the Mayo Clinic, Massachusetts General Hospital, and Boston University.
Read More: At-Home Sensors Can Spot Parkinson’s DiseaseRare Brain Disorder Does Not Derail Future Career in Medicine
Tuesday, August 16, 2022

In May 2020, Rachael Muggleton was wrapping up her third year of pre-med studies at Penn State University when she unexpectedly and rapidly fell ill, victim to a rare and dangerous inflammation in the brain. She details her remarkable journey in a piece on the Neurocritical Care Society website, in which she describes her decline in health, months-long stay at Strong Memorial Hospital, and remarkable recovery.
Initially admitted to Arnot-Ogden Medical Center in her hometown of Elmira, NY, Rachael was quickly transferred to the Neuromedicine Intensive Care Unit (NMICU) at Strong, where physicians put her in a 42 day medically-induced coma to control her seizures, as a multidisciplinary team of specialists strove to calm her brain and immune system.
Rachael suffered from a rare and complex condition called autoimmune encephalitis (AE), an inflammation in the brain triggered by the body’s own immune system attacking healthy brain cells, which can result in seizures, impaired memory and cognition, and problems with balance, speech, and vision. Tests determined she had a specific type of AE characterized by the creation of antibodies that attack NMDA receptors, which reside at the connections between neurons, disrupting normal signaling between nerve cells and triggering inflammation. This form of AE is more common in women and can be associated with certain cancers, however, the source of the damaging immune response sometimes cannot be identified, as was the case with Rachael.
Read More: Rare Brain Disorder Does Not Derail Future Career in MedicineNew Grant Will Unlock Workings of Glymphatic System
Monday, August 15, 2022
A decade ago, researchers in the lab of Maiken Nedergaard, M.D., D.M.Sc., answered a basic question of biology that up to that point had eluded scientists: how is waste removed from the brain? The discovery of what is now known as the glymphatic system and subsequent research have transformed the way we study a range of neurological disorders and critical brain functions. A new $15 million grant from the National Institutes of Health (NIH) will bring together several teams of researchers to accelerate our understanding of the complex mechanics that control this system, with an eye toward the development of new therapies for diseases like Alzheimer’s.
The new research program will be led by Nedergaard, co-director of the Center for Translational Neuromedicine, and involve scientists and engineers from the University of Rochester, Penn State University, Boston University, and the University of Copenhagen. The research is being funded through The BRAIN Initiative, a massive research program supported by NIH and several other federal research agencies that aims to fill gaps in our current knowledge of the brain’s organization and function.
The glymphatic system – a network of plumbing that runs parallel to blood vessels and pumps cerebral spinal fluid (CSF) through brain tissue to wash away waste – was all but invisible to the scientific world until 2012 when it was first described in a study published in Science Translational Medicine. A paper in the journal Science a year later showed that this system operates primarily while we sleep and removes toxic proteins associated with Alzheimer’s disease. These findings fundamentally changed scientists’ understanding of the biological purpose of sleep and opened the door to potential new ways to treat neurological disorders.
Read More: New Grant Will Unlock Workings of Glymphatic SystemExperimental Gene Therapy Targets Duchenne Muscular Dystrophy
Friday, May 6, 2022
 Children in Rochester were recently among the first in the nation to receive an experimental treatment for Duchenne muscular dystrophy (DMD). The study is part of an accelerating trend of clinical trials involving gene therapies that could transform how we treat a number of devastating childhood neurological disorders.
Children in Rochester were recently among the first in the nation to receive an experimental treatment for Duchenne muscular dystrophy (DMD). The study is part of an accelerating trend of clinical trials involving gene therapies that could transform how we treat a number of devastating childhood neurological disorders.
Emma Ciafaloni, M.D., a neuromuscular neurologist with the University of Rochester Medical Center (URMC) Department of Neurology and Golisano Children’s Hospital, is leading the Rochester study site. URMC was recently one of the first three sites in the nation to start dosing patients in a phase 3 placebo-controlled clinical trial for a gene therapy being developed by Sarepta Therapeutics for children with DMD. The international study will soon add additional sites in North America, Europe, and Asia. Ciafaloni served as the chair of the independent Data Safety and Monitoring Board for the company’s early phase clinical trials of the therapy.
DMD is a condition found almost exclusively in boys and is characterized by muscle weakness, the symptoms of which often appear at a young age and progress rapidly leading to significant disability. Children with DMD typically end up in a wheelchair by age 9 or 10 because of weakness in their legs. The symptoms eventually spread to the heart and muscles responsible for breathing, and the disease is often fatal by the time the individual reaches their 20s or early 30s. An estimated 12,000 people in the U.S. suffer from the disease.
The muscle weakness associated with DMD occurs due to a genetic defect in muscle cells that impairs the production of dystrophin, an important muscle building protein that is largely absent in people with the disease. The new treatment consists of a single infusion that, via an associated adenovirus, delivers into muscle cells a separate and potentially functional “micro” version of the dystrophin gene that takes over production of the protein.
The study is the latest in a number of new gene therapies for pediatric neurological disorders that are in the developmental pipeline and have the potential to transform care and significantly reduce the burden of disease. This includes a gene therapy for spinal muscular atrophy (SMA) that was approved by the FDA in 2019. Ciafaloni was involved in the clinical trials that led to the therapy’s approval and some of the first children to receive the therapy in the U.S. were patients of the UR Medicine Pediatric Neuromuscular Medicine Program. Last year, it was announced that URMC would be the lead study site for an experimental gene therapy for CNL5 Batten disease, a rare and fatal disorder that first appears in childhood. This study is being led by pediatric neurologist Jonathan Mink, M.D., Ph.D.
In many childhood neurological disorders, spotting the disease before symptoms appear is critical for these new therapies to be effective. Ciafaloni is currently working to get Duchene added to the New York State Newborn Screening Program, a panel of medical tests that screen newborns for 50 different disorders, primarily genetic, that can be more effectively treated if identified earlier. DMD strikes early in life and the target age for the new study is 4-7 years old. In 2018, Ciafaloni, along with others in the medical community and families, successfully convinced the state to add SMA to the list of newborn tests.
Daily Steroids Safe and Slow Progression of Duchenne Muscular Dystrophy
Thursday, May 5, 2022
 New research published in JAMA recommends daily steroid doses for children with Duchenne muscular dystrophy (DMD), marking a significant change in how the disease is treated. University of Rochester Medical Center (URMC) neurologist Robert Griggs, M.D., and Michela Guglieri, M.D., with Newcastle University in the U.K., led the study, which was conducted by a global team of researchers dedicated to improving care for this fatal disease.
New research published in JAMA recommends daily steroid doses for children with Duchenne muscular dystrophy (DMD), marking a significant change in how the disease is treated. University of Rochester Medical Center (URMC) neurologist Robert Griggs, M.D., and Michela Guglieri, M.D., with Newcastle University in the U.K., led the study, which was conducted by a global team of researchers dedicated to improving care for this fatal disease.
“Corticosteroids are likely to remain the main treatment for DMD worldwide for the foreseeable future, so it is critical that we establish a standard of care that is backed by scientific evidence,” said Griggs. “This study shows that health concerns over the daily use of corticosteroids are overstated and that there is a clear benefit in terms of improved motor and pulmonary functions. These findings clearly support the daily regimen over an intermittent one as an initial treatment for boys with DMD.”
DMD is a condition found almost exclusively in boys and characterized by muscle weakness, which appears at age 3-4 and progresses rapidly, leading to significant disability. The symptoms eventually spread to the heart and muscles responsible for breathing, and the disease is often fatal by the time the boy reaches his late teens. An estimated 28,000 people in the U.S. suffer from the disease.
While corticosteroids prednisone and deflazacort are known to improve muscle strength and function in patients with DMD and have been a frontline treatment for years, there is currently no universally accepted standard for steroid use in DMD. A global survey of physicians who treat DMD found 29 different regimens, with the most common being ten days on and ten days off. This intermittent dosing regimen was put in place in an effort to limit the potential side effects associated with prolonged steroid use in children, such as weight gain, stunted growth, and loss of bone density.
The Finding the Optimum Regimen of Corticosteroids for DMD (FOR-DMD) study was launched in 2013 to compare daily and intermittent steroid use and establish, from a clinical benefit and safety perspective, the most beneficial regimen for DMD patients. Griggs and Kate Bushby, M.D., with Newcastle University initiated the phase 3 clinical trial conducted through the Muscle Study Group, an international network of muscular dystrophy researchers that Griggs helped create in 1997 to advance clinical research in neuromuscular disorders, including DMD.
Read More: Daily Steroids Safe and Slow Progression of Duchenne Muscular DystrophyDocumentary Sheds Light on the Parkinson’s ‘Pandemic’
Wednesday, May 4, 2022

 A new documentary, titled The Long Road to Hope, tells the story of individuals with Parkinson’s and efforts to study, treat, and prevent the disease from a global perspective.
A new documentary, titled The Long Road to Hope, tells the story of individuals with Parkinson’s and efforts to study, treat, and prevent the disease from a global perspective.
The documentary was produced by the University of Rochester Center for Heath + Technology (CHeT) and features 12 Parkinson’s patients from the U.S., Canada, the U.K., and the Netherlands and medical commentary from University of Rochester Medical Center neurologist Ray Dorsey, M.D., and Bas Bloem, M.D., Ph.D., with Radboud University Medical Center in the Netherlands.
Parkinson's disease is the fastest growing neurological disorder in the world, outpacing Alzheimer’s, and can be triggered by exposure to pesticides and industrial chemicals. Dorsey and Bloem discuss the pandemic scope of this largely preventable disease and how addressing it will require a global effort with the same level of focus and resources employed with success to address other public health challenges, such as polio, HIV, and breast cancer.
Read More: Documentary Sheds Light on the Parkinson’s ‘Pandemic’Heatwole Appointed Director of CHeT
Wednesday, April 27, 2022
Chad Heatwole, M.D., M.S., has been appointed the new director of the Center for Health + Technology (CHeT) at the University of Rochester. Selected through a national search process, Heatwole took over on a permanent basis on April 25 from Ray Dorsey, M.D., who led the Center since 2013.
“CHeT has a proud history dating back 35 years and has played a leading role in the study and approval of many of the drugs we use today to treat Parkinson’s and other neurological diseases,” said Bob Holloway, M.D., chair of the URMC department of Neurology. “More recently, under Ray’s leadership CHeT has become a pioneer in deploying technologies to improve remote access to specialized care and allow broader participation in clinical research. Chad is well-positioned to lead CHeT into the next chapter and bring patients and communities – across a range of diseases – more into the center of what we do and become true partners in the development of future therapeutics.”
“Chad has played a pivotal role in our Neuromuscular Disease Center, particular the study of myotonic dystrophies, which is recognized as one of the top programs in the world,” said Mark Taubman, M.D., CEO of URMC and dean of the University of Rochester School of Medicine and Dentistry. “He has helped create a robust infrastructure to support clinical trials, which has been instrumental in the growth of the neuromuscular program and we look forward to extending these efforts across the Medical Center, under CHeT. I also want to thank Ray for his transformative leadership and creating a strong foundation which will ensure that CHeT thrives under Chad’s guidance.”
Read More: Heatwole Appointed Director of CHeTArticle Details Baseball Player’s Road to Recovery after Devastating Brain Injury
Monday, February 14, 2022
On July 31 last year, Daniel Brito, third basemen for the Lehigh Valley Iron Pigs, had just taken the field in the bottom of first inning during the first game of a planned double header against the Rochester Red Wings when the unthinkable happened. A tangle of abnormal blood vessels – called an arteriovenous malformation (AVM) – burst in his brain and triggered a seizure. Brito collapsed in the infield, the game was halted, an ambulance was brought onto the field, and he was rushed to UR Medicine’s Strong Memorial Hospital.
While those frightening scenes at Frontier Field were reported by the media, the full story of what occurred that day and Brito’s remarkable journey to recovery from a dangerous and potentially deadly brain injury is only now being fully told in a story appearing in The Athletic.
“Everything that happened to Daniel felt like it was one in a million,” said Debra Roberts, M.D., the director of the UR Medicine Neuromedicine Intensive Care Unit which was Brito’s home for almost two months as he recovered from the damage caused to his brain. “A million in one chance he is born in Venezuela and becomes a professional baseball player. And a million in one chance that he both has an AVM and that it ruptures.”
AVMs are rare, can form at a very young age, and frequently go undetected until it triggers dizziness, headaches, or seizures, which result in the AVM being identified in brain scans and medically managed or surgically removed. While ruptures are rare, occurring in roughly two percent of people with an AVM annually, the consequences can be severe, both in terms of damage to nearby brain tissue, but also the pressure that the bleeding and buildup of fluids puts on the brain. The stress response triggered in the body can also sometimes lead to complications with other organs as the body fights for survival.
Read More: Article Details Baseball Player’s Road to Recovery after Devastating Brain InjuryResident Interviews
Tuesday, February 1, 2022
The Department of Neurology would like to welcome residency applicants, interviewing on Monday, January 9th
Adult Neurology Applicants
Abhilasha Boruah – Case Western Reserve University
Julia Iourinets – Loyola University
In (Josh) Kang – Georgetown University
Aaron Kuang – SUNY Downstate Health Sciences University
Casey Manzanero – SUNY Upstate Medical University
Alexander Mathew – University of Virginia
Sarah Wang – Albert Einstein College of Medicine
Child Neurology Applicants
Destiny Bailey – University of Texas Southwestern Medical School
Hosain Ghassemi – University of Kansas SOM
Colin Huang – University of California San Francisco SOM
Delia Rospigliosi – Baylor COM
Pablo Vazquez – Tufts University SOM
Dr. Jonathan Mink receives Child Neurology Society’s highest honor
Monday, November 22, 2021
Jonathan W. Mink, M.D., Ph.D., the Frederick A. Horner M.D. Distinguished Professor in Pediatric Neurology and Chief of Child Neurology at University of Rochester Medical Center, has been awarded the Child Neurology Society’s (CNS) 2021 Hower Award.
The award is the organization’s highest honor and is given annually to a child neurologist recognized as an outstanding teacher, scholar, and for making high levels of contributions to the field and the CNS, Mink served as president of the CNS from 2017-2019.

Jonathan Mink, M.D. Ph.D.
In his early career, Mink studied the neurobiological basis of Movement Disorders and developed the prevailing model of how the basal ganglia of the brain contribute to motor control. Since moving to the University of Rochester in 2001, he has focused on clinical research in Movement Disorders, including Tourette syndrome, and Batten disease. Mink is a dedicated teacher and mentor and many of his students have gone on to become child neurologists and physician-scientists. He is currently the Director of the University of Rochester Batten Center, co-director of the University of Rochester Tourette Center of Excellence, and co-director of the University of Rochester Intellectual and Developmental Diseases Research Center.
He was recognized at the society’s annual meeting, where he delivered the Hower Award lecture entitled “On Mentors and Protégés: Standing on the Shoulders of Giants and Following Footsteps into the Future.”
“Receiving the Hower Award is a tremendous honor,” Mink said. “I have had the privilege to learn from so many giants and to learn even more from the students, residents, and fellows I have mentored. Each protégé has led me to explore new questions and new directions. The contributions recognized by this award would have not been possible without their inspiration and partnerships.”
The Child Neurology Society is the preeminent non-profit professional association of pediatric neurologists in the United States, Canada, and worldwide.
Read More: Dr. Jonathan Mink receives Child Neurology Society’s highest honorRadiologic Society of North America Recognizes Thomas Johnson, MD, PhD, Department of Neurology
Monday, November 8, 2021
Adolescents and young adults with post- concussive symptoms who suffered three to five concussions showed disruption in the default mode network, an interconnected network of brain regions involved in wakeful rest and internal thoughts. Results of study using a special MRI technique called resting-state functional MRI (fMRI) are being presented at the annual meeting of the Radiological Society of North America (RSNA).
“In the last 20 years, the public awareness of concussion and its long-term effects on the brain has increased and so has research into the topic,” said Thomas Johnson, M.D., Ph.D., a resident physician in neurology at the University of Rochester Medical Center in Rochester, New York. “But there has been scant research using resting state fMRI at the intersection of the adolescent/young adult population and athletes with multiple concussions.”
Dr. Johnson said the study results give clues as to the threshold at which concussions cause effects, which in turn may help inform protocols for playing contact sports following a concussion.
“Suffering three to five concussions has the potential for long-term disruption of cognitive processes,” he said. “We need to determine our tolerance for concussions. When do we say no more contact sports? We need more evidence to set some limits for people.”
In the future, Dr. Johnson said he would like to conduct follow-up research on his study group by scanning the patients with resting-state fMRI in five years to determine whether disruptions in the default mode network remain.
AHA Recognizes UR Medicine for Excellence in Stroke Care
Wednesday, November 3, 2021
The American Heart Association/American Stroke Association has recognized UR Medicine’s Comprehensive Stroke Center for providing lifesaving stroke care, including the administration of interventions capable of improving outcomes, especially when provided as soon as possible after the onset of a stroke.
Strong Memorial Hospital received AHA/ASA’s new Advanced Therapy award, which indicates that surgical intervention was employed in at least 50% of applicable patients within 90 minutes for direct arriving and within 60 minutes for transfer patients. This award was created in recognition of new acute stroke care guidelines that recommend endovascular therapy for eligible patients. Thrombectomy is credited with leading to faster and more complete reperfusion for certain patients and is considered a mainstay of effective stroke care. Strong Memorial is one of only two New York State hospitals outside of New York City to be recognized with Advanced Therapy designation.
Strong Memorial Hospital also received the AHA/ASA’s Stroke Gold Plus with Honor Roll Elite award, which recognizes a door-to-clot-busting medication time within 60 minutes for at least 85 percent of applicable stroke patients.
“We are extremely proud of the teams that provide stroke care across UR Medicine hospitals,” said neurologist Curtis Benesch, M.D. M.P.H., Chief of Stroke and Medical Director of the UR Medicine Comprehensive Stroke Center. “This is truly a system-wide approach that brings together neurologists, neurosurgeons, emergency room physicians, anesthesiologists, technologists, and acute care nurses and providers, and harnesses technologies such as telemedicine to deliver fast, high-quality care regardless to which hospital a stroke patient is transported.”
Read More: AHA Recognizes UR Medicine for Excellence in Stroke CareURMC to Lead First Gene Therapy Study for Batten Disease
Wednesday, November 3, 2021
The University of Rochester Medical Center (URMC) will serve as the lead study site in the U.S. for an experimental treatment being developed by Neurogene for CLN5 Batten disease, a rare and fatal neurodegenerative disorder.
“CLN5 is a devastating and rapidly progressive neurodegenerative disease in children that leads to vision loss, cognitive and motor impairment, seizures and, ultimately, premature death,” said Jonathan W. Mink, M.D., Ph.D., the Frederick A. Horner MD Distinguished Professor in Pediatric Neurology, Chief of Child Neurology at URMC. “This trial will move research forward in developing a potentially disease-modifying treatment for CLN5 disease, providing hope to individuals and families where currently none exists.”
Batten disease is a group of rare, inherited neurodegenerative diseases also called neuronal ceroid lipofuscinoses (NCLs). The CLN5 subtype is caused by a variants in the CLN5 gene, which leads to disruption of normal protein function. The disease will often first appear and be diagnosed in childhood. There are currently no approved treatments that can reverse the symptoms of this disease.
The Medical Center is home to the University of Rochester Batten Center (URBC), which is led by Mink and is one of the nation’s premier centers dedicated to the study and treatment of this condition.
This clinical trial is possible because of the work started back in 2001 by Mink, URMC neurologist Frederick Marshall, and others to understand the natural history of these complex diseases. Working with patients from across the U.S., the team created the Unified Batten Disease Rating Scale, which tracks and quantifies how the different forms of disease progress over time. This tool is employed by researchers across the world to evaluate patients and develop and test new potential therapies.
The planned open-label phase 1/2 clinical trial will evaluate a single intraventricular dose delivered directly into cerebrospinal fluid in the brain. The treatment, called NGN-101, uses an adeno-associated virus to deliver a healthy version of CLN5 gene directly to the central nervous system. Animal studies have shown that the treatment has the potential to halt the key features of disease progression, including vision, motor, cognitive, and behavioral declines.
“At this point for CLN5 disease, what we can offer patients is limited to managing some of their symptoms, and even standard treatment for symptoms like seizures are not consistently effective,” said Mink. “This new study also has the potential to inform development of gene therapies for other forms of the disease. It is a moment that the research community and patients and families have been waiting a long time to come.”
Neurogene’s NGN-101 was recently cleared by the Food and Drug Administration to begin clinical trials and has received Orphan Drug Designation by the U.S. and European regulatory agencies. URMC anticipates enrolling its first study participants in early 2022. Due to the rare nature of CNL5, Mink anticipates that patients from across the U.S. will travel to Rochester to participate in the study. Other URMC researchers involved in the clinical trial include Amy Vierhile, D.N.P. Jennifer Vermilion, M.D., Heather Adams, Ph.D., and Erika Augustine, M.D.
Resident Interviews
Sunday, August 1, 2021
The Department of Neurology would like to welcome residency applicants, interviewing on Monday, January 3rd.
Child Neurology Applicants
Nicholas Benjamin – Drexel University College of Medicine
Cristina Pinto – Rutgers School of Medicine
Arkadip Saha – California Northstate University
Rachel Wlock – Western Michigan University
Benesch and Glance Author New Recommendations on Surgical Stroke Risk
Thursday, June 3, 2021
URMC neurologist Curt Benesch, M.D., M.P.H., and anesthesiologist Laurent Glance, M.D., lead the effort to develop new American Heart Association/American Stroke Association (AHA/ASA) recommendations to lower the risk of perioperative acute stroke.
The statement, which was published in the journal Circulation, focuses on the cerebrovascular complications of non-cardiac surgery and summarizes the current literature concerning the preoperative neurological risk stratification and management of patients before undergoing non-cardiac, non-neurological surgery; intraoperative strategies to mitigate the risk of stroke; and the identification and treatment of patients who experience a perioperative stroke.
Benesch and Glance served as chair and vice chair of a panel of surgeons, anesthesiologists, neurologists, and nurses convened by the AHA/ASA to draft the statement. Robert Holloway, M.D., M.P.H., chair of the Department of Neurology, also served on the panel. The group conducted a literature review that emphasized publications based on randomized, controlled trials, followed by those describing meta-analyses, very large administrative databases and quality registries, and relevant, smaller observational studies. The final scientific AHA/ASA statement was endorsed by the American Academy of Neurology and the American Association of Neurological Surgeons. Benesch and Glance also co-authored an earlier companion paper on the perioperative risks of stroke in patients undergoing cardiac surgery.
Perioperative stroke can be defined as any embolic, thrombotic, or hemorrhagic cerebrovascular event with motor, sensory, or cognitive dysfunction lasting at least 24 hours, occurring intraoperatively or within 30 days after surgery. The incidence of perioperative stroke in patients undergoing non-cardiac, non-neurological surgery is between 0.1% and 1.0%, a number that has risen since 2004 in both men and women and across races and ethnic groups. More than 60% of in-hospital strokes are likely perioperative, occurring on either a surgical service or in the angiography suite.
The new statement stratifies preoperative risk factors, provides guidance on stroke recognition in the perioperative setting, and details stroke prevention strategies, including management of medications, blood pressure, blood transfusion, ventilation, and anesthetic technique. The statement also recommends that large vessel occlusions (LVO) -- ischemic strokes that result from a blockage in one of the major arteries of the brain and represent 10% of perioperative strokes -- be treated via mechanical thrombectomy. In instances where clinical situations lack high-quality clinical trial evidence, recommendations reflect the best evidence available and the consensus of experts to provide pragmatic guidance to practitioners who must make real-world decisions every day in clinical practice.
AHA/ASA Scientific Statements:
Perioperative Neurological Evaluation and Management to Lower the Risk of Acute Stroke in Patients Undergoing Noncardiac, Nonneurological Surgery
Considerations for Reduction of Risk of Perioperative Stroke in Adult Patients Undergoing Cardiac and Thoracic Aortic Operations: A Scientific Statement From the American Heart Association
What’s the story with brain fog and menopause?
Sunday, May 16, 2021
"Growing evidence says this is real," says Miriam Weber, an associate professor of neurology and of obstetrics and gynecology. "Multiple studies have shown declines in memory and attention," she says. "What we don't know is whether it persists. So far it seems like it may be temporary, just through the transition" from perimenopause through menopause.
Gretchen Birbeck Receives Grant to Explore Intersection of Infectious Diseases and Neurological Disorders
Wednesday, May 12, 2021
University of Rochester Medical Center (URMC) neurologist Gretchen Birbeck, M.D., M.P.H., has received a $4.3 million award from the National Institutes of Neurological Disorders and Stroke (NINDS) to continue her research in sub-Saharan Africa on the neurological problems that arise in people recovering from malaria, HIV, and other infectious diseases, including COVID.
The NINDS Research Program Award, which uses the R35 funding mechanism, is given to investigators whose record of research achievement demonstrates an ability to make major contributions to the field of neuroscience. The eight-year award is intended to provide recipients the freedom to embark on ambitious, creative, and longer-term research projects, without the constraints of specific aims.
Birbeck has spent the last 25 years working in Zambia and Malawi in collaboration with local government ministries, medical schools, hospitals, and other U.S.-affiliated neuroscientists to identify the mechanisms of common neurological disorders and improve care through evidence-based interventions and clinical trials. Her research has focused on evaluating outcomes of cerebral malaria and other brain infections in children, and the neurological symptoms that arise from chronic HIV infection and treatments. These diseases -- which are prevalent in sub-Saharan Africa -- have broad effects on cognitive, behavioral, quality-of-life, and economic outcomes.
Birbeck will initially focus on two research projects:
- Nearly one-third of cerebral malaria survivors develop epilepsy or other neurological conditions soon after recovery. Previous research by Birbeck has demonstrated that improved seizure control and management of aggressive fever caused by malaria could provide the key to decreasing the risk of brain injury and developing epilepsy. Birbeck and her team will examine the role of neuroinflammation in structural injury and neurologic morbidity with laboratory assessments of acute inflammation, serial neuroimaging, and long-term neurological outcomes. Researchers will also investigate the effects of co-infection with COVID on children who have recovered from malaria.
- Given the widespread availability of HIV therapies, the next challenge in neuro-HIV care in Africa includes disorders associated with chronic low grade inflammation brought about by the virus and the toxicity of long-term use treatments such antiretroviral drugs. Specifically, studies have shown high rates of cerebrovascular disease in children with HIV, despite long-standing effective treatment of the virus. Utilizing a network of rural and urban HIV clinics, the team will study HIV-associated accelerated aging of the nervous system. Given its highly inflammatory state, the researchers will examine whether COVID could potentially contribute to this burden in children. The team will also see if COVID infection in adults with HIV contributes to cognitive impairment, psychiatric symptoms, strokes, neuropathies, and/or seizures.
The projects involve researchers, clinicians, and students and trainees from URMC, the University of Zambia's University Teaching Hospitals, Queen Elizabeth Central Hospital in Malawi, the University of Malawi College of Medicine, the Centre for Infectious Disease Research in Zambia, and a consortium of rural hospitals in Zambia led by Chikankata Hospital. The research program award will also help provide the infrastructure, mentorship and an environment for scholarship and training for both U.S. and African academics.
Don't sleep much? UK study suggests it could lead to dementia
Wednesday, April 21, 2021
A new study observing the sleep patterns of nearly 8,000 adults in the United Kingdom goes against earlier beliefs about the connection between sleep duration and the possible development of dementia later in life.
"Previous studies have indicated people who sleep excessively, or long sleepers, tend to have an increased risk for dementia," said Dr. Alice Hoagland, a sleep specialist with Rochester Regional Health. "But this is the first study that indicated that people who biologically were short sleepers also had a higher increased risk for dementia."
The study followed people for 25 years, beginning when they were age 50. It found that people who slept six hours or less had a higher risk of being diagnosed with dementia in their 70s.
Doctors with both Rochester Regional Health and the University Rochester Medical Center had many questions about the study - and not all of them could be answered based on the findings.
"I would be very hard pressed to say that being a very short sleeper, sort of staying up late at night and getting up early in the morning and all that, is predictive of developing dementia because we simply don't know which way this goes," said Dr. Alice Hoagland, director of Rochester Regional Health's Insomnia Clinic.
"Whether these are people who just naturally get six hours of sleep or less - because there are people who are like that - or whether these are people who would like to sleep longer and they just can't because they don't have the opportunity, that's yet to be seen," said said Dr. Michael Yurcheshen, a professor of neurology and sleep medicine with URMC.
"We certainly do see patients in our practice here who do get six or fewer hours of sleep who do seem to function just fine," said Dr. Yurcheshen.
Rates of Parkinson’s disease are exploding. A common chemical may be to blame
Thursday, April 8, 2021
Asked about the future of Parkinson's disease in the US, Dr Ray Dorsey says, "We're on the tip of a very, very large iceberg."
Dorsey, a neurologist at the University of Rochester Medical Center and author of Ending Parkinson's Disease, believes a Parkinson's epidemic is on the horizon. Parkinson's is already the fastest-growing neurological disorder in the world; in the US, the number of people with Parkinson's has increased 35% the last 10 years, says Dorsey, and "We think over the next 25 years it will double again."
Most cases of Parkinson's disease are considered idiopathic -- they lack a clear cause. Yet researchers increasingly believe that one factor is environmental exposure to trichloroethylene (TCE), a chemical compound used in industrial degreasing, dry-cleaning and household products such as some shoe polishes and carpet cleaners.
Clinical trials are moving out of the lab and into people’s homes
Thursday, February 18, 2021
After the pandemic forced thousands of trials to shut down, researchers found clever ways to conduct human studies remotely — while reaching more people, quickly and cheaply.
Remote trials are likely to persist in a post-pandemic era, researchers say. Cutting back on in-person visits could make recruiting patients easier and reduce dropout rates, leading to quicker, cheaper clinical trials, said Dr. Ray Dorsey, a neurologist at the University of Rochester who conducted remote research for years.
In fact, he noted, enrollment in one of his current virtual studies, which is tracking people with a genetic predisposition to Parkinson's, actually surged last spring. "While most clinical studies were paused or delayed, ours accelerated in the midst of the pandemic," he said.
New Research Sheds Light on Vision Loss in Batten Disease
Friday, February 5, 2021
 Progressive vision loss, and eventually blindness, are the hallmarks of juvenile neuronal ceroid lipofuscinosis (JNCL) or CLN3-Batten disease. New research shows how the mutation associated with the disease could potentially lead to degeneration of light sensing photoreceptor cells in the retina, and subsequent vision loss.
Progressive vision loss, and eventually blindness, are the hallmarks of juvenile neuronal ceroid lipofuscinosis (JNCL) or CLN3-Batten disease. New research shows how the mutation associated with the disease could potentially lead to degeneration of light sensing photoreceptor cells in the retina, and subsequent vision loss.
"The prominence and early onset of retinal degeneration in JNCL makes it likely that cellular processes that are compromised in JNCL are critical for health and function of the retina," said Ruchira Singh, Ph.D., an associate professor in the Department of Ophthalmology and Center for Visual Science and lead author of the study which appears in the journal Communications Biology. "It is important to understand how vision loss is triggered in this disease, what is primary and what is secondary, and this will allow us to develop new therapeutic strategies."
Batten disease is caused by a mutation in the CLN3 gene, which is found on chromosome 16. Most children suffering from JNCL have a missing part in the gene which inhibits the production of certain proteins. Rapidly progressive vision loss can start in children as young as 4, who eventually go on to develop learning and behavior problems, slow cognitive decline, seizures, and loss of motor control. Most patients with the disease die between the ages of 15 and 30.
It has been well established that vision loss in JNCL is due to degeneration of the light-sensing tissue in the retina. The vision loss associated with JNCL can precede other neurological symptoms by many years in some instances, which often leads to patients being misdiagnosed with other more common retinal degenerations. However, one of the barriers to studying vision loss in Batten disease is that mouse models of CLN3 gene mutation do not produce the retinal degeneration or vision loss found in humans. Additionally, examination of eye tissue after death reveals extensive degeneration of retinal cells which does not allow researchers to understand the precise mechanisms that lead to vision loss.
URMC is a hub for Batten disease research. The Medical Center is home to the University of Rochester Batten Center (URBC), one of the nation's premier centers dedicated to the study and treatment of this condition. The URBC is led by pediatric neurologist Jonathan Mink, M.D., Ph.D., who is a co-author of the study. Batten disease is also one of the key research projects that will be undertaken by the National Institute of Child Health and Human Development-supported University of Rochester Intellectual and Development Diseases Research Center.
To study Batten disease in patient's own cells, the research team reengineered skin cells from patients and unaffected family members to create human-induced pluripotent stem cells. These cells, in turn, were used to create retinal cells which possessed the CLN3 mutation. Using this new human cell model of the disease, the new study shows for the first time that proper function of CLN3 is necessary for retinal pigment epithelium cell structure, the cell layer in the retina that nourishes light sensing photoreceptor cells in the retina and is critical for their survival and function and thereby vision.
Singh points out that understanding how RPE cell dysfunction contributes to photoreceptor cell loss in Batten disease is important first step, and it will enable researchers to target specific cell type in the eye using potential future gene therapies, cell transplantation, and drug-based interventions.
Additional co-authors of the study include Cynthia Tang, Jimin Han, Sonal Dalvi, Kannan Marian, Lauren Winschel, Celia Soto, Chad Galloway, Whitney Spencer, Michael Roll, Lisa Latchney, Erika Augustine, Vamsi Gullapalli, and Mina Chung with URMC, David Williams and Stephanie Volland with the University of California, Los Angeles, Vera Boniha with the Cleveland Clinic, and Tyler Johnson with Sanford Research. The research was supported with funding from the National Eye Institute BrightFocus Foundation, the David Bryant Trust, the Foundation of Fighting Blindness, the Knights Templar Eye Foundation, the Retina Research Foundation, and Research to Prevent Blindness.
Ann Leonhardt Caprio elected as a Fellow of the AHA
Saturday, January 2, 2021
We are pleased to announce that Ann Leonhardt Caprio, DNP, RN, ANP-BC, UR Comprehensive Stroke Center Program Coordinator, has recently been named as a Fellow of the American Heart Association (FAHA), Council of Cardiovascular and Stroke Nursing. Highly competitive, election as a FAHA recognizes the recipient's scientific accomplishments, volunteer leadership and service. Earning the FAHA credential demonstrates to colleagues and patients that the recipient has been welcomed into one of the world's most eminent organizations of cardiovascular and stroke professionals.
Fellowship recognizes leaders within the AHA who have made significant contributions to the field of cardiovascular and cerebrovascular science and medicine. FAHA demonstrate outstanding credentials and achievement, contribute to the AHA through involvement at the local, affiliate, and/or national level, and receive a strong recommendation from leaders in their field.
Blog: Are the new mRNA vaccines safe?
Wednesday, December 30, 2020

John Lueck
Joanne Ladolcetta, a freelance writer based out of San Francisco, wanted to put together information to help address circulating fears and misconceptions about the recently FDA approved COVID-19 mRNA vaccines. She reached out to friends Bryant Johnson (Cartoonist) and John Lueck (Researcher at the University of Rochester Medical Center) to tackle some of the most common vaccine questions. The collaboration resulted in an approachable informative write-up with creative illustrations and helpful links to provide readers the ability to do a deeper dive into the generation and application of the novel COVID-19 mRNA vaccines.

Courtesy of Bryant Johnson
Read More: Blog: Are the new mRNA vaccines safe?
Welcome Resident Applicants for January 11th
Wednesday, December 30, 2020
The Department of Neurology would like to welcome residency applicants, interviewing on Monday, January 11th.
Adult Neurology Applicants
George Cappos -- University of Florida
Avinash Kolli -- Loyola University Chicago Stritch School of Medicine
Abena Kwegyir-Aggrey -- Pennsylvania State University
Sloan Lynch -- Boston University
Benjamin Meyer -- Columbia University
Stephanie Reyes -- University of Michigan
William Signorile, III -- Stony Brook University
Child Neurology Applicants
Serina Bsales -- Rutgers, Robert Wood Johnson Medical School
Anthony Di Caro -- New York Institute of Technology College of Osteopathic Medicine
Shama Khan -- Drexel University College of Medicine
Rima Madan -- State University of New York Upstate Medical Center
Welcome Resident Applicants for January 12th
Wednesday, December 30, 2020
The Department of Neurology would like to welcome residency applicants, interviewing on Monday, January 12th.
Adult Neurology Applicants
Mary Abramczuk -- Drexel University
Tiffany Kyo -- Case Western Reserve University
Amanda Lin -- Wright State University
Chiedza Mupanomunda -- Northwestern University
Jennifer Purks -- Georgetown University
Ilana Selli -- University of Buffalo
Bright Spots for Digital Technologies in the Midst of a Global Pandemic
Thursday, December 3, 2020
Lockdowns and social distance have led to new digital health technologies becoming crucial tools in fighting the pandemic. "Digital health technologies such as telemedicine have been vital in addressing certain health needs that local health systems are not able to handle," Valerie Shelly, program manager, ACCESS Health shared.
According to Ray Dorsey, director of the Center for Health and Technology at the University of Rochester Medical Center, the majority of patient consultations in the U.S. are now happening virtually, and there's been at least a ten-fold increase in virtual checkups in recent weeks.
The question technology companies should ask themselves is how to sustain the use of these effective telehealth services after the pandemic subsides.
New IDD Research Center Begins Work with Principal Project on Batten Disease
Thursday, November 5, 2020
The principal project of the Intellectual and Developmental Disabilities Research Center (IDDRC) will focus on Batten disease, specifically CLN3 disease, also known as juvenile-onset Batten disease. Children with this rare genetic disorder start developing symptoms such as vision loss, impaired motor control, seizures, and dementia between 5-10 years of age. The University of Rochester Batten Center (URBC) is a recognized leader in research and treatment of this condition. With several potential gene therapies for Batten disease currently in advanced stages of development, URMC will focus on identifying biomarkers to evaluate the effectiveness of these experimental treatments.
"Even within individual families, we have learned that each diagnosed child may have a different disease experience in terms of the age of symptom onset, pattern of symptom progression, and the types of burdens experienced by them and their families," said Heather Adams, Ph.D., associate professor in the departments of Neurology and Pediatrics and coinvestigator of the UR IDDRC Principal Project. "We cannot miss any opportunity to learn from affected individuals."
Patients and families from across the U.S. come to URMC for care and to participate in research. While some visit labs in Rochester equipped to work with these patients and their families, in many instances a mobile URBC lab will travel to them. "Research is the main way that we feel like we contribute to the Batten community. We try to support research as much as we can. It is how we feel connected, doing what we can to help everyone's effort," said Bridget Patterson who lives in Virginia. Two of her four children, Nora and Gabriel, have Batten disease. "A disease like this really does affect the whole family. We have two other children that are not affected, but they feel the effects of the disease every day. I know that helping their lives be better too is one reason why we are involved in this research. If we can find a cure, a treatment, Nora and Gabriel would be the ones most dramatically impacted but it would help all of us."
There are 11 other currently known childhood-onset forms of Batten disease, genetically distinct from one another, and all have significant impacts on neurodevelopment. URBC is designated a Center of Excellence by the Batten Disease Support and Research Association.
New research examines COVID-19 impact on aging brain
Thursday, September 24, 2020
Researchers at the University of Rochester Medical Center (URMC) and Duke University Medical Center will collaborate on a study that investigates why some older patients, who become severely ill from COVID-19, develop delirium that can lead to brain damage and a dementia diagnosis.
Nearly 30-percent of patients hospitalized with COVID-19 develop delirium -- a state of confusion and impaired awareness. For severely ill patients the likelihood of delirium is closer to 70-percent. "The initial delirium, and then the cognitive, behavioral, and emotional problems -- commonly known as dysexecutive syndrome -- were arguably the most notable things in older people that had managed to survive COVID-19," said Harris Gelbard, M.D., Ph.D. Professor and Director, Center for Neurotherapeutics Discovery, who is also the principal investigator at URMC on this study which is being funded by the National Institute of Aging. "Nobody knows whether that's permanent or not because of the advanced age of the people this is impacting."
Using a model for inhaled lipopolysaccharide-based acute lung injury in mice to mimic what happens in the lungs of a severally ill COVID-19 patient, Gelbard and his colleague Niccolo Terrando, Ph.D. at Duke University Medical Center will look for specific events in the neurovascular unit —brain endothelial cells and their blood-brain barrier (BBB) forming tight junctions that support the central nervous system -- that can be traced back to cognitive impairment. Part of the hypothesis Gelbard is investigating is that scarring in the lung may cause platelets and inflammatory white cells to migrate to blood vessels in the central nervous system with the white cells traversing the BBB to cause neurologic disease. "The goal is to establish what the prerequisites are for lung injury that will lead to brain injury. And at that point, then we can start asking more complicated questions."
The researchers will also investigate how the body responds to URMC-099, an anti-inflammatory and neuroprotective agent developed by Gelbard, to prevent these sequelae. The use of behavior analysis at Duke and in vivo brain imaging at URMC will determine delirium-like changes in the mice.
Gelbard and Terrando are confident that this study will lead to a larger and longer study of the impact COVID-19 has on the brain of an older population. "If you could do something to prevent that in the first place, chances are you are going to do better, down the road."
Program to Create National Model of Support for Parkinson’s Patients
Tuesday, September 22, 2020
The University of Rochester Medical Center (URMC) in collaboration with the Parkinson's Foundation is developing a palliative care program that will be become the standard of care in the organization's 33 Centers of Excellence clinics across the U.S.
The initiative -- which is being funding with $1.6 million in support from the federal Patient-Centered Outcomes Research Institute (PCORI) -- is led by URMC neurologist Benzi Kluger, M.D., a professor of Neurology and Medicine and director of URMC's new Palliative Care Research Center.
Kluger and his current and former colleagues in Rochester and the University of Colorado have developed an innovative model of palliative care delivery consisting of interdisciplinary teams of providers that address the needs of Parkinson's patients and their families as they grapple with the physical, emotional, social, and spiritual symptoms of their disease. In a previous PCORI-funded study published earlier this year in JAMA Neurology, Kluger and his team demonstrated that outpatient palliative care improves quality of life and other outcomes, including reductions in caregiver burden and improvement in motor symptoms.
The Parkinson's Foundation Centers of Excellence program recognizes medical centers that have brought together teams of neurologists, movement disorder specialists, physical and occupational therapists, and mental health professionals, and provide high levels of support and care for Parkinson's patients.
Kluger and his team are developing virtual training programs tailored to the unique needs and circumstances of each clinic. The program will provide caregivers with the tools, resources, and skills to deliver a patient-centered model of care that effectively addresses psychosocial issues patients are experiencing, provides support to families and care partners, screens for non-motor symptoms like pain and depression, and encourages the development of advanced care roadmaps for individual patients.
Nedergaard Honored for Alzheimer’s Research
Tuesday, September 15, 2020
Maiken Nedergaard, M.D., D.M.Sc. has been awarded the International Prize for Translational Neuroscience of the Gertrud Reemtsma Foundation for her research in the glymphatic system, the brain's unique waste removal process.
Nedergaard's research was recognized by the Foundation for findings that "offer new approaches for treatments and preventive measures for Alzheimer's and other neurodegenerative diseases."
First discovered by researchers in the URMC Center for Translational Neuromedicine in 2012, the glymphatic system piggybacks on blood vessels and pumps cerebrospinal fluid, washing waste from the brain. The accumulation of toxic proteins like beta amyloid are linked neurological disorders, including Alzheimer's disease. Nedergaard's lab has since gone on to show how sleep disruption, age, and injury can impair the brain's ability to effectively remove waste.
Nedergaard was presented the award at a ceremony at the Max Plank Society in Cologne, Germany on September 10.
URMC Tapped to Advance Research in Intellectual and Developmental Disabilities
Wednesday, July 8, 2020
The University of Rochester has been designated an Intellectual and Developmental Disabilities Research Center (IDDRC) by the National Institute of Child Health and Human Development (NICHD). The award recognizes the Medical Center's national leadership in research for conditions such Autism, Batten disease, and Rett syndrome, will translate scientific insights into new ways to diagnose and treat these conditions, and provide patients and families access to cutting edge care.
The IDDRC at the University of Rochester will be led by John Foxe, Ph.D., director of the Del Monte Institute for Neuroscience, and Jonathan Mink, M.D., Ph.D., chief of Child Neurology at Golisano Children's Hospital. The designation is accompanied with more than $6 million in funding from NICHD.
New Therapy Reduces Chronic Low Back Pain in Large International Study
Friday, June 19, 2020
A new study hasfound that tanezumab, a monoclonal antibody that inhibits nerve activity, provides relief in patients with chronic low back pain, one of the leading reasons why people seek medical care and the number one cause of disability worldwide.
"This demonstration of efficacy is a major breakthrough in the global search to develop non-opioid treatments for chronic pain," said John Markman, M.D., director of the Translational Pain Research Program in the University of Rochester Medical Center (URMC) Department of Neurosurgery and lead author of the study which appears in the journal Pain. "There were also improvements in function linked to the reduction in pain severity."
This is the first study that shows long-term relief for chronic low back pain with a single dose of tanezumab delivered under the skin once every two months. The study was conducted in 191 sites across eight countries in North America, Europe, and Asia.
Researchers are increasingly finding that certain proteins circulating in the bloodstream heighten the sensitivity of cells in the nervous system to pain. One of these proteins, called nerve growth factor (NGF), may explain why some individuals experience more intense and chronic back pain. Tanezumab is an NGF inhibitor.
The patients with chronic low back pain enrolled in this study did not previously have relief with at least three different types of pain medication, including opioids, and were considered "difficult-to-treat." Patients with symptoms, signs, and x-ray evidence of moderate-to-severe osteoarthritis, a disorder commonly found in older patients with chronic low back pain, were excluded from the study.
Animal Study Shows Human Brain Cells Repair Damage in Multiple Sclerosis
Tuesday, May 19, 2020
A new study shows that when specific human brain cells are transplanted into animal models of multiple sclerosis and other white matter diseases, the cells repair damage and restore function. The study provides one of the final pieces of scientific evidence necessary to advance this treatment strategy to clinical trials.
"These findings demonstrate that through the transplantation of human glial cells, we can effectively achieve remyelination in the adult brain, " Steve Goldman, M.D., Ph.D., professor of Neurology and Neuroscience at the University of Rochester Medical Center (URMC), co-director of the Center for Translational Neuromedicine, and lead author of the study. "These findings have significant therapeutics implications and represent a proof-of-concept for future clinical trials for multiple sclerosis and potential other neurodegenerative diseases."
The findings, which appear in the journal Cell Reports, are the culmination of more than 15 years of research at URMC understanding support cells found in the brain called glia, how the cells develop and function, and their role in neurological disorders.
Goldman's lab has developed techniques to manipulate the chemical signaling of embryonic and induced pluripotent stem cells to create glia. A subtype of these, called glial progenitor cells, gives rise to the brain's main support cells, astrocytes and oligodendrocytes, which play important roles in the health and signaling function of nerve cells.
Study by John Markman Points to New Way of Assessing Patient Pain
Monday, April 20, 2020
The professor of Neurosurgery and Neurology found that asking, "Is your pain tolerable" in conjunction with the traditional 0-10 scale can help doctors better understand whether treatment — including opioids — is necessary.
New COVID-19 Neurology Link
Wednesday, March 25, 2020
We have added a new link to the Neurology Intranet Page under the General Links to the left. Clicking on the COVID-19 Neurology link will take you to a BOX folder with access to files containing current COVID-19 information related to Neurology. If you are not logged into BOX, you will be prompted to log in. If you do not have a BOX account, please contact NeurologyIT at 5-0431 and they will create an account for you.
New Book Details Roadmap to Prevent and Treat Parkinson’s
Wednesday, March 11, 2020
A new book titled "Ending Parkinson's Disease: A Prescription for Action" and authored by University of Rochester Medical Center neurologist Ray Dorsey, M.D. and his colleagues, lays out a new vision to prevent, advocate for, care for, and treat this major and growing global health threat.
"Parkinson's disease is a looming pandemic and we are woefully unprepared to meet this challenge -- many people remain undiagnosed and untreated, research funding for the disease has stagnated, and the most effective treatment is now a half century old," said Dorsey, the David M. Levy Professor of Neurology and director of the Center for Health + Technology (CHeT). "At least some cases of Parkinson's are man-made and, therefore, preventable."
Parkinson's disease is the fastest growing neurological disorder in the world, outpacing Alzheimer's.Over the past 25 years, the number of people with the condition has jumped from three million to more than six million, and by 2040, it is projected to double again.
First described in early 18th century London at the height of the Industrial Revolution, Parkinson's and its rise have been fueled by environmental exposures to harmful chemicals. The two biggest culprits currently still in use are paraquat, a herbicide widely used in the U.S. despite being banned in 32 countries, and trichloroethylene (TCE), a solvent used in a wide range of industrial and consumer products. Not only are agricultural and industrial workers at risk of exposure, but these chemicals also enter the food chain, water supply, reside in the soil in brownfield sites, and impact indoor air quality.
The authors also advocate removing barriers to care. For example, over 40 percent of individuals with the disease do not see a neurologist soon after diagnosis, primarily because of where they live. Technologies like telemedicine have been shown to deliver effective specialized care to patients and improves their lives. However, Medicare policies often do not pay for these services.
Confronting the Parkinson's pandemic will require marshalling the same focus and resources employed with success to address other public health challenges, such as polio, HIV, and breast cancer. The authors label their course of action PACT: prevent the disease, advocate for policies and resources, care for all affected, and treat the condition with new and more effective therapies.
URMC has a long been a leader in the field of Parkinson's research and care. Medical Center researchers were instrumental in conducting pivotal clinical trials that led to at least four FDA-approved drugs currently treat the disease. CHeT is a leading center for the application of new technologies to study and assess Parkinson's. The themes detailed in the book will form the basis of a new initiative launched by URMC in the coming months that will focus on the research, grassroots advocacy, and public policy steps necessary to prevent the disease and expand access to care.
Additional co-authors of the book include Todd Sherer, Ph.D., CEO of the Michael J. Fox Foundation, Mike Okun, M.D., with the University of Florida, and Bastiaan R. Bloem, M.D., Ph.D., with Radboud University in the Netherlands. Proceeds from sales of the book will support Parkinson's research at URMC and other institutions.
Kluger to Lead New Palliative Care Research Initiative
Wednesday, March 4, 2020
Benzi Kluger, M.D., has been tapped to lead palliative care research across URMC. Kluger comes to URMC from the University of Colorado School of Medicine and started at the Medical Center on January 1.
Kluger, who has been appointed a professor of Neurology and Medicine, is the director of URMC's new Palliative Care Research Center within the Department of Medicine. In this role, he will develop resources and core infrastructure to enable researchers and clinicians from across the University to undertake palliative care research projects.
"Dr. Kluger has established himself as a leading researcher and scholar in both neurological disorders and palliative care," said Bob Holloway, M.D., M.P.H., chair of the Department of Neurology. "We are fortunate to have recruited him to Rochester and look forward to helping him have a major impact on the field of palliative care."
"In his young and blossoming career Benzi has already gained international recognition as a productive, creative scholar in the realm of innovative palliative care delivery models," said Robert Horowitz, MD, chief of the Palliative Care Division at URMC. "He is an ambitious, generative, and prolific scholar, clinician, teacher and human being, with an explicit commitment to building ties across UR schools, departments, and divisions."
Kluger's specific interest is in innovative models of palliative care delivery, in which an interdisciplinary team addresses the many needs of seriously ill patients and their families, as they grapple with the physical, emotional, social, and spiritual symptoms of their disease. Kluger is working with faculty in the Wilmot Cancer Center, Divisions of Palliative Care and Nephrology, the School of Nursing, and other Medical Center departments and divisions to develop and evaluate integrated models of outpatient palliative care. Kluger will also oversee the creation of a new Neuropalliative Care Division within the Department of Neurology.
With support from a PCORI grant, Kluger led a multisite randomized controlled trial in Colorado that compared the effectiveness of multidisciplinary outpatient palliative care integrated with standard care versus standard care alone for Parkinson's patients. The results of the study, which were published earlier this month in JAMA Neurology, showed that outpatient palliative care improves quality of life and other outcomes, including reductions in caregiver burden and improvement in motor symptoms.
"Palliative care provides a framework to address the multiple needs of patient populations from the time of diagnosis and is particularly beneficial when people reach more into more advanced stages of illness where our traditional care models have less to offer," said Kluger. "This effort is part of a wider movement to make palliative care a standard and expected part of care for persons living with serious diseases."
Kluger conducted his Medical and Neurology Residency training at the University of Colorado. He completed fellowship training in Behavioral Neurology and Movement Disorders at the University of Florida. He recently established the International Society of Neuropalliative Care (ISPN), which has members from US, Canada, Europe, Asia and Australia, and will be the organization's first president. Kluger and Holloway are co-editors of the book "Neuropalliative Care: A Guide to Improving the Lives of Patients and Families Affected by Neurological Disease."
The ANA Q&A: Neurology Research in Sub-Saharan Africa
Tuesday, March 3, 2020
"One hears a lot about malaria deaths, but the sad reality is that a third of survivors sustain a brain injury with associated neurological sequelae. More than 200,000 African children each year end up with neurodisabilities from malaria. This is low-hanging fruit for decreasing the global burden of neurological disease and increasing the human capacity in this region of the world."
~Gretchen Birbeck, M.D., M.P.H., Professor of Neurology, ANA International Outreach Committee Chair
To celebrate International Women's Day (March 8), we're highlighting ANA members who are doing impressive work both domestically and abroad. Keep reading for our interview with Gretchen Birbeck, M.D., M.P.H. Dr. Birbeck is a neurologist who divides her time between the U.S. and Africa. Her U.S. academic home is the University of Rochester, where she is the Rykenboer Professor of Neurology. She also serves as chair of the ANA's International Outreach Committee.
We spoke with her to learn more about her research, her work with the International Outreach Committee, and what the theme of this year's International Women's Day, "Each for Equal," means to her.
Can you give an overview of the initiatives you've been working on in Zambia?
My work in Zambia really mirrors what an academic neurologist does anywhere—I teach, provide clinical care and conduct research. And for me the split is about 70/30 with the largest proportion of my time being spent on research activities.
On the research front, I am the Principal Investigator for three NIH-funded R01s. The ChASE study is a Cohort Study of HIV-Associated Seizures and Epilepsy. One of the clinical challenges in providing neurological care in sub-Saharan Africa is knowing what to do for someone who is HIV infected presenting with new onset seizure. Epidemiological data that otherwise informs if and when to start a chronic antiseizure medication may not apply to persons with HIV especially if an HIV-associated drug reaction or opportunistic infection has precipitated the seizure. And unfortunately, the choice of seizure medications may be limited to enzyme-inducing agents that interact with antiretroviral medications. ChASE is providing some insights on what causes seizures in this population, who is at risk of long-term seizure disorders and what happens when the seizure medications available in HIV endemic regions are combined with the HIV medications used locally. This is an especially dynamic study as it involves adults and children in rural and urban populations. I spent the first two decades of my time in Zambia based in a rural area and I still have excellent research teams and colleagues there so it is wonderful to remain working and engaged with them even though I am now based primarily in Lusaka.
I am also working on the Malaria Fever study which is a randomized controlled trial (RCT) of aggressive antipyretic therapy using maximal dose ibuprofen and acetaminophen for fever control in pediatric malaria. My K23 project was a prospective cohort study of neurological outcomes in pediatric cerebral malaria survivors. Since completing my K23, I've been working down the list of potentially modifiable risk factors for brain injury in this population hoping to eventually conduct a multi-country RCT of a neuroprotective "package" of care to improve outcomes in child survivors of cerebral malaria. One hears a lot about malaria deaths, but the sad reality is that a third of survivors sustain a brain injury with associated neurological sequelae. More than 200,000 African children each year end up with neurodisabilities from malaria. This is low-hanging fruit for decreasing the global burden of neurological disease and increasing the human capacity in this region of the world. I also think what we learn about epileptogenesis from the cerebral malaria model may help us understand the process in general and this has implications for advances in neurological care everywhere.
Finally, the MRI Ancillary Grant is an imaging study of children enrolled in the Malaria Fever study. This is evaluating structural evidence of brain injury to potentially identify neuroprotective effects and/or side effects from the antipyretics that won't necessarily be mediated by fever control. This is really an important additional outcome for the RCT since it is quite possible that the anti-inflammatory benefits of the antipyretics might be neuroprotective yet not significantly reduce fever. But the addition of imaging may also help us better identify adverse effects from the antipyretics. One of the neurological phenomena that occurs in pediatric cerebral malaria is the development of brain microhemorrhages. These feature prominently among autopsy findings and, more recently, our research team identified microhemorrhages in children who survived cerebral malaria. So, one major concern is that children who receive ibuprofen (which is not standard of care for malaria fevers) may have an increased risk of microhemorrhages or frank bleeding. The MRI Ancillary Grant will allow us to see if this is occurring.
Clinically, I have an epilepsy clinic in rural Zambia that I staff weekly, I pinch hit for attending on child neurology consults when needed on the inpatient service and I read EEGs Zambia at the University Teaching Hospitals (UTH) Children's Hospital and Malawi for Queen Elizabeth Central Hospital's Pediatric service.
On the teaching front, there is a new postgraduate training program in neurology now at UTH and it is doing an amazing job of transforming care and education here. I can't take any credit for the program, which is led by Dr. Deanna Saylor (Johns Hopkins) and was co-founded by Dr. Omar Siddiqi (Beth Israel at Harvard), but I will proclaim myself to be the program's biggest cheerleader. And in this vibrant environment, I'm able to spend my medical education endeavors primarily as a mentor for young researchers, both American and African. My mentees study stigma, nutritional neuropathies, cognition in adolescents with HIV, TB meningitis, the impact of health system structure on neurological care delivery, CNS IRIS, and comorbid HIV and NCDs.
So, things are busy and chaotic, but never boring!
Parkinson's Foundation Charity Hockey Game
Friday, January 17, 2020
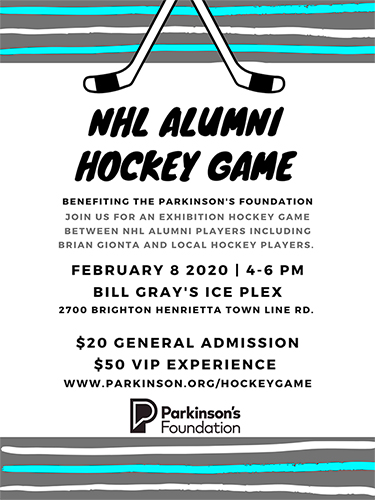
The Parkinson's foundation is putting on a charity hockey game Saturday February 8th from 4-6pm. I will be participating in the event showing washed up NHL players how it's done along with raising money by selling tickets for a good foundation and cause so anyone that can make the game and support it would be amazing! They are asking players to sell tickets (in the "purchasing from a player" box (Here's the link)) and I thought who better to ask than the people that work hands on with Parkinson's disease. Thanks, everyone!
Justin Alves,
Human Subject Research Coordinator
Amy Chesire, L-CSW-R, MSG was recently recognized by the Huntington Study Group as Coordinator of the Year!
Tuesday, December 10, 2019
The Huntington Study Group, which was founded in 1993, is a research organization that is devoted to finding new treatments for Huntington's disease. The group includes more than 400 investigators and coordinators from over 100 research sites. Amy has been Instrumentally involved with our Huntington's disease program for more than twenty years. Her commitment to the Huntington's disease community is unparalleled. She is compassionate, knowledgeable, reliable and engaged at all levels of care for patients and families: local, regional, national and international. It is an honor to continue to work with and learn from her. Congratulations, Amy!
CMSU Tapped for ALS Clinical Trial Initiative
Thursday, November 14, 2019
The Clinical Materials Services Unit (CMSU) has been awarded the contract to provide drug supply and distribution services to the for a new clinical research initiative that seeks to rapidly evaluate new drug candidates for Amyotrophic Lateral Sclerosis (ALS).
The HEALEY ALS Platform Trial -- which will be conducted by the Sean M. Healey & AMG Center at Massachusetts General Hospital -- is a new clinical trial initiative in which studies of investigational ALS treatments are tested and evaluated simultaneously. New treatments can be added to the study as they become available. This approach has already proven successful in the cancer field and will greatly accelerate therapy development by allowing investigators to test more drugs, increase patient access to trials, and reduce the cost by quickly and efficiently evaluating the effectiveness of multiple therapies.
Three drugs developed by Biohaven Pharmaceuticals, RA Pharma, and Clene Nanomedicine will be the first to participate in the platform trial. CMSU will be responsible for providing clinical supply chain management, packaging, labeling, distribution, and return services for all the drugs used in the platform study.
CMSU is led by senior research associate Cornelia Kamp, M.B.A., and director of Clinical and Business Affairs Patrick Bolger, R.Ph., M.B.A., and is a core research unit of the Center for Health + Technology (CHeT). Over the past 11 years CMSU has provided clinical supply services to 60 multi-center clinical trials conducted in the US, Canada, New Zealand and Australia supported with funding from the NINDS, NCCAMS, NICHD, NEI, Michael J. Fox Foundation, DOD, FDA, and numerous pharmaceutical and biotech companies. At any given time, CMSU supports between 15-20 clinical trials. CMSU recently moved to its new location at 150 Metro Park in Rochester.
URMC-099 Combats Surgery-Induced Delirium, Cognitive Dysfunction in Preclinical Model of Orthopedic Surgery
Wednesday, November 6, 2019
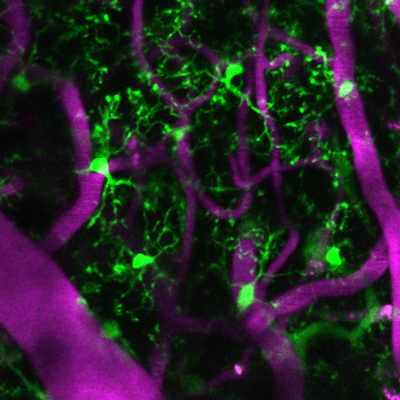
Living microglia, genetically marked to glow green, in the cerebral cortex with magenta colored blood vessels from a mouse treated with URMC-099.
A new study published in the Journal of Neuroinflammation found that prophylactic treatment with URMC-099 -- a "broad spectrum" mixed-lineage kinase 3 inhibitor -- prevents neuroinflammation-associated cognitive impairment in a mouse model of orthopedic surgery-induced perioperative neurocognitive disorders (PND).
PND, a new term that encompasses postoperative delirium, delayed neurocognitive recovery, and postoperative neurocognitive disorder, is the most common complication after routine surgical procedures, particularly in the elderly. Following surgery, such as hip replacement or fracture repair, up to 50 percent of patients experience cognitive disturbances like anxiety, irritability, hallucinations, or panic attacks, which can lead to more serious complications down the line. Currently, there are no FDA-approved therapies to treat it.
Developed in the laboratory of Harris A. "Handy" Gelbard, M.D., Ph.D., director of the Center for Neurotherapeutics Discovery at the University of Rochester Medical Center, URMC-099 inhibits damaging innate immune responses that lead to inflammation in the brain and accompanying cognitive problems. Using animal models of diseases like HIV-1-associated neurocognitive disorders, Alzheimer's disease and multiple sclerosis, Gelbard has shown that the compound blocks enzymes called kinases (such as mixed lineage kinase type 3, or MLK3) that respond to inflammatory stressors inside and outside cells.
Gelbard and Niccolò Terrando, Ph.D., director of the Neuroinflammation and Cognitive Outcomes laboratory in the Department of Anesthesiology at Duke University Medical Center, used an orthopedic surgery mouse model that recapitulates features of clinical procedures such as a fracture repair or hip replacement, which are often associated with PND in frail subjects. In a pilot experiment, they treated one group of these mice with URMC-099 before and after surgery, and another group prior to surgery only. Gelbard and Terrando's teams, including first author Patrick Miller-Rhodes, a senior pre-doctoral student in the Neuroscience Graduate Program working in the Gelbard lab at URMC, measured the following:
- How the surgery affected the central nervous system and the immune cells (microglia) that reside there was evaluated using stereology and microscopy.
- Surgery-induced memory impairment was assessed using the "What-Where-When" and Memory Load Object Discrimination tasks.
- The acute peripheral immune response to surgery was assessed by cytokine/chemokine profiling and flow cytometry.
- Long-term fracture healing was assessed in fracture callouses using micro-computerized tomography and histomorphometry analyses.
- For additional details see the "Materials and Methods" section of the study
The team found that the surgery disrupted the blood brain barrier and activated microglia (a first line immune responder present in the inflamed brain), which led to impaired object place and identity discrimination when the mice were subject to the "What-Where-When" and Memory Load Object Discrimination tasks. Both URMC-099 dosing methods prevented the surgery-induced microgliosis (increase in the number of activated microglia) and cognitive impairment without affecting fracture healing.
"A major concern regarding the use of anti-inflammatory drugs for PND is whether they will affect fracture healing. We found that our preventive, time-limited treatment with URMC-099 didn't influence bone healing or long-term bone repair," said Gelbard and Terrando, professor of Neurology, Neuroscience, Microbiology and Immunology, and Pediatrics at URMC and associate professor of Anesthesiology at Duke University Medical Center, respectively. "These findings of improvement in cognition and normal fracture healing provide compelling evidence for the advancement of URMC-099 as a therapeutic option for PND."
"Right now we have nothing to treat this condition," said Mark A. Oldham, M.D., assistant professor in the department of Psychiatry at URMC who treats patients with PND. "We work hard to provide good medical care, including helping people sleep at night and making sure they are walking, eating and drinking, but it isn't clear that these efforts have any meaningful long-term impact."
According to Oldham, recent studies that track patients following an episode of PND show that many of them don't resolve completely, and that they have a new cognitive baseline after delirium.
"It is increasingly an accepted fact that after delirium, people have suffered some kind of neurological insult, which leaves them cognitively or functionally worse off than before the incident," he noted.
Next steps for the research include identifying definitive mechanisms for pain modulation, immune cell trafficking and neuro-immune characterization in PND. Gelbard and Terrando are tackling some of these questions with funds from the National Institutes of Health (RO1 AG057525). The current study was also funded by multiple grants from the NIH (P01MH64570, RO1 MH104147, RO1 AG057525 and F31 MH113504). The University of Rochester has four issued U.S. patents and multiple issued patents in foreign countries covering URMC-099.
New Location for Clinical Trial Support Services
Wednesday, September 4, 2019
The URMC Clinical Materials Services Unit (CMSU) has relocated to a newly renovated space at 150 Metro Park in Rochester. CMSU is a unique academic-based organization that provides consulting and supply chain logistics to small and large multi-center clinical trials.
The CMSU will hold an open house at the new facility on Tuesday, September 10 from 3:00 to 6:00pm.
CMSU was founded in 2008 when clinical researchers at URMC determined the need for a dedicated, on-site facility to manage entire supply chains in support of clinical trials. The CMSU is a core research unit of the Center for Health + Technology (CHeT) which is directed by Ray Dorsey, M.D.
CHeT faculty have been involved in the conduct of clinical research for more than 30 years and have conducted 133 clinical trials, involving 48 different sponsors, 43,000 study participants, and have played a leading role in bringing seven new drugs to market -- five for Parkinson's disease and two in Huntington's disease.
CMSU provides a full array of investigational drug and device packaging, labeling, distribution, and accountability services that support academic medical centers, pharmaceutical and biotech companies, and contract research organizations. CMSU, which is led by executive director Cornelia Kamp, M.B.A, is staffed by 8 dedicated full time employees with more than 150 years of collective pharmaceutical industry experience.
Over the past 11 years CMSU has provided clinical supply services to 60 multi-center clinical trials conducted in the US, Canada, New Zealand and Australia supported with funding from the NINDS, NCCAMS, NICHD, NEI, Michael J. Fox Foundation, DOD, FDA, and numerous pharmaceutical and biotech companies. At any given time, CMSU supports between 15-20 clinical trials.
CMSU also manages the logistical drug supply operations of NeuroNEXT, a NINDS-funded national network of academic medical centers dedicated to accelerating clinical research for neurological disorders. To date, CMSU has been involved in determining the drug supply requirements for 36 of the 67 proposals approved for clinical trials.
The CMSU was previously located in the BioVenture Center in Henrietta. The new 8,800+ square foot facility operates under current Good Manufacturing Practices (cGMP) and is licensed by the New York State Board of Pharmacy. The new location consolidates warehouse, office, and processing space and allows for the more efficient coordination and distribution of research materials.
Mobile Stroke Unit Expands Operations to Monroe County
Wednesday, August 21, 2019
The UR Medicine Mobile Stroke Unit (MSU) is now being dispatched to provide stroke care to patients throughout Monroe County. The MSU had been operating on a pilot basis in the City of Rochester since its launch in October 2018.
The MSU, which is operated in partnership with American Medical Response (AMR) and is the only unit of its kind in upstate New York, serves as an "emergency department on wheels" and brings the medical expertise and technology necessary to diagnose and treat stroke directly to the patient. Immediate care is essential during a stroke, during which millions of brain cells die every minute. However, if caught early, many stroke victims can make a full recovery.
It is estimated that 3,000 people in Monroe County suffer from a stroke every year. Stroke is the fifth leading cause of death and the number one cause of long-term disability in the U.S.
The MSU is equipped with a portable CT scanner that scans the patient's brain to determine the type of stroke they are experiencing. These scans and results from a mobile lab on the unit are transmitted to stroke experts at UR Medicine's Comprehensive Stroke Center at Strong Memorial Hospital, who consult via an on board teleconferencing system with the EMS personnel and determine if treatment -- in the form of the clot busting drug tissue plasminogen activator (tPA) -- can be administered immediately on scene.
"The ability to diagnose and start care in a patient's driveway is a game changer for our region," said Tarun Bhalla, M.D., Ph.D., Chief of Stroke and Cerebrovascular Surgery at the UR Medicine Comprehensive Stroke Center and director of the Mobile Stroke Unit initiative. "We are grateful to our partners in the EMS community for their cooperation in making this lifesaving technology available to stroke patients across Monroe County."
"The sooner patients receive care, the more likely they are to return to their lives," said Curtis Benesch, M.D., M.P.H., Chief of Stroke and Medical Director of the UR Medicine Comprehensive Stroke Center. "The time saved by delivering care directly to a stroke patient on scene can mean the difference between recovery of function or a lifetime of disability."
The MSU is dispatched by the City of Rochester/Monroe County 9-1-1 Emergency Communications Center in coordination with the following EMS agencies:
- Brighton Volunteer Ambulance
- Churchville Fire Department Rescue Squad
- CHS Mobile Integrated Health Care (Chili, Henrietta, Scottsville, Caledonia)
- Gates Volunteer Ambulance
- Greece Volunteer Ambulance
- Hilton Fire Department Ambulance
- Honeoye Falls-Mendon Volunteer Ambulance
- Irondequoit Ambulance
- Monroe Ambulance
- Northeast Quadrant Advanced Life Support
- Penfield Volunteer Emergency Ambulance Service
- Perinton Ambulance
- Pittsford Volunteer Ambulance
- Point Pleasant Fire Department Ambulance
- Rush Fire Department Ambulance
- RIT Ambulance
- Seabreeze Fire Department Ambulance
- Union Hill Volunteer Ambulance
- Webster Emergency Medical Services
"AMR is proud to partner with the University of Rochester and Monroe County to expand the available care options in Monroe County," said Tim Frost, regional director for AMR Western New York. "We are focused on providing the best possible care for the communities we serve, and bringing this new technology to the area is a testament to that."
Read More: Mobile Stroke Unit Expands Operations to Monroe CountyURMC Research Tool Unlocks Natural History of Batten Disease
Wednesday, July 31, 2019
An article appearing in Neurology Today, a publication of the American Academy of Neurology, describes how University of Rochester Medical Center (URMC) researchers have painstakingly compiled decades of patient data and developed a highly sensitive rating scale that has provided a detailed picture of Batten disease. This tool, which was developed 17 years ago, has set a standard for how to conduct natural history research in rare childhood neurodegenerative diseases.
A common challenge in the treatment and study of neurological disorders is that these diseases are often poorly understood. The complex manifestation of these conditions -- in which the appearance, severity, and progression of symptoms can vary widely -- combined with the difficulty in recruiting study participants with rare neurological disorders often conspire to hamper efforts to precisely define the disease. This is a major problem when it comes to clinical trials, where rigorously defined outcome measures are required to determine if an experimental treatment is effective.
CLN3 disease is such an example. The disorder is one of a family of conditions called neuronal ceroid lipofuscinoses (NCL), more commonly referred to as Batten disease, which are characterized by vision loss, movement disorders, seizures, and dementia. It is estimated 2 to 4 out of every 100,000 children in the U.S. have NCL. CLN3 disease, a juvenile onset form of NCL, is the most prevalent form of the disease.
Initiated in 2001 by URMC neurologists Frederick Marshall, M.D. and Jonathan Mink, M.D., the Unified Batten Disease Rating Scale (UBDRS) includes physical, seizure, behavioral, and vision assessments. Over time, the scale has been refined based on clinical observations. To date, University of Rochester Batten Disease researchers have used the UBDRS to perform almost 500 evaluations in more than 200 patients in the U.S. and around the world.
The development of the UBDRS was followed by the creation of a registry of known cases and the formation of the University of Rochester Batten Center in 2005. The center is co-directed by Mink and Erika Augustine, M.D. and includes Heather Adams, Ph.D. and Amy Vierhile, D.N.P on the leadership team and has become a leading center internationally for clinical research on all forms of Batten disease.
Read more about the development of the UBDRS in Neurology Today.
New Grants will Accelerate Clinical Trials in Rare Neurological Disorders
Wednesday, June 26, 2019
Two new grants from the National Institute of Neurological Disorders and Stroke (NINDS) will pave the way for new treatments for neuronal ceroid lipofuscinoses and Charcot Marie Tooth diseases, two groups of rare neurological disorders. The funding, which totals $10 million, will support new research programs led by University of Rochester Medical Center (URMC) neurologists Erika Augustine, M.D., and David Herrmann, M.B.B.Ch., and involve an international team of scientists and clinicians.
The funding comes from the NINDS Clinical Trial Readiness for Rare Neurological and Neuromuscular Diseases program, which was created to support studies that lay the groundwork for the next generation of treatments -- including gene replacement therapies -- currently under development. URMC researchers play leading roles in three of the five NINDS clinical trial readiness programs. URMC neurologist Rabi Tawil, M.D., is a co-director of an existing program that focuses on facioscapulohumeral muscular dystrophy.
"For many neurological diseases, there is a lack of preparedness to run the highest quality clinical trials," said Herrmann. "This includes making sure that you have teams in place and ways to effectively measure the effect of a new drug. And because you're dealing with a rare disease, getting enough patients into a trial is often a challenge."
"As the pipeline of potential new treatments expands, we have to be ready," said Augustine. "This means not just understanding the natural history of these disease, but to have clinical trial tools that are fit for purpose, both to meet regulatory requirements and to measure what is important to patients and families."
The research program led by Augustine will focus on Juvenile neuronal ceroid lipofuscinosis (CLN3 disease) -- the most prevalent form of a family of neurological disorders commonly referred to as Batten diseases. The symptoms of CLN3 disease emerge in early childhood and involve vision loss, seizures, and impaired cognitive and motor function, all of which worsen as the disease progresses and youth typically die of disease complications by their twenties or thirties. There are currently no therapies available to modify the course of the disease.
The new funding will support a partnership between the University of Rochester Batten Center and the University of Hamburg in Germany to validate clinical outcomes and neuroimaging biomarkers that will precisely measure the symptoms and progression of CLN3 Disease and enable researchers to determine if new experimental therapies are effective. This funding builds upon more than 15-years of leading research by the Batten Center, which is directed by Jonathan Mink, M.D., Ph.D., in collaboration with Heather Adams, Ph.D. Frederick Marshall, M.D., Amy Vierhile, P.N.P., and Christopher Beck, Ph.D.
The program headed by Herrmann, who heads the URMC Neuromuscular Disease Program, will focus on Charcot Marie Tooth disease (CMT), a family of rare inherited peripheral neuropathies that is characterized by progressive weakness, imbalance, sensory loss, and gait abnormalities. While physical and occupational therapy, braces and other orthopedic devices, and surgery can help individuals cope with the disabling symptoms of the disease, there is currently no disease modifying treatment for CMT.
The project will involve researchers from URMC, the University of Iowa, the University of Pennsylvania, the University of Sydney in Australia, University College of London, and the C. Besta Neurological Institute in Milan, Italy. The team will be validating a clinical outcomes tool and new imaging technologies that measure the integrity and density of muscle tissue and nerve endings. The goal of the program is to generate a set of biomarkers and patient-centered measures of meaningful functional improvement that can ultimately be used in future clinical trials.
Johns Hopkins School of Medicine 2019 Honors Gretchen Birbeck, MD, MPH, with their Global Achievement Award
Monday, June 10, 2019
Gretchen L. Birbeck, MD, MPH, Professor, Department of Neurology, University of Rochester Medical Center, has dedicated much of her career to improving care for neurological disorders in sub-Saharan Africa. Her work in Zambia initially focused on understanding the burden of epilepsy and barriers to care for patients with epilepsy, and this early work led to studies addressing the pathophysiology and determinants of outcomes of pediatric cerebral malaria in both Malawi and Zambia. She has also contributed to our understanding of neurological complications of HIV and the overall burden of neurological diseases in sub-Saharan Africa.
Dr. Birbeck has worked to improve the neurologic training of healthcare workers and to develop research capacity in both Zambia and Malawi. Moreover, she has been a true pioneer in the field of global neurology as the first to demonstrate how one could have a viable academic neurology career while working in a low-resourced setting. In fact, she has maintained continuous NIH funding for her work in sub-Saharan Africa for the past 16 years. For her work, she has been named Fellow of the American Academy of Neurology, the American Neurologic Association, and the Royal Society of Tropical Medicine & Hygiene; and has received numerous awards. She is a U.S. Paul Rogers Society Ambassador for Global Health Research and was recognized by the International League Against Epilepsy as an Ambassador for Epilepsy.
Her trailblazing work serves as the foundation for the field of global neurology, and she has mentored the majority of neurologists in academic global neurology today. Birbeck's dedication to improving neurological care in sub-Saharan Africa and building the careers of junior African and U.S. neurologists and scientists is unparalleled.
New Gene Therapy Poised to Transform Care for Spinal Muscular Atrophy
Wednesday, June 5, 2019
The University of Rochester Medical Center (URMC) has been tapped as one of the first institutions in the U.S. to offer a new gene replacement therapy to treat spinal muscular atrophy (SMA). The new treatment can be delivered within weeks of birth and clinical trials have shown that it dramatically changes the course of the disease.
"SMA is a devastating disease and, until very recently, diagnosis was tantamount to either a death sentence or a lifetime of severe disability," said URMC neurologist Emma Ciafaloni, M.D., the director of the URMC Pediatric Neuromuscular Medicine Program. "This new therapy, combined with the clinical expertise necessary to treat this complex disease, holds the promise to slow, if not completely halt, the progression of SMA."
Ciafaloni served on a panel overseeing data collection and safety for clinical studies of the new treatment. She is also served as an advisor to Avexis, the company that developed the new gene therapy and was acquired by Novartis in 2018. The treatment is being marketed under the brand name Zolgensma.
The gene therapy, which is administered in the form of a one-time IV infusion, was recently approved by the Food and Drug Administration (FDA) under a "fast track" review process. URMC is one of only 17 medical centers in the U.S., and the only one in New York State, that will initially offer the treatment.
SMA -- a rare hereditary genetic disease that is diagnosed in one out of every 10,000 children born in the U.S. each year -- is caused by a mutation in the survival motor neuron gene (SMN1). This genetic flaw disrupts the production of a protein critical to the function of the nerves that control muscles.
In infants with SMA type 1, the most common and severe form of the disease, symptoms will typically appear within six months as they begin to gradually experience difficulty breathing, swallowing, speaking, and moving. Left untreated, the infant's muscles will progressively deteriorate, eventually leading to paralysis and death, which in most cases occurs within two years. SMA is the number one genetic cause of death in infants.
The new treatment employs a genetically-engineered virus that enters the spinal cord and delivers fully functioning copies of the SMN1 gene directly to the patient's motor neuron cells. These healthy genes rapidly replicate, enhance the cells' protein production, and help re-establish muscle control.
New Multi-Institutional Partnership to Focus on Stroke Rehabilitation
Monday, May 20, 2019
The University of Rochester Medical Center (URMC), Burke Neurological Institute, and Wadsworth Center of the New York State Department of Health (NYSDOH) have been awarded a $5 million grant from the Empire State Development Corporation to speed the development of ground-breaking neurological treatments for those disabled from stroke.
The project is a part of the NeuroCuresNY (NCNY) initiative, a new non-profit formed by the three institutions to accelerate the discovery of novel treatments for chronic neurological impairment and disability. The new state funding will support a two-year pilot study that will be launched in January 2020. This study design will be unique because it will test the efficacy of state-of-the-art robotic-assisted rehabilitation technology combined with drugs to improve the functional recovery of stroke patients.
Neurological conditions such as stroke, traumatic brain injury and spinal cord injury permanently disable more than one million people each year in the U.S., and stroke is the nation's leading cause of disability. Clinical trials for neurological disabilities and impairments are usually passed over because of unclear results, high costs, and challenges in recruiting participants. NCNY will seek to lower the barriers to participation in clinical trials by assisting with travel funding for patients, while providing a supportive and guiding environment for patients and their families.
Clinical and research faculty from URMC Departments of Neurology, Neurosurgery, and Physical Medicine & Rehabilitation will collaborate with the UR Neurorestoration Institute during the pilot study.
Mouse Study: Deep Sleep Helps the Brain Wash Away Toxic Proteins
Friday, March 1, 2019
Deep sleep allows the brain to wash away waste and toxic proteins more efficiently, according to a new mouse study published in the journal Science Advances. The new findings shed light on previous evidence linking Alzheimer's disease with aging and sleep deprivation.
"Sleep is critical to the function of the brain's waste removal system and this study shows that the deeper the sleep, the better," said Maiken Nedergaard, MD, DMSc, co-director of the Center for Translational Neuromedicine at the University of Rochester Medical Center (URMC) and lead author of the study.
"These findings also add to the increasingly clear evidence that quality of sleep or sleep deprivation can predict the onset of Alzheimer's and dementia."
The study suggests that the slow and steady brain and cardiopulmonary activity linked to deep non-REM sleep are optimal for the function of the glymphatic system, the brain's waste removal system. The findings may also explain why some forms of anesthesia can result in cognitive dysfunction in older adults.
Grant Marks Two Decades of NIH Support for Muscular Dystrophy Research
Tuesday, February 26, 2019
Deposits of toxic RNA (red) are seen here inside muscle cell nuclei (blue) from an individual with myotonic dystrophy
The University of Rochester Medical Center (URMC) has received $8 million from the National Institutes of Health (NIH) to support pioneering research on muscular dystrophy. The grant, which is a renewal of URMC's Paul D. Wellstone Muscular Dystrophy Cooperative Research Center, will fund ongoing work to investigate the genetic mechanisms and progression of this complex multi-system disease, research that has led scientists to the threshold of potential new therapies for myotonic dystrophy.
"The mission of the URMC Wellstone Center is to promote research that leads to effective treatments for muscular dystrophy," said Charles Thornton, M.D., a professor in the URMC Department of Neurology and director of the URMC Wellstone Center. "This new funding will enable us to continue a research program that has been forged from a true partnership between bench scientists, clinical researchers, and patients and their families."
URMC is home to one of six NIH-designated Wellstone Centers in the nation. URMC was selected in the first cycle of funding when the program was launched 16 years ago and is the only Wellstone Center that has been continuously funded since the program's inception. With the current award, URMC has received a total of $29.8 million in NIH funding to study the disease since 2003.
The URMC Wellstone Center focuses on myotonic dystrophy, a disease that can be lethal in infants and adults and is characterized by progressive disability. Researchers at URMC have been studying myotonic dystrophy for more than 30 years and their work has transformed our understanding of the biological mechanisms of the disease. The new funding will support a long-standing collaboration between researchers at the University of Rochester and RNA scientists at the University of Florida.
Approximately 40,000 Americans have myotonic dystrophy, which is one of the most common forms of muscular dystrophy. People with the disease have muscle weakness and prolonged muscle tensing (myotonia), which makes it difficult to relax muscles after use. Eventually many patients have difficulty walking, swallowing, and breathing.
Possible Parkinson's 'Pandemic' Looms: Report
Wednesday, February 20, 2019
TUESDAY, Feb. 19, 2019 (HealthDay News) -- The number of people living with Parkinson's disease worldwide could double in the next two decades, experts project.
In a report warning of a possible Parkinson's "pandemic," researchers say the stage is set for cases to surge to 12 million or more by 2040.
What's to blame? In large part, trends that are generally positive: Older age is a major risk factor for Parkinson's, and with life expectancy rising worldwide, more people will develop the disease. At the same time, Parkinson's patients are surviving longer, which drives up the number of people living with the disease at any given time.
Then there's a less expected factor: Declining smoking rates. While the habit has many devastating effects, research suggests it protects against Parkinson's.
Those are obviously trends that no one wants to reverse, said report author Dr. Ray Dorsey.
There are, however, other ways to slow the projected rise in Parkinson's, said Dorsey, a professor of neurology at the University of Rochester Medical Center in New York.
URMC Designated as a Duchenne Care Center
Monday, February 11, 2019
Parent Project Muscular Dystrophy (PPMD), a nonprofit organization dedicated to advancing care and research for patients with Duchenne muscular dystrophy, has named the University of Rochester Medical Center (URMC) a Certified Duchenne Care Center. This program of leading centers, created in 2014 by PPMD, reviews and recognizes clinics nationwide for their outstanding neuromuscular programs.
"Our goal is to make a positive impact on the quality of life of children, adolescents, and adults affected by Duchenne by providing a team of experts in all specialties needed to best care for patients, a friendly and supportive atmosphere, and coordinated care that is highly accessible for families," said Emma Ciafaloni, M.D., the director of the URMC Duchenne Muscular Dystrophy Clinic. "We are honored to be recognized by PPMD as a Certified Duchenne Care Center as we continue to provide the best care and support possible for Duchenne patients and their families."
Study: Neurons in the Brain Work as a Team to Guide Movement of Arms, Hands
Tuesday, December 11, 2018
 The apparent simplicity of picking up a cup of coffee or turning a doorknob belies the complex sequence of calculations and processes that the brain must undergo to identify the location of an item in space, move the arm and hand toward it, and shape the fingers to hold or manipulate the object. New research, published today in the journal Cell Reports, reveals how the nerve cells responsible for motor control modify their activity as we reach and grasp for objects. These findings upend the established understanding of how the brain undertakes this complex task and could have implications for the development of neuro-prosthetics.
The apparent simplicity of picking up a cup of coffee or turning a doorknob belies the complex sequence of calculations and processes that the brain must undergo to identify the location of an item in space, move the arm and hand toward it, and shape the fingers to hold or manipulate the object. New research, published today in the journal Cell Reports, reveals how the nerve cells responsible for motor control modify their activity as we reach and grasp for objects. These findings upend the established understanding of how the brain undertakes this complex task and could have implications for the development of neuro-prosthetics.
"This study shows that activity patterns in populations of neurons shift progressively during the course of a single movement," said Marc Schieber, M.D., Ph.D., a professor in the University of Rochester Medical Center (URMC) Department of Neurology and the Del Monte Institute for Neuroscience and a co-author of the study. "Interpreting these shifts in activity that allow groups of neurons to work together to perform distinctive and precise movements is the first step in understanding how to harness this information for potential new therapies."
Kelly Family Pumped About GCH Milestone
Tuesday, November 13, 2018

UR Medicine's Golisano Children's Hospital has been designated an official Leukodystrophy Care Network Center by the Hunter's Hope Foundation.
Hunter's Hope Foundation co-founders Jim and Jill Kelly announced the designation on Monday, making Rochester just the seventh Leukodystrophy Care Network Center in the nation and the first in New York State.
Led by Robert Thompson-Stone, M.D., assistant professor of Pediatrics and Child Neurology, the UR LCC will work across disciplines to provide the best care to patients and families. Thompson-Stone and others will also participate in regular meetings with fellow Leukodystrophy Care Network clinicians throughout the United States, allowing providers to share best care practices and discuss new and ongoing research into leukodystrophies.
"Our Child Neurology team works across disciplines to put the needs of our patients and families above all else, and this designation really validates the work we've done so far," said Thompson-Stone. "Going forward, we are eager to work collaboratively with this national network of talented physicians and care providers on both clinical care and research efforts."
One in 7,000 children are born with a leukodystrophy, a group of rare, progressive genetic diseases that affect the brain and spinal cord. Jim and Jill Kelly's son, Hunter, was diagnosed in 1997.
"Jill and I were told to go home, make Hunter comfortable and that he wouldn't live to see his second birthday. Hunter lived to be eight and a half years-old," shared Jim Kelly, Hunter's Hope Co-Founder and Pro Football Hall of Fame Member. "We believe he lived so much longer than expected because of the good Lord, and because we treated Hunter as though he was living, not dying. Twenty-one years later, families are being told the same thing that Jill and I were, and that has to change."
The Hunter's Hope Foundation established the Leukodystrophy Care Network in 2015 with the goal of improving the health and quality of life of individuals affected by leukodystrophies. Through the designation, the foundation will support a patient care coordinator in Rochester who will help families navigate their treatment
New Research Initiative to Focus on Cerebrovascular Diseases
Monday, October 29, 2018
A multidisciplinary group of clinical and bench researchers has been formed at the University of Rochester Medical Center (URMC) to study cerebrovascular disease. The Cerebrovascular and Neurocognitive Research Group (CNRG), which consists of faculty from Neurology, Neurosurgery, Electrical and Computer Engineering, Microbiology and Immunology, and Vascular Biology will leverage advanced brain imaging technologies to investigate a number of diseases, including stroke, cerebral small vessel disease (CSVD), and vascular dementia.
UR Named National Center of Excellence for Parkinson’s Research
Wednesday, October 3, 2018
The University of Rochester has been selected as a Morris K. Udall Center of Excellence in Parkinson's Disease Research by the National Institute of Neurological Disorders and Stroke (NINDS). The new $9.2 million award brings together researchers from industry and multiple academic institutions to focus on the development of digital tools to enhance understanding of the disease, engage broad populations in research, and accelerate the development of new treatments for Parkinson's disease.
Welcome Resident Applicants
Monday, October 1, 2018

The Department of Neurology would like to welcome residency applicants, interviewing on Monday, January 14th. A wine and cheese reception for the applicants will be held from 4:00 - 4:30 PM in the Garvey Room. All Faculty & Residents are invited to attend.
Adult Neurology Applicants
Nicole Baldwin -- University of Minnesota
Cara Doyle -- Campbell University School of Osteopathic Medicine
Daniel Orme -- University of Utah
Allan Phan -- University of Wisconsin
Noellie Rivera-Torres -- Universidad Central del Caribe, Puerto Rico
Janani Sadasivan -- Michigan State University
UR Medicine Unveils Upstate New York’s First Mobile Stroke Unit
Thursday, September 27, 2018
Next month, UR Medicine will begin operation of a Mobile Stroke Unit (MSU), a high-tech 'emergency room on wheels' that is designed to provide life-saving care to stroke victims. The $1 million unit will be operated in partnership with AMR as a community resource and represents a significant step forward for stroke care in the Rochester region.
While the MSU resembles an ambulance on the outside, inside it contains highly specialized staff, equipment, and medications used to diagnose and treat strokes. The unit is equipped with a portable CT scanner that is capable of imaging the patient's brain to detect the type of stroke they are experiencing. The scans and results from a mobile lab on the unit are wirelessly transmitted to UR Medicine stroke specialists at Strong Memorial Hospital, who will consult with the on board EMS staff via telemedicine and decide if they can begin treatment immediately on scene.
If it is determined that the patient is experiencing an ischemic stroke -- which account for approximately 90 percent of all strokes -- the MSU team can administer the drug tissue plasminogen activator (tPA) to attempt to break up the clot in the patient's brain. While en route to the hospital, UR Medicine specialists will continue to remotely monitor and assess the patient's symptoms.
"The UR Medicine Mobile Stroke Unit essentially brings the hospital to the patient," said neurosurgeon Tarun Bhalla, M.D., Ph.D., with the UR Medicine Comprehensive Stroke Center. "This unit will improve care and outcomes by shortening the gap between diagnosis and treatment and enable us to initiate care before the patient reaches the hospital."
It is estimated that 3,000 people in Monroe County suffer from a stroke every year. Stroke is the fifth leading cause of death and the number one cause of long-term disability in the U.S. However, if caught early, many stroke victims can make a full recovery.
"Ten years ago we realized there was an epidemic of stroke in our community which resulted in tremendous human suffering and health care costs," said Web Pilcher, M.D., Ph.D., chair of the UR Medicine Department of Neurosurgery. "We decided to embark on a long-term plan to provide the best stroke care in upstate New York. The Mobile Stroke Unit represents the next evolution in that effort and places Rochester among an elite list of communities with this cutting-edge technology."

The current best treatment for stroke is tPA. But in order to work properly, the drug must be given within four and half hours of the first stroke symptoms. Depending upon the circumstances, doctors may also elect to perform a minimally invasive endovascular surgical procedure that involves threading a catheter through the blood vessels and physically removing the obstruction in the brain. The capabilities provided by the MSU to diagnose, start treatment, and prepare hospital staff to receive the patient before they arrive at the emergency department will save lives and improve chances of recovery.
"In stroke care, time equals brain," said neurologist Curtis Benesch, M.D., M.P.H., with the UR Medicine Comprehensive Stroke Center. "The approximately 30 minutes that could be saved by the Mobile Stroke Unit by starting treatment before a stroke patient reaches the hospital could mean the difference between the recovery of function or a lifetime of impairment."
"Patients who receive tPA sooner are more likely to go home and retain the ability to walk and care for themselves," said Bob Holloway, M.D., M.P.H., chair of the UR Medicine Department of Neurology. "The Mobile Stroke Unit will improve outcomes for stroke victims in our community and, because people with less disability use fewer health care resources, lower costs in the long term."
The unit is owned by UR Medicine and will be operated by AMR. The MSU will be staffed by a UR Medicine nurse trained in stroke care and a CT technician, an AMR paramedic and emergency medical technician, and remotely by a stroke specialist at UR Medicine.
The construction and operating costs of the unit, which was custom built by Frazer Ltd. in Houston, are being funded by UR Medicine and philanthropy, including a lead gift from Elena Prokupets and support from the Del Monte family and other donors in the Rochester community.
"We are extremely grateful to Elena for her gift to the School of Medicine and Dentistry, which has made it possible to bring this life saving technology to Rochester," said Mark Taubman, M.D., CEO of the University of Rochester Medical Center. "Her generosity, along with the support of many others, has provided us the resources to invest in the infrastructure, technology, and clinical talent necessary to provide the most advanced stroke care to our community."
The MSU is part of a broader UR Medicine initiative to bring state-of-the-art stroke care to the region. This includes Strong Memorial Hospital's designation as the region's only Comprehensive Stroke Center by the Joint Commission, a certification that indicates that the hospital either meets or exceeds the highest standards of care required to provide timely, advanced, and coordinated care to patients with cerebrovascular disease, and the Neuromedicine Intensive Care Unit, a 12-bed ICU that provides care to critically ill patients with complex neurological life threating illnesses such as stroke. UR Medicine stroke specialists also provide 24/7 consultation services for emergency department personnel in several hospitals in the region via telemedicine.
Eight years ago, UR Medicine, in partnership with the Greater Rochester Health Foundation, created the Stroke Treatment Alliance of Rochester/New York (STAR-NY), to educate medical professionals and the broader community about stroke recognition and prevention.
Common Painkiller Not Effective for Traumatic Nerve Injury
Monday, September 24, 2018
A new study out today in the Journal of Neurology finds that pregabalin is not effective in controlling the chronic pain that sometimes develops following traumatic nerve injury. The results of the international study, which was driven by an effort to identify effective non-opioid pain medications, did show potential in relieving in pain that sometimes lingers after surgery.
"The unrelenting burning or stabbing symptoms due to nerve trauma are a leading reason why people seek treatment for chronic pain after a fall, car accident, or surgery," said John Markman, M.D., director of the Translational Pain Research Program in the University of Rochester Department of Neurosurgery and lead author of the study. "While these finding show that pregabalin is not effective in controlling the long-term pain for traumatic injury, it may provide relief for patients experience post-surgical pain."
Pregabalin, which is marketed by Pfizer under the name Lyrica, is approved to treat chronic pain associated with shingles, spinal cord injury, fibromyalgia, and diabetic peripheral neuropathy. However, it is also commonly prescribed as an "off label" treatment for chronic nerve injury syndromes that occur after motor vehicle accidents, falls, sports injuries, knee or hip replacement and surgeries such as hernia repair or mastectomy.
A previous eight-week study had shown that pregabalin reduced pain intensity better than placebo in these chronic, post-traumatic pain syndromes. These results led many doctors to prescribe this medication for long-term pain that does not resolve as expected.
Chronic postsurgical pain syndromes occur in approximately one or two out of every 10 surgical patients and the levels rated as intolerable after roughly one or two in every 100 operations. With 55 million surgeries performed in the U.S. every year, severe chronic pain impacts more than a million new people annually. Roughly one third of these patients are believed to have neuropathic pain or ongoing pain related to nerve injury.
These rates vary widely by type of surgery. The risks factors and underlying mechanisms of this type of chronic pain are not well understood, but because the types of symptoms patients describe like "burning", "unpleasant tingling," or "numbness" resemble other nerve pain syndromes like shingles pain. As a result, physicians trying to find useful non-opioid pain relievers have often turned to prescribing gabapentin or pregabalin.
The current study was conducted in 101 centers in in North America, Europe, Africa, and Asia and followed 539 individuals for three months. Study participants were randomized into two groups who either prescribed pregabalin or a placebo.
The study found that pregabalin was not effective in controlling pain for individuals with traumatic nerve injury. A retrospective analysis of a subgroup of study of participants, whose nerve pain was attributed to surgery, showed that the drug did provide better pain relief than placebo at 3 months.
"The possibility that there was pain relief for those patients who had a hernia repair, or breast surgery for cancer, or a joint replacement lays the groundwork for future studies in these post-surgical syndromes where there is so much need for non-opioid treatments," said Markman.
One major challenge is that different biological changes in the nerves and other tissues that cause pain to persist after healing from trauma vary from one patient to the next. Currently, there is no diagnostic method that allows doctors to readily identify the patients whose pain will respond to a particular type of pain treatment.
Despite employing new strategies to reduce placebo effects, the patients receiving placebo also had a steady lowering of their pain over the course of the study. The pattern of these placebo effects in longer studies has proved to be a major challenge to the development of new pain medications.
"Given the rising rates of surgery and shrinking reliance on opioids, it is critical that we understand how to study new drugs that work differently in patients like the ones included in this study," Markman added.
Additional co-authors of the study include Malca Resnick, Scott Greenberg, Ruoyong Yang, Joseph Scavocne, Ed Whalen, Gabriela Gregorian, Bruce Parsons, and Lloyd Knapp with Pfizer and Nathaniel Katz with Analgesic Solutions. Pfizer funded the trial, and was involved in its design as well as the data collection and analysis. The company also paid for medical writing assistance and editorial support in preparing the article for the journal. Markman has received consulting fees and research funding support from Pfizer.
UR Achieves Lewy Body Disorder Association Center of Excellence Status
Monday, September 17, 2018
The University of Rochester movements disorders division has been designated as a lead body disorder Association research center of excellence. This designation is obtained at the understanding of the disorder, educating patients and caregivers, and investigating possible research activities specifically aimed at this difficult disease. While many people are always involved in obtaining such a designation, special kudos go to Dr. Katie Amodeo who has been instrumental in our success with this endeavor and will continue to play a key role in developing a successful UR program focused on the rapidly growing field of neurodegenerative diseases characterized by Parkinsonism and Dementia.
Drug Shows Promise in Slowing Multiple Sclerosis
Wednesday, September 5, 2018
Research appearing in the New England Journal of Medicine could herald a new treatment approach for individuals with multiple sclerosis (MS) if confirmed in future studies. The results of a clinical trial, which involved researchers from the University of Rochester Medical Center (URMC), showed that the drug ibudilast slowed the brain shrinkage associated with progressive forms of the disease.
"These results indicate that ibudilast may be effective in protecting the central nervous system and slowing the damage to the brain that is caused by MS," said URMC neurologist Andrew Goodman, M.D., a co-author of the study who served on the national steering committee for the Phase II clinical trial, dubbed SPRINT-MS. "While more clinical research is necessary, the trial's results are encouraging and point towards a potential new type of therapy to help people with progressive MS."
MS is a neurological disorder in which the body's own immune system attacks myelin, the fatty tissue that insulates the nerve fibers in the brain and spinal cord. These attacks are caused by inflammation which damages myelin, disrupting communication between nerve cells and leading to cognitive impairment, muscle weakness, and problems with movement, balance, sensation, and vision. MS usually presents with a relapsing-remitting course, in which symptoms occur then disappear for weeks or months and then may reappear, or primary and secondary progressive courses, which are marked by a gradual decline in function.
Richard Barbano Co-Authors New Guideline for Managing Consciousness Disorders
Thursday, August 16, 2018
A new practice guideline update for the diagnosis and ongoing medical and rehabilitative care of individuals in a vegetative or minimally conscious state has a result of a brain injury have been published by the American Academy of Neurology, the American Congress of Rehabilitation Medicine, and the National Institute on Disability, Independent Living, and Rehabilitation Research.
URMC neurologist Richard Barbano, M.D., Ph.D., was part of a team of physicians and researchers who prepared the new guideline, which appears in the journal Neurology.
The experts carefully reviewed all of the available scientific studies on diagnosing, predicting health outcomes, and caring for people with disorder of consciousness, focusing on evidence for people with prolonged disorders of consciousness -- those cases lasting 28 days or longer.
The guideline recommends that a clinician trained in the management of disorder of consciousness, such as a neurologist or brain injury rehabilitation specialists, should do a careful evaluation and the evaluation should be repeated several times early in recovery.
Additional findings include:
- The outcomes for patients with prolonged disorder of consciousness differ greatly. It is estimated that one in five people with severe brain injury from trauma will recover to the point where they can live at home and care for themselves without assistance.
- There is moderate evidence that patients with a brain injury from trauma will fare better in terms of recovery than a person with a brain injury from another cause.
- Very few treatments for disorder of consciousness have been carefully studied. However, moderate evidence shows that the drug amantadine can hasten recovery in patients with disorder of consciousness after a traumatic brain injury when used within one to four months after the injury.
Ralph Jozefowicz Honored for Mentoring Next Generation of Leaders in Neurology
Tuesday, August 14, 2018
URMC neurologist Ralph Jozefowicz, M.D., has been awarded the American Academy of Neurology's (AAN) Leading in Excellence through Mentorship award. He received the recognition at the AAN's 2018 annual meeting.
Jozefowicz, a professor of Neurology and Medicine, is a nationally recognized leader and innovator in neurologic education and has received numerous awards and accolades from AAN, the American Neurological Association, the Fulbright Program, the Association of American Medical Colleges, and Jagiellonian University in Poland for his work in the field.
He currently serves as director for the second year medical student "Mind, Brain and Behavior" course and co-director of the third year Neurology Clerkship. He is also the Neurology Residency Program Director at the URMC.
You can read more about the award and perspectives from colleagues he has mentored over the years in Neurology Today.
NIH Extends URMC’s Role in Network to Advance Neurological Care
Thursday, July 26, 2018
National Institute of Neurological Disorders and Stroke (NINDS) has extended the University of Rochester Medical Center's (URMC) membership in the Network for Excellence in Neuroscience Clinical Trials, or NeuroNEXT, which was created to accelerate clinical research involving new treatments for neurological disorders. The $1.5 million grant will provide patients in the region access to cutting-edge experimental therapies and continue the Medical Center's key role in helping bring new drugs to market.
"Neurological diseases are some of the most challenging in all of medicine and the process of translating promising discoveries into new treatments requires building partnerships across many institutions in order to create the infrastructure necessary to recruit patients and run multi-site clinical trials," said Robert Holloway, M.D., M.P.H., chair of the URMC Department of Neurology and principal investigator of the URMC NeuroNEXT site. "The Medical Center has a long history in the field of experimental therapeutics and we are proud to be a part of NeuroNEXT and to support efforts that will make clinical research better, faster, and more efficient in the quest to aid patients and families affected by neurological disease."
In 2011, URMC was one of the original 25 institutions selected to participate in NeuroNEXT. The network was created to streamline the operations of neuroscience clinical trials and help increase the number of new treatments that get into clinical practice. The program is designed to encourage collaborations between academic centers, disease foundations, and industry.
Over the last five years, URMC has been involved in NeuroNEXT studies involving the testing of new drugs for myasthenia gravis, multiple sclerosis, Huntington's disease, stroke, brain cancer, and neuropathy. "We could not have accomplished this without the phenomenal talent and dedication of our faculty, study coordinators, and research teams." said Erika Augustine, M.D., M.S., co-Investigator on the grant.
"One of the advantages of NeuroNEXT, and something that makes it unique, is the network's ability to quickly mobilize a group of specialists from a certain disease area to initiate a clinical study when opportunities emerge for trials," said Robin Conwit, M.D., program director at NINDS. "The structure of NeuroNEXT, with its broad focus across neuroscience clinical studies, has the potential to reach many individuals who are affected by brain disorders."
The Medical Center's site -- dubbed UR NEXT -- has made significant contributions to the success and vitality of the network. URMC is the dominant provider of comprehensive neurological care in upstate New York with growing referral networks that have a regional, national, and international reach. This breadth of geographic reach and specialization of services has resulted in the Medical Center being one of the network's leading performers in terms of clinical trial recruitment and performance.
The Medical Center is also home to the Experimental Therapeutics in Neurological Disease post-doctoral training program now entering its 28th year of continuous funding from the National Institutes of Health, and the Center for Health + Technology (CHeT), a unique academic-research organization with decades of experience in development, management, and operation of multi-site clinical trials.
"The complexity of neurological diseases and the ever evolving nature of scientific innovation in this field mean that we must look always to the future and build the teams that turn new discoveries into new ways to diagnose, treat, and prevent these diseases," said Jonathan Mink, M.D., Ph.D., co-investigator on the grant who is leading Rochester's training of its investigators. "The UR NEXT grant will help us train the next generation of experts in leading and conducting multi-center clinical trials,"
In addition to URMC's role as a NeuroNEXT site, the Medical Center has two additional key roles supporting the national network. The URMC Clinical Materials Services Unit -- part of CHeT -- provides logistical support and drug supply distribution services for NeuroNEXT clinical trials and UR Labs provides central laboratory services for the network.
Announcing the formation of a combined Pediatric and Adult Neurofibromatosis Clinic
Friday, July 13, 2018
We are pleased to announce the formation of a combined pediatric and adult Neurofibromatosis clinic. This clinic will be held every four months, and will offer families the ability to be seen on the same day by clinicians expert in neurofibromatosis (NF). Our clinic is headed by Dr. Alex Paciorkowski, who is trained in both Neurology and Genetics. He has a particular interest in neuro-developmental disorders, and is an excellent resource particularly with challenging genetics cases. Dr. Marina Connolly, a child neurologist with special interest and expertise in pain, and headaches, which are common to our patients, will see pediatric NF patients. Dr. Joy Burke is the adult neuro-oncologist who will be joining us, with expertise in treating tumors of the nervous system including brain, spine, and nerves.
Patients with neurofibromatosis may be affected by these problems, and may also have other neurological problems such as migraines, nerve pain, or cognitive function issues which Dr. Burke can address. Dr. Bo Lee, our neuro-genetics fellow will also be involved in patient care, learning about this complex but relatively common neurologic disease. Carolyn Dickinson is the pediatric nurse practitioner on the team, and has been working with children with neurofibromatosis for many years. Finally, Kelly Minks, CGC MS, is our genetic counselor, and assists our team with genetic testing issues.
As neurofibromatosis may affect various organ systems a multidisciplinary clinic allows patients to coordinate appointments with various other specialties, and minimize travel. This combined clinic will also allow our specialists to discuss cases, ease the transition for adolescent and young adults, and facilitate research efforts.
NN108 Topiramate as a disease modifying therapy for Cryptogenic Sensory Peripheral Neuropathy (CSPN)
Thursday, July 12, 2018

The University of Rochester Medical Center is currently looking for people with Cryptogenic Sensory Peripheral Neuropathy for a research study conducted by the Network for Excellence in Neuroscience Clinical Trials (NeuroNEXT).
The purpose of the research study is to learn if the drug topiramate slows the progression of Cryptogenic Sensory Peripheral Neuropathy (CSPN), also known as "idiopathic neuropathy" or neuropathy of an unknown cause, and improves quality of life. As part of this study, we will use a number of assessments and questionnaires to determine iftopiramate improves symptoms of CSPN. There is a one in two (or 50%) chance of receiving the study drug or placebo pill.
Participants must be between 18-75 years of age to be in the study, have a diagnosis of CSPN or idiopathic neuropathy, have signs of metabolic disease including abdominal obesity, pre-diabetes, high blood pressure or abnormal cholesterol/lipids, and no history of prior therapy with topiramate.
This study is actively enrolling participants. To learn more information, please visit ClinicalTrials.gov, identifier number: NCT02878798. If you are interested in participating, contact Janet Sowden at the University of Rochester Medical Center by phone at (585) 275-1267 or email at janet_sowden@urmc.rochester.edu.
AHA Grants Will Accelerate Search for New Stroke Therapies
Wednesday, June 27, 2018
A series of awards from the American Heart Association (AHA) to a team of researchers at the University of Rochester Medical Center (URMC) will focus on the development of new treatments to thwart the damage in the brain caused by stroke.
One of the research projects brings together experts in stroke, cardiovascular biology, platelet biology, and peptide chemistry. Marc Halterman, M.D., Ph.D., with the URMC Center for Neurotherapeutics Discovery, Scott Cameron, M.D., Ph.D., and Craig Morrell, D.V.M., Ph.D., with the URMC Aab Cardiovascular Research Institute, and Bradley Nilsson, Ph.D., with the University of Rochester Department of Chemistry will focus on the role that platelets play in acute brain injury and inflammation during stroke.
Platelets serve an important role in protecting against blood loss and repairing injured blood vessels. However, during a stroke the inflammatory properties of platelets can interfere with the restoration of blood flow once the clot in the brain is removed, particularly in micro-vessels, which can lead to permanent damage of brain tissue.
The research team will build synthetic peptides that activate platelets to study the phenomenon -- which is called no-reflow -- in an effort to identify specific switches within platelets that can be turned off and limit the cells' inflammatory functions without blocking their ability to prevent bleeding.
Two AHA pre-doctoral fellowship awards Kathleen Gates and Jonathan Bartko in Halterman's lab will support research that examines the link between an immune system response triggered by stroke in the lungs that can exacerbate damage in the brain and investigate the cellular mechanisms that determine whether or not brain cells die following stroke.
A final AHA award to the Halterman lab will seek to identify new drug targets by focusing on specific proteins activated during stroke that are suspected to play an important role in determining the survival of neurons.
Collectively, the AHA Collaborative Sciences Award, Pre-Doctoral, and Innovation awards represent $1.09 million in funding.
Dr. Nimish Mohile New Role as Associate Chair of Faculty Development
Tuesday, June 26, 2018

In this role, Nimish will work with me to lead our efforts to support faculty and residents in developing their
careers and enhancing their contributions to the department, the medical center and the field of neurology. To
achieve these goals, Nimish will collaborate with the Associate Chairs of the Department and various Associate Deans
of the Medical School [Faculty Development (Janine Shapiro), Academic Affairs (Jeff Lyness) and Inclusion and
Diversity (Linda Chaudron)].
As a Department, we seek to provide an open, warm and nurturing environment to enable and support our amazing
faculty, residents and staff every day. Nimish has bold initiatives to create supportive structures for career
growth and promotion, in addition to leading the Department's diversity initiatives. He will also
participate as a member of the Department's Promotion and Tenure Committee.
Nimish joined the Department in 2007, after completing his neurology training at Northwestern University (2004) and
his neuro-oncology training at Memorial Sloan-Kettering (2007). Nimish has created a vibrant, inclusive and
forward thinking Division of Neuro-oncology, which excels in all of its missions. The clinical program now
sees more than 100 brain tumor patients each year, he has been the PI for over 20 brain tumor clinical trials, and
he Director for the UCNS Neuro-Oncology Fellowship and the Neurology Resident Mentoring Program. The program
is simply flourishing under his leadership. While he will continue to lead the Neuro-Oncology Division,
he is setting his sights higher however, as he takes on new leadership roles within the Department and nationally
through the American Academy of Neurology.
Please join us in congratulating Nimish!
UR Medicine Recognized for Excellence in Stroke Care
Monday, June 11, 2018
The American Heart Association/American Stroke Association (AHA/ASA) has once again honored the UR Medicine Strong Memorial Hospital for having achieved the highest standard of care for stroke. This award identifies hospitals that provide care that can speed the recovery and reduce death and disability for stroke patients.
Strong Memorial Hospital has received the 2018 AHA/ASA Get With The Guidelines program's Stroke Gold Plus Quality Achievement Award. The hospital was also recognized for the Target: Stroke Honor Role Elite Plus designation, which identifies hospitals that have consistently and successfully reduced door-to-needle time -- the window of time between a stroke victim's arrival at the hospital, the diagnosis of an acute ischemic stroke, and the administration of the clot-busting drug tPA. If given intravenously in the first four and a half hours after the start of stroke symptoms, tPA has been shown to significantly reduce the effects of stroke and lessen the chance of permanent disability.
Wilmot announces new Pilot Award recipients
Monday, April 30, 2018
Wilmot's competitive seed-grant program aims to fund research projects that will generate preliminary data
necessary to potentially apply for federal funding in the future. Thanks to financial support from two community
organizations -- Adding Candles for a Cure and the Edelman Gardner Cancer Research Foundation -- four
projects have received funding that started Jan. 1.
Mark Noble, Ph.D., Professor in the
departments of Biomedical Genetics and Neuroscience, received a $50,000 grant for his project titled, "A
biomarker for a novel glioblastoma (GBM) vulnerability." The co-investigators for this project are Kevin Walter, M.D.,
Mahlon Johnson, M.D.,
Ph.D., Nimish
Mohile, M.D., and Peggy Auinger, M.S.
Bradford Mahon, Ph.D., Assistant Professor in the Departments of Neurology and Neurosurgery, received a $50,000 grant
for his project seeking to demonstrate feasibility and preliminary efficacy of advanced MRI mapping in improving outcome
in patients with glioblastoma. Kevin Walter, M.D., is
the co-investigator for this project.
Congratulations to all Wilmot pilot grant recipients.
Bogachan Sahin, M.D., Ph.D., Named Highland Hospital Chief of Neurology
Monday, April 23, 2018
Dr. Sahin has been an Assistant Professor of Neurology
at the University of Rochester’s School of Medicine and Dentistry since 2013. He earned his undergraduate degree in molecular biology at Princeton University and his M.D. and Ph.D. in Neuroscience at the University of Texas Southwestern Medical Center. Dr. Sahin completed his residency in neurology and fellowship in vascular neurology at Johns Hopkins University. In 2015, he became the Director of the Vascular Neurology Fellowship Program at the University of Rochester Medical Center and has transformed the fellowship. In 2017, there were 76 Vascular Neurology Fellowship Programs across the United States and only 36 of them were filled. Under Dr. Sahin’s leadership, the University of Rochester’s program has filled for three consecutive years and counting.
“Dr. Sahin is an outstanding clinical neurologist and a passionate educator. We look forward to Dr. Sahin bringing the same positive leadership approach to Highland that he’s brought to the Vascular Neurology Fellowship Program as we continue to integrate and expand our acute care service,” said Robert G. Holloway Jr., M.D., M.P.H., Professor and Chair of the Department of Neurology at the University of Rochester Medical Center.
“Highland Hospital is a New York State Designated Primary Stroke Center and an integral part of our stroke care network in UR Medicine. As a board-certified Vascular Neurologist, Dr. Sahin will also serve as the Stroke Center Director, ensuring Highland Hospital maintains its vital role in providing excellent stroke care to our community,” said Curtis Benesch, M.D., M.P.H., Professor of Neurology and Neurosurgery and Medical Director, URMC Comprehensive Stroke Center.
Dr. Sahin follows Adam Kelly, M.D., who served as Highland Hospital’s Chief of Neurology for almost six years.
Read More: Bogachan Sahin, M.D., Ph.D., Named Highland Hospital Chief of NeurologyNational Initiative Focuses on New Treatments for Lewy Body Dementia
Wednesday, April 18, 2018
The University of Rochester Medical Center (URMC) has been selected to participate in a national network created to develop new ways to diagnose and treat Lewy Body Dementia (LBD). The new initiative, which is being organized by the Lewy Body Dementia Association, will seek to raise awareness and advance research for this complex disorder.
"Lewy Body Dementia is a challenging, multifaceted disease and research to find new diagnostic tools and treatments is still in its infancy," said URMC neurologist Irene Richard, M.D., who will serve as director of the URMC Lewy Body Dementia Association Research Center of Excellence. "This new network of will create an infrastructure of clinician researchers who understand the disease, are able to identify patients to participate in research, and have experience participating in multi-site clinical trials."
LBD is a progressive brain disorder marked by abnormal protein deposits -- called Lewy Bodies -- in areas of the brain important for behavior, cognition, and motor control. This complex disease gives rise to a range of symptoms, including cognitive impairment, sleep disturbances, hallucinations, difficulty with blood pressure regulation, and problems with movement and balance. Individuals with the disease will often experience marked fluctuations in their levels of alertness and clarity of thought.
Robert Holloway & Benjamin George Study Regional Stroke Care
Monday, April 16, 2018
New research shows that stroke patients are increasingly being transferred out of smaller community and rural hospitals and sent to larger medical centers for their care and rehabilitation. While this is a positive sign for patients who need more advanced treatments, the trend has drawbacks in terms of cost and points to the need to improve the coordination of care between hospitals.
“The underlying goal of stroke care is to get the right person to the right hospital at the right time,” said University of Rochester Medical Center (URMC) neurologist Benjamin George, M.D., M.P.H., a co-author of the study which appears this month in the journal Neurology. “The findings of this study show that in recent years community-based hospitals are erring on the side of caution and transferring more patients from their emergency departments to larger hospitals. Given the high cost and burden associated with these transfers, striking a balance between cost and need is essential.”
Telehealth, Exercise the Focus of World Parkinson’s Disease Day
Tuesday, April 10, 2018
The University of Rochester Medical Center (URMC) is helping lead two advocacy efforts to increase awareness of the value of telehealth for individuals with Parkinson's. These activities coincide with World Parkinson's Disease Day on April 11.
"The prevalence of Parkinson's disease is increasing and the number of people with the disease is expected to more than double in the next 20 years," said neurologist Ray Dorsey, M.D., director of the URMC Center for Health + Technology (CHeT). "Telemedicine, along with other technologies, will be key to meeting this growing demand and will serve to expand access to quality care, help reduce the burden of caregivers, and potentially lower costs."
CHeT is working with the Parkinson's Foundation to advocate for telehealth by encouraging all of the Foundation's 18 Centers of Excellence to provide at least one telemedicine visit on April 11. Dorsey has undertaken several studies over the last decade to demonstrate the feasibility and effectiveness of connecting Parkinson's patients with specialists using telemedicine. Results of a recent study funded by the Patient-Centered Outcomes Research Institute demonstrated that telemedicine can successfully deliver quality care.
In addition, CHeT has partnered with Burn Along -- an online video fitness and wellness platform that offers hundreds of classes at all fitness levels -- in inviting individuals with Parkinson's disease, caregivers, family members, and advocates to participate in free classes to raise awareness of the importance of exercising for Parkinson disease. Studies have shown that exercise can help keep the symptoms of Parkinson's at bay and may even slow the progression of the disease.
Burn Along has joined with Dance for PD -- a Brooklyn-based company that has created dance classes for people with Parkinson's -- to produce videos for distribution on their website. Individuals who sign up for the free classes with Burn Along on April 11 will have access to all of the site's video content for the entire month of April.
For more information or to sign up for free fitness classes for the month of April, visit: http://fit.burnalong.com/world-parkinson-day/
Mobile Apps Could Hold Key to Parkinson’s Research, Care
Monday, March 26, 2018
By Mark Michaud
A new study out today in the journal JAMA Neurology shows that smartphone software and technology can accurately track the severity of the symptoms of Parkinson's disease. The findings could provide researchers and clinicians with a new tool to both develop new drugs and better treat this challenging disease.
"This study demonstrates that we can create both an objective measure of the progression of Parkinson's and one that provides a richer picture of the daily lived experience of the disease," said University of Rochester Medical Center (URMC) neurologist Ray Dorsey, M.D., a co-author of the study.
One of the difficulties in managing Parkinson's is that symptoms of the disease can fluctuate widely on a daily basis. This makes the process of tracking the progression of the disease and adjusting treatment a challenge for physicians who may only get a snapshot of a patient's condition once every several months when they visit the clinic. This variation also limits the insight that researchers can gather on the effectiveness of experimental treatments.
The new study, which was led by Suchi Saria, Ph.D., an assistant professor of Computer Science at Johns Hopkins University, harnesses the capabilities of technology that already resides in most of our pockets all day, every day.
Researchers recruited 129 individuals who remotely completed a series of tasks on a smartphone application. The Android app called HopkinsPD, which was originally developed by Max Little, Ph.D., an associate professor of Mathematics at Aston University in the U.K., consists of a series of tasks which measure voice fluctuations, the speed of finger tapping, walking speed, and balance.
The Android app is a predecessor to the mPower iPhone app which was developed by Little, Dorsey, and Sage Bionetworks and has been download more than 15,000 times from Apple's App Store since its introduction in 2015.
As a part of the study, the researchers also conducted in-person visits with 50 individuals with Parkinson's disease and controls in the clinic at URMC. Participants were asked to complete the tasks on the app and were also seen by a neurologist and scored using a standard clinical evaluation tool for the disease. This aspect of the study was overseen by URMC's Center for Health + Technology.
John Markman Elected to American Pain Society Board
Friday, March 16, 2018

John Markman, M.D.
The American Pain Society is the nation's leading organization of scientists, physicians, and allied professionals focused on increasing knowledge of pain and transforming clinical practice and policy to reduce pain-related suffering. Markman founded and directs the University's Neuromedicine Pain Management Center and Translational Pain Research Program. Together these programs were previously recognized as a Center of Excellence by the American Pain Society.
Congratulations Dr. Markman!
In Wine, There’s Health: Low Levels of Alcohol Good for the Brain
Friday, February 2, 2018
By Mark Michaud
While a couple of glasses of wine can help clear the mind after a busy day, new research shows that it may actually help clean the mind as well. The new study, which appears in the journal Scientific Reports, shows that low levels of alcohol consumption tamp down inflammation and helps the brain clear away toxins, including those associated with Alzheimer's disease.
"Prolonged intake of excessive amounts of ethanol is known to have adverse effects on the central nervous system," said Maiken Nedergaard, M.D., D.M.Sc., co-director of the Center for Translational Neuromedicine at the University of Rochester Medical Center (URMC) and lead author of the study. "However, in this study we have shown for the first time that low doses of alcohol are potentially beneficial to brain health, namely it improves the brain's ability to remove waste."
The finding adds to a growing body of research that point to the health benefits of low doses of alcohol. While excessive consumption of alcohol is a well-documented health hazard, many studies have linked lower levels of drinking with a reduced risk of cardiovascular diseases as well as a number of cancers.
Lungs Mays Hold Key to Thwarting Brain Damage after a Stroke
Wednesday, January 31, 2018
By Mark Michaud
The harm caused by a stroke can be exacerbated when immune cells rush to the brain an inadvertently make the situation worse. Researchers at the University of Rochester Medical Center (URMC) are studying new ways to head off this second wave of brain damage by using the lungs to moderate the immune system's response.
"It has become increasingly clear that lungs serve as an important regulator of the body's immune system and could serve as a target for therapies that can mitigate the secondary damage that occurs in stroke," said URMC neurologist Marc Halterman, M.D., Ph.D. "We are exploring a number of drugs that could help suppress the immune response during these non-infection events and provide protection to the brain and other organs."
Halterman's lab, which is part of the Center for NeuroTherapeutics Discovery, has been investigating domino effect that occurs after cardiac arrest. When blood circulation is interrupted, the integrity of our intestines becomes compromised, releasing bacteria that reside in the gut into the blood stream. This prompts a massive immune response which can cause systemic inflammation, making a bad situation worse.
While looking at mouse models of stroke, his lab observed that a similar phenomenon occurs. During a stroke blood vessels in the brain leak and the proteins that comprise the wreckage of damaged neurons and glia cells in the brain make their way into blood stream. The immune system, which is not used to seeing these proteins in circulation, responds to these damage-associated molecular patterns and ramps up to respond. Mobilized immune cells make their way into the brain and, finding no infection, nevertheless trigger inflammation and attack healthy tissue, compounding the damage.
The culprit in this system-wide immune response is neutrophils, a white cell in the blood system that serves as the shock troops of the body's immune system. Because our entire blood supply constantly circulates through the lungs, the organ serves as an important way station for neutrophils. It is here that the cells are often primed and instructed to go search for new infections. The activated neutrophils can also cause inflammation in the lungs, which Halterman suspects may be mistakenly identified as post-stroke pneumonia. The damage caused by activated neutrophils can also spread to other organs including the kidneys, and liver.
Electrical Stimulation in Brain Bypasses Senses, Instructs Movement
Thursday, December 7, 2017
The brain’s complex network of neurons enables us to interpret and effortlessly navigate and interact with the world around us. But when these links are damaged due to injury or stroke, critical tasks like perception and movement can be disrupted. New research is helping scientists figure out how to harness the brain’s plasticity to rewire these lost connections, an advance that could accelerate the development of neuro-prosthetics.
A new study authored by Marc Schieber, M.D., Ph.D., and Kevin Mazurek, Ph.D. with the University of Rochester Medical Center Department of Neurology and the Del Monte Institute for Neuroscience, which appears today in the journal Neuron, shows that very low levels of electrical stimulation delivered directly to an area of the brain responsible for motor function can instruct an appropriate response or action, essentially replacing the signals we would normally receive from the parts of the brain that process what we hear, see, and feel.
“The analogy is what happens when we approach a red light,” said Schieber. “The light itself does not cause us to step on the brake, rather our brain has been trained to process this visual cue and send signals to another parts of the brain that control movement. In this study, what we describe is akin to replacing the red light with an electrical stimulation which the brain has learned to associate with the need to take an action that stops the car.”
December 7th - Neurology for the Primary Care Provider Conference
Tuesday, November 28, 2017
Now in its twenty-fourth year, Neurology for the Primary Care Provider continues to attract a large audience of clinicians who manage patients with acute and chronic neurologic disorders in diverse settings. Each year, over 100 health care professionals – approximately one half of whom are physicians – attend this conference. The program highlights the most recent diagnostic and treatment advances in the field of neurology, utilizing a highly interactive case-based format.
The lecturers in this course are pre-eminent experts in their fields, who have also demonstrated superior skills at presenting material of this type to large audiences. This year’s speakers include Drs. Colleen Tomcik, M.D., Ralph Jozefowicz, M.D., Andrew Southerland, M.D. and Jonathan Marcus, M.D.
- Tomcik is an Assistant Professor of Neurology in the General Neurology Unit at the University of Rochester and will be speaking on headache.
- Jozefowicz is Professor of Neurology and Medicine, and Associate Chair for Education in the Department of Neurology at the University of Rochester and will be speaking on the Five Minute Neurological Examination.
- Southerland is an Assistant Professor of Neurology at the University of Virginia and will be speaking on stroke.
- Marcus is an Associate Professor of Neurology in the Sleep Disorders Unit at the University of Rochester and will be speaking on sleep disorders.
Parkinson’s Disease: A Looming Pandemic
Tuesday, November 14, 2017

New research shows that the number of people with Parkinson’s disease will soon grow to pandemic proportions. In a commentary appearing today in the journal JAMA Neurology, University of Rochester Medical Center neurologist Ray Dorsey, M.D. and Bastiaan Bloem, M.D., Ph.D., with Radboud University Medical Center in the Netherlands, argue that the medical community must be mobilized to respond to this impending public health threat.
“Pandemics are usually equated with infectious diseases like Zika, influenza, and HIV,” said Dorsey. “But neurological disorders are now the leading cause of disability in the world and the fastest growing is Parkinson’s disease.”
The piece builds upon the Global Burden of Disease study, also co-authored by Dorsey, which appeared in The Lancet Neurology in September and showed that neurological disorders are now the leading source of disability globally. That study tracked the prevalence of neurological diseases like Parkinson’s, Alzheimer’s, stroke, epilepsy, meningitis, encephalitis, multiple sclerosis, and migraine, both globally and by country.
Neurology for the Primary Care Provider XXIV: Updates in the Diagnosis and Treatment of Common Neurologic Disorders
Sunday, November 12, 2017
The University of Rochester Institute for Innovative Education is pleased to announce the upcoming event, Neurology for the Primary Care Provider XXIV. This educational program includes a one-day conference that will take place on Thursday, December 7, 2017, at the University of Rochester Medical Center in Rochester, NY.
Course Description
Now in its 24th year, Neurology for the Primary Care Provider continues to attract a large audience of clinicians who manage patients with acute and chronic neurologic disorders in diverse settings. Each year, over 100 health care professionals – approximately one half of whom are physicians – attend this conference. The program highlights the most recent diagnostic and treatment advances in the field of neurology, utilizing a highly interactive case-based format.
Birbeck Honored for Work Combating Malaria in Africa
Thursday, October 26, 2017

University of Rochester Medical Center neurologist Gretchen L. Birbeck, M.D., M.P.H., has
been recognized by the American Neurological Association (ANA) with one of its 2017
scientific awards for her research on the neurological damage associated with malaria in sub-Saharan Africa. Birbeck
divides her time between Rochester and health projects in Africa.
The ANA, a professional organization representing the nations top academic neurologists and neuroscientists,
announced it 2017 scientific awards at its annual meeting last week in San Diego. The awards recognize leaders in
academic neurology and neuroscience who have exemplified excellence in a number of areas, including stroke, dementia
and neurodegenerative disease.
Birbeck was recognized with the ANAs Soriano Lectureship, which was established in 1987 by ANA member Victor Soriano
and his wife to provide a brilliant lecture delivered by an outstanding scientist who is a member of the
Association.
During her presentation, Birbeck described research to blunt neurological consequences and behavioral disorders,
cognitive impairment, and seizures that can often accompany cases of pediatric cerebral malaria. The disease is a
major global health concern and impacts approximately 400,000 children in Africa each year.
Postdoctoral Fellow Wins Prize for Brain Injury Research
Tuesday, October 24, 2017

Stephen Steadman '64, center, presents Kevin Mazurek, left, with the first place honor and audience prize at the Meliora Weekend competition for the Steadman Family Postdoctoral Associate Prize in Interdisciplinary Research. Steadman, who received a BS in physics from the University of Rochester, is a scientific administrator at the Laboratory for Nuclear Science and the Department of Physics at MIT. Melissa Sturge-Apple, dean of graduate studies, is at right. (University of Rochester photo / Bob Marcotte)
Even simple movements require the integration of information from multiple areas of the brain. This process breaks down when brain damage occurs, resulting in neurological disorders.
But what if researchers could find a way to bypass those damaged areas and maintain the flow of information?
Kevin Mazurek, a postdoctoral fellow in the lab of Marc Schieber, professor of neurology, described how the lab is making progress in doing just that. He finished in first place and took the audience prize as well in the Meliora Weekend competition for the Steadman Family Postdoctoral Associate Prize in Interdisciplinary Research.
Mazurek’s prizes were worth $1,250.
Using micro electrical stimulation in primates, “we’ve shown that we can deliver the information successfully to two functionally different areas of the brain,” Mazurek explained. “This is an important first step.”
The next steps in the research, which incorporates neurology, neuroscience, electrical engineering, and biomedical engineering, include expanding the ability to communicate information across a wide reach of brain areas. This could “potentially improve the quality of living for individuals with injuries such as stroke, traumatic brain injury, or Alzheimer’s disease.”
This is the second year of the competition.
It is open to all postdoctoral scholars and appointees in the School of Medicine and Dentistry, and in Arts, Sciences & Engineering. Four prizes are awarded for research that exemplifies the importance of cross- disciplinary approaches toward examining high impact questions of science. Prizes were awarded based on 3-minute oral presentations to a panel of judges.
This year’s topics ranged from “Recent Breakthroughs in Understanding the Brain’s Waste Removal System” to “Catalytic Solar-Driven Generation of H2 in Artificial Photosynthesis” – and the benefits of yoga in helping cancer patients cope with the side affects of chemotherapy.
Data and Technology Drive New Approaches to Parkinson’s Care, Research
Wednesday, October 18, 2017
Complex, multi-system diseases like Parkinson’s have long posed challenges to both scientists and physicians. University of Rochester Medical Center (URMC) researchers are now reaching for new tools, such as algorithms, machine learning, computer simulations, and mobile technologies, to both improve care and identify new therapies.
Parkinson's disease is a progressive neurological disorder that erodes an individual’s control over their movements and speech. While many of the recent advances in treatment have transformed Parkinson’s into a manageable chronic illness, the individual patient experience can vary widely in both the onset and progression of the symptoms of the disease. This creates problems for clinicians who must constantly tweak the combination and doses of medications to effectively manage symptoms and researchers who are often confronted with a range of responses to experimental treatments.
The advent and spread of new technologies – such as to broadband internet, smartphones, and remote monitoring and wearable sensors – coupled with growing investments in computational resources and expertise in fields such as bioinformatics and data science have the potential to provide researchers with unprecedented insight into the complex variations of diseases like Parkinson’s.
An example of this approach is new research out in the journal The Lancet Neurology. The study sought to identify genetic markers that may explain why motor symptoms –stiffness or rigidity of the arms and legs, slowness or lack of movement, tremors, and walking difficulties – come on more rapidly for some patients with the disease.
The research involved Charles Venuto, Pharm.D., an assistant professor in the URMC Department of Neurology and the Center for Health + Technology (CHeT), and GNS Healthcare, and was funded by the Michael J. Fox Foundation for Parkinson’s Research and the National Institute of Neurological Disorders and Stroke.
The researchers tapped into huge data sets compiled by the Parkinson’s Progression Markers Initiative (PPMI) which has collected biological samples and clinical data from hundreds of individuals with the disease.
“We have access to more information about diseases like Parkinson’s than ever before,” said Venuto. “But all of that data has created a scientific conundrum akin to losing sight of the forest for the trees. In order to unlock the potential of this information we need to harness more sophisticated ways to understand what we are seeing.”
In a departure from traditional research approaches, the team turned over the vast quantities of genetic, clinical, and imaging profiles compiled by the PPMI study to a machine learning and simulation program. As the computer program analyzed the data, it was also “learning” by constantly refining and modifying its criteria and algorithms as it sifted through the information looking for patterns and associations.
The study identified a mutation in the LINGO2 gene that, together with a second gene and demographic factors, could identify patients with faster motor progression of Parkinson’s. The finding, if confirmed, could ultimately help clinicians refine care and help researchers more precisely understand how individual patients may respond to experimental therapies.
The application of data-driven technologies to biomedical research has exploded in the last several years. URMC neurologist Ray Dorsey, M.D., M.B.A., who is also the director of CHeT, has been at the forefront of this transformation. Dorsey has long been a pioneer in expanding access to Parkinson’s care via telemedicine.
Inherited Neuropathies Patient Day Meeting
Tuesday, October 10, 2017

On Saturday, September 16th in the Helen Wood Hall Auditorium 125 people gathered for the 1st Inherited Neuropathies Patient Day from 8:30 am – 3:30 pm. In attendance were patients with Inherited Neuropathies, caregivers, staff, and speakers. The Patient Day included speakers from the University of Rochester Medical Center and Round Table Discussions with Inherited Neuropathies patients and caregivers. The meeting allowed patients and caregivers to learn about patient care and research.
Some highlights from the Inherited Neuropathies Patient Day Meeting were Round Table Discussions which included patients, spouses, and parents talking about life with Inherited Neuropathies, lessons learned, and helpful resources. A second Round Table Discussion involved patients in Inherited Neuropathies research. Patients and caregivers had several opportunities to meet other individuals and to share their stories throughout the day during breaks, lunch, and at the end of the meeting.
Featured Presentations at the Inherited Neuropathies Patient Day Meeting included:
Inherited Neuropathies: What are they and how are they diagnosed? by Dr. David Herrmann
Role of Physical Therapy in the management of Inherited Neuropathies by Katy Eichinger, P.T., Ph.D.
Orthotic Management of Charcot Marie Tooth Neuropathies (CMT) by Alicia Gotcsik, CO, CPed
When is Orthopaedic Surgery a good choice and what does in entail? by Dr. Judy Baumhauer
Neuropathic Pain Management: CMT and Fabry’s Disease by Dr. John Markman
How We Do It: Round Table Discussion and Q & A session featuring insights from Patients featuring Patients affected by Inherited Neuropathies and Facilitated by Cindy Gibson, NP and Deb Guntrum, FNP
Update on Inherited Neuropathy Research by Dr. David Herrmann
Participation in Research by: Joan Mountain, RN and Janet Sowden, BSc (Hons)
Round Table Discussion: Patient Perspective for participating in Research
Study Will Explore Link Between HIV, Micro-Strokes, and Dementia
Monday, October 2, 2017
New research will seek to understand why people who are HIV positive are more susceptible to a progressive cerebrovascular disease that can ultimately give rise to dementia. One of the goals of the research is to identify new ways to prevent the blockages that occur in blood vessels and cause damage in the brain.
The $3.6 million National Institute of Aging-sponsored study will be led by University of Rochester Medical Center (URMC) neurologist Giovanni Schifitto, M.D., M.S., and Sanjay B. Maggirwar, M.B.A., Ph.D., with the Department of Microbiology and Immunology.
While it is estimated that more than 1 million Americans are living with HIV, treatments such as combined anti-retroviral therapies (cART) have transformed the disease into a manageable chronic illness. However, as the population living with HIV ages, the long-term effects of both the infection and treatment have given rise to additional health problems.
One such problem is cerebral small vessel disease (CSVD). While the reason CSVD occurs is not clear and may ultimately be the result of a number of factors, a common mechanism is believed to be inflammation. The new study will examine the interaction of two types of blood cells – platelets and monocytes. When these cells become stuck together and form complexes the resulting blockages can lead to a hardening of the arteries.
The brain in particular is highly susceptible to damage when blood flow becomes impaired due its network of tiny vessels. When complexes of platelets and monocytes accumulate in the brain they can promote inflammation which can cause vessels to become leaky, plugged, or burst, resulting in micro-strokes or micro-hemorrhages that damage neurons and other tissue in the brain.
Moving for Parkinson’s Disease
Wednesday, September 27, 2017
The URMC Movement Disorders team is participating this weekend in Moving Day, the Parkinson Foundation's annual community awareness and fundraising walk. The event is Sunday, October 1st on the MCC campus, with registration beginning at 9AM.
Funds raised from this event support programs in the community such as the PD education series, a variety of exercise programs and support groups, as well as grant funding for the University of Rochester's the Parkinson Foundation Center of Excellence. The event is family-friendly with kid's activities, a movement pavilion showcasing different exercise programs, and a "Parkinson's Experience" tent run by Michelle Burack, MD, PhD, equipped with a variety of accessories that reproduce PD symptoms for people without the disease to experience.
Show your support for our Movement Disorders team by donating here: Click Here To Donate
Study Says Video Conferencing Offers Quality Care
Wednesday, September 20, 2017
A new study has found that video conferencing can deliver quality care to patients who have Parkinson's disease. Published in the Aug. 16, 2017, online issue of Neurology®, this study is the first national randomized controlled trial of telemedicine to connect remote specialists to patients directly in their homes. The results support CAST's technology policy priorities.
"Over 40% of people with Parkinson's disease never receive care from a neurologist, yet studies have shown that people who see a neurologist are less likely to be hospitalized with illnesses related to Parkinson's disease, have greater independence, and are less likely to die prematurely," said study author Ray Dorsey, MD, the David M. Levy Professor of Neurology at the University of Rochester Medical Center (URMC) and lead author of the study.
Many Parkinson's patients live far from movement disorder specialists and/or have mobility and driving challenges that make doctor visits difficult. The 195 study participants received either their usual care from their usual providers or their usual care and up to four video conference visits with a neurologist who they had not seen before. The study did not include people with the disease who live in nursing homes, who account for nearly 25% of all Medicare beneficiaries with Parkinson's disease.
Each virtual house call provided the same quality of care and saved the patients an average of 169 minutes and nearly 100 miles of driving. "Telemedicine is especially valuable to patients in remote, rural, and underserved areas because it gives them the ability to consult specialists they would otherwise have to travel hours to see," said Peter Schmidt, Ph.D., Senior Vice President, Chief Research and Clinical Officer of the Parkinson's Foundation, said in University of Rochester Medical Center (URMC) news.
"Broader adoption of this technology has the potential to expand access to patient-centered care," Dorsey told URMC news. "We now have the ability to reach anyone, anywhere but the promise and benefits of telemedicine will not be fully realized until the changes are made in Medicare policy."
CAST and Study Results
This study supports a recent LeadingAge Aging Services Technology Issue Brief, which holds that telemedicine can help long-term and post-acute care providers deliver integrated and person-centered care, supporting older adults' health. These technologies are essential to strategic partnerships with physicians, hospitals, Accountable Care Organizations, and other coordinated care delivery models that will improve the quality of life and care, while easing care burdens and cost.
CAST's technology policy priorities, set at the March 2014 CAST Commissioners Meeting, include advocating with agencies of the U.S. Department of Health and Human Services, including CMS and its Center for Medicare and Medicaid Innovation, for more demonstration projects focusing on health IT and telehealth.
The Patient-Centered Outcomes Research Institute supported the recent study.
Do the Drugs that Keep HIV Patients Alive Damage Their Brains?
Friday, August 25, 2017
Researchers from the University of Rochester Medical Center recently set out to understand whether drugs used to keep HIV patients alive could be damaging their brains. On the contrary, early results from their clinical study showed that short-term use of combination anti-retroviral therapy (cART) improved mental function in HIV-infected individuals.
Giovanni Schifitto, M.D., M.S., professor of Neurology at the University of Rochester Medical Center, is leading the study to better understand the short and long term effects of combination antiretroviral therapy on HIV patients’ brains. At 12 weeks, the therapy appears to improve mental performance and functional connectivity in the brain.
HIV patients often experience mental decline ranging from mild impairment to full-blown dementia. Experts have long debated the cause of that mental decline: HIV itself, or the drug used to combat it.
Some of the first HIV drugs were known to cause damage to peripheral nerves. Newer anti-retroviral drugs are believed to be safer, but patients taking these drugs continue to experience mental impairment - even when their viral load is extremely low. In fact, some studies have shown improvement in HIV patients’ mental function when they stop using cART.
“But those studies were very indirect,” said Schifitto, who is also the director of the Clinical Research Center and function leader for Participant and Clinical Interactions at the CTSI. “They studied cohorts of people who were already on medications, which makes it very hard to pull apart whether the virus or the drug is to blame for effects in the brain.”
Schifitto’s clinical study, on the other hand, followed 17 HIV-infected individuals who had not received any treatment prior to the study. These patients scored worse on mental function tests and brain imaging revealed fewer connections in their brains than the HIV-negative control group.
After receiving cART for 12 weeks, the HIV patients’ mental performance and functional brain connectivity improved nearly to the level of the HIV-negative group. This not only suggests that short term cART use does not damage the brain, but that the virus is the culprit for early mental impairment in HIV-infected patients.
However, this is just a first step of the study, which will enroll and follow over 150 participants for two years. It is possible that cART will cause mental decline after prolonged use and the team want to track if and when that happens. They are also monitoring sleep, mood, and several other factors that can impact mental function in HIV patients taking cART.
In the end, the outcomes of the short and long term studies may help health care providers tailor cART cocktails and treatment schedules to individual patients’ needs. The results could also have implications for preventative use of cART in individuals who are at high risk for contracting HIV, a practice called pre-exposure prophylaxis (PrEP).
The study started with just a single site at the University of Rochester Medical Center, but now includes sites at Cornell Medical Imaging Center, Gay Men’s Health Crisis, SUNY Upstate Medical, University at Buffalo, and University of Texas Health Science Center at Houston. It also utilized the CTSI’s Clinical Research Center, a dedicated space for researchers to conduct safe and controlled clinical studies with the support of highly trained clinical research staff.
Ray Dorsey Study: Telemedicine as Effective as In-Person Care for Parkinson’s
Wednesday, August 16, 2017
New findings from a nationwide program that links neurologists with patients with Parkinson’s disease in their homes via video conferencing shows that telemedicine can successfully deliver quality care. The study, which appears today in the journal Neurology, points to a new way to improve care for people who suffer from the disease, but may have not have access to a neurologist.
“Virtual house calls for chronic diseases like Parkinson’s are not only as effective as in-person care but broader adoption of this technology has the potential to expand access to patient-centered care,” said Ray Dorsey, M.D., the David M. Levy Professor of Neurology at the University of Rochester Medical Center (URMC) and lead author of the study. “We now have the ability to reach anyone, anywhere but the promise and benefits of telemedicine will not be fully realized until the changes are made in Medicare policy.”
“Telemedicine is especially valuable to patients in remote, rural, and underserved areas because it gives them the ability to consult specialists they would otherwise have to travel hours to see,” said Peter Schmidt, Ph.D., Senior Vice President, Chief Research and Clinical Officer of the Parkinson’s Foundation. “The Parkinson’s Foundation aims to narrow these gaps in Parkinson’s care, which is why we are working with experts from URMC, a Parkinson’s Foundation Center of Excellence.”
The results in the paper come from the Connect.Parkinson project, a research study funded by the federal Patient-Centered Outcome Research Institute. Connect.Parkinson is led by URMC in collaboration with the Parkinson’s Foundation and with additional support from PatientsLikeMe, the Michael J. Fox Foundation for Parkinson’s Research, SBR Health, Vidyo, and IDSolutions. The study is the first national randomized controlled clinical trial of telemedicine for Parkinson’s disease.
It is estimated that 40 percent of people who have Parkinson’s disease do not see a neurologist soon after diagnosis. This places them at significantly greater risk of falls leading to hip fractures, ending up in a nursing home or hospital, and even death. This challenge of providing care to these individuals will become ever greater as the population ages—it is projected that the number of people with Parkinson’s disease will double by 2030.
The most significant barriers to appropriate care for Parkinson’s patients are distance and disability. Most movement disorder specialists are located in academic medical centers in large urban areas. Most patients live in suburban and rural areas, have impaired mobility and driving ability, and are faced with the challenge of making frequent trips to the doctor’s office – a task that becomes more difficult as the disease progresses.
The goal of the Connect.Parkinson study was to see if telemedicine would allow neurologists to deliver care to patients in the comfort of their homes. A total of 195 individuals with Parkinson’s from across the U.S. were selected to participate in the study. Participants either received care through their primary care physician or had that care supplemented with up to four visits via video conference with the neurologist they had not seen before.
Parkinson’s disease particularly lends itself to telemedicine because many aspects of the diagnosis and treatment of the disease are “visual” – meaning that the interaction with the doctor primarily consists of listening to the patient and observing them perform certain tasks such as holding their hands out or walking.
The researchers found that the telemedicine visits were as effective as in-person visits in the doctor’s office, with the quality of life reported by the participants as no better or worse for people who received care in their homes compared with those who received standard care. The virtual house calls also saved patients an average of 169 minutes and nearly 100 miles of travel per visit.
While the current study is one of several that have demonstrated the potential benefits of telemedicine, widespread adoption of this technology is hindered by federal healthcare policies. Approximately two-thirds of Parkinson’s patients are on Medicare. However, the program does not reimburse for in-home telemedicine care. Legislation has been introduced in Congress to allow Medicare to expand reimbursement for telemedicine.
“We can shop, bank, make travel reservations, take classes, and buy groceries via the internet from the comfort of our own homes, but too many patients still cannot access health care,” said Dorsey. “Telemedicine is an option if you are a veteran, a member of the Armed Services, a Medicaid beneficiary, or a Canadian, but not if you have a chronic condition and are a Medicare beneficiary.”
Additional co-authors of the study researchers from URMC, the Parkinson’s Foundation, Simone Consulting, Johns Hopkins School of Medicine, the University of Pennsylvania Perelman School of Medicine, the University of California San Francisco, Northwest Neurology, Oregon Health and Science University, Baylor College of Medicine, Augusta University, Duke Medical Center, Massachusetts General Hospital, Struther’s Parkinson’s Center, Beth Israel Deaconess Medical Center, the University of Miami, Northwestern University, the Feinstein Institute of Medical Research, the Medical University of South Carolina, the University of Kansas Medical Center, the Parkinson’s Institute, the Mayo Clinic, the University of California Berkeley, the Karolinska Institute in Sweden, and PatientsLikeMe. The study was funded with support from the Patient-Centered Outcome Research Institute.
Neurology and Neurosurgery Earn Top 50 Ranking in U.S. News & World Report's 'Best Hospitals'
Wednesday, August 9, 2017
Strong Memorial Hospital’s Neurology and Neurosurgery specialty program has been ranked among the top 50 in the
nation for 2017-2018 by U.S. News & World Report. The program ranked 39th among the nation’s
hospitals, and this is the seventh consecutive year it has been nationally ranked by U.S. News.
In June, UR
Medicine’s Golisano Children’s Hospital was
recognized as one of the nation’s best children’s hospitals in three specialty areas — Neonatology,
Nephrology, and Neurology and Neurosurgery — in the U.S. News & World Report’s Best
Children’s Hospital rankings.
For the 2017-18 adult rankings, U.S. News evaluated more than 4,500 U.S. hospitals; only 152 were ranked in at
least one specialty.
Eight Strong Memorial Hospital specialty programs earned High Performing ratings: Cardiology and Heart Surgery,
Diabetes and Endocrinology, Gastroenterology and GI Surgery, Geriatrics, Nephrology, Orthopaedics, Pulmonology, and
Urology.
U.S. News recognized hospitals that were high-performing across multiple areas of care and ranked them within
their states and by metropolitan areas. U.S. News rated Strong Memorial as the top hospital in the Rochester
Metro area and fourth among New York state hospitals.
U.S. News evaluates nearly 5,000 hospitals nationwide for its
Best Hospitals rankings; methodologies include objective measures such as patient survival, the number of
times a given procedure is
performed, infection rates, adequacy of nurse staffing and more.
Surviving a Stroke Propels Career in Brain Research
Wednesday, July 26, 2017
Left to right: Brad Mahon, Frank Garcea, and Edward Vates
On a warm day in July 2005, Frank Garcea’s soccer playing days came to an abrupt end when he suffered what could have been a deadly stroke during a practice with his teammates. Instead, the events of that day and his subsequent treatment – which serve as the basis for a review published in the New England Journal of Medicine (NEJM) – set him on a career path that would ultimately lead to a Ph.D. studying how the brain recovers from injury.
Garcea, who was about to begin his senior year at the Aquinas Institute in Rochester, was in the middle of a training session when he started experiencing a pounding headache. He first suspected he might just be dehydrated on that hot summer day, but soon after his limbs began to tingle and grow numb, his eyes became sensitive to the bright sunlight, and he had difficulty walking. Very quickly it became obvious that something was wrong and someone called 911.
Garcea eventually ended up at Strong Memorial Hospital and was diagnosed with a subarachnoid hemorrhage. He would undergo surgery the next morning under the clinical care of UR Medicine neurosurgeon Edward Vates, M.D., Ph.D.
Subarachnoid hemorrhages account for approximately 5-10 percent of all strokes in the U.S. These occur when a blood vessel in the brain bursts causing bleeding. If not treated immediately, these strokes can cause major disability and, in many cases, death.
“When an aneurysm ruptures, it is an intracranial catastrophe,” said Vates, a co-author of the NEJM article. “In 25 to 50 percent of cases, these strokes result in death, and this estimate does not fully account for patients who die before receiving medical attention.”
Vates uses Garcea’s experience as jumping off point to describe the decision-making process required to diagnose and identify treatment options for subarachnoid hemorrhages.
Faulty Support Cells Disrupt Communication in Brains of People with Schizophrenia
Thursday, July 20, 2017

Astrocytes help coordinate communication
between neurons. The one on the left is
derived from a healthy brain and the one on
the right is from an individual diagnosed
with schizophrenia.
New research has identified the culprit behind the wiring problems in the brains of people with schizophrenia. When researchers transplanted human brain cells generated from individuals diagnosed with childhood-onset schizophrenia into mice, the animal’s nerve cell networks did not mature properly and the mice exhibited the same anti-social and anxious behaviors seen in people with the disease.
“The findings of this study argue that glial cell dysfunction may be the basis of childhood-onset schizophrenia,” said University of Rochester Medical Center (URMC) neurologist Steve Goldman, M.D., Ph.D., co-director of the Center for Translational Neuromedicine and lead author of the study which appears today in the journal Cell. “The inability of these cells to do their job, which is to help nerve cells build and maintain healthy and effective communication networks, appears to be a primary contributor to the disease.”
Expanding local services for advanced neurological care
Sunday, July 9, 2017
Rapid changes in neuroscience and digital technology play important roles in improving neurological care at Cayuga Health System’s hospitals and building a seamless connection for local patients needing advanced care at UR Medicine in Rochester.
“The sub-specialties in neurology have grown rapidly in the last 20 years and are improving patient outcomes in complex areas of care,” says Dr. Richard L. Barbano, MD, PhD. and associate chair of Community Outreach and Regional Development at UR Medicine.
However, the most sophisticated neurological care is provided at major medical centers and not easily accessible to patients living far away from those programs. Upgrades in digital technology now allow Cayuga Health System hospitals to build a network of partnerships linking local health care to major research and teaching hospitals, such as UR Medicine.
“When Cayuga Health System’s strong general neurology program is combined with access to the broad range of neuroscience research, training, and sub-specialties in Rochester, patients with complicated neurological conditions receive the highest level of care,” Dr. Barbano says.
Emma Ciafaloni appointed Robert C. and Rosalyne H. Griggs Professor in Experimental Therapeutics of Neurological Disease
Friday, July 7, 2017
Emma Ciafaloni, professor of neurology, was jointly appointed as the Robert C. and Rosalyne H. Griggs Professor in Experimental Therapeutics of Neurological Disease for the period from April 1, 2017 through December 31, 2019. She retains her joint appointment as professor of pediatrics.
A specialist in the diagnosis and treatment of neuromuscular diseases and in clinical trials in both adults and children, Ciafaloni is codirector of the Muscular Dystrophy Association Neuromuscular Clinic, program director of the neuromuscular medicine fellowship, and Director of the Pediatric Neuromuscular Medicine program in the Medical Center’s Neuromuscular Disease Unit.
She published in the New England Journal of Medicine, JAMA, Journal of Child Neurology, the Journal of Immunology, and the Journal of Pediatrics.
Ciafaloni graduated from the medical school at the Universita’ Statale di Milano, in Milan, Italy; received training in mitochondrial diseases at Columbia University; and completed her neurology residency and neuromuscular fellowships at Duke University. She joined the Neurology Department at Rochester in 2002.
Golisano Children's Hospital Recognized by US News and World Report
Tuesday, June 27, 2017

UR Medicine’s Golisano Children’s Hospital has been recognized as one of the nation’s best children’s hospitals in three specialty areas — neonatology, nephrology, and neurology and neurosurgery — in the U.S. News & World Report’sBest Children’s Hospital rankings.
The 2017-2018 rankings, released online Tuesday, placed the children’s hospital’s neonatology program at No. 27 nationally; nephrology at No. 43; and neurology and neurosurgery at No. 44.
“As with everything we do and have achieved, this recognition reflects a partnership with contributions from the interdisciplinary workforces of pediatrics, surgery and surgical subspecialties, emergency medicine, neurology, and obstetrics and gynecology,” said Nina Schor, M.D., Ph.D., pediatrician-in-chief at Golisano Children’s Hospital. “It also wouldn’t be possible without our community, and the health care organizations outside the hospital.”
The Division of Neonatology, which provides care for premature and critically ill newborns, admits about 1200 infants per year. Approximately 1 in 12 babies born in the Finger Lakes Region spend their first days in the children’s hospital’s Gosnell Family Neonatal Intensive Care Unit (NICU), which is the region’s only Level IV NICU.
UR Medicine Recognized for Stroke Care
Tuesday, June 27, 2017

The American Heart Association/American Stroke Association (AHA/ASA) has once again honored the UR Medicine Strong Memorial Hospital as having met its highest standards of care for stroke.
Strong Memorial Hospital has received the AHA/ASA Get With The Guidelines program’s Stroke Gold Plus Quality Achievement Award. The hospital was also tapped for the Target: Stroke Honor Role Elite Plus, which recognizes hospitals that have consistently and successfully reduced door-to-needle time – the window of time between a stroke victim’s arrival at the hospital, the diagnosis of an acute ischemic stroke, and the administration of the clot-busting drug tPA. If given intravenously in the first three hours after the start of stroke symptoms, tPA has been shown to significantly reduce the effects of stroke and lessen the chance of permanent disability.
“This recognition is a testament to the hard work of our outstanding team of nurses, physicians, and therapists and their dedication to provide the highest quality of care to stroke victims,” said neurologist Curtis Benesch, M.D., M.P.H., the medical director of the UR Medicine Comprehensive Stroke Center.
“This award reflects a singular focus on improving the care stroke victims receive from the first 911 call to when they arrive at the hospital through operating room, neurocritical care, and rehabilitation,” said Tarun Bhalla, M.D., Ph.D., the surgical director of the Comprehensive Stroke Center.
Strong Memorial Hospital is home to the region’s only Comprehensive Stroke Center, a designation by the Joint Commission that indicates that the hospital either meets or exceeds the highest standards of care required to provide timely and comprehensive care to patients with complex cerebrovascular disease.
The AHA/ASA Get With the Guidelines program recognizes hospitals that have reached aggressive goals of treating stroke patients and comply with core standard levels of care. For more information about the Get With The Guidelines program, visit the AHA/ASA website.
Special Chair Update - Two Legendary Faculty
Monday, June 19, 2017
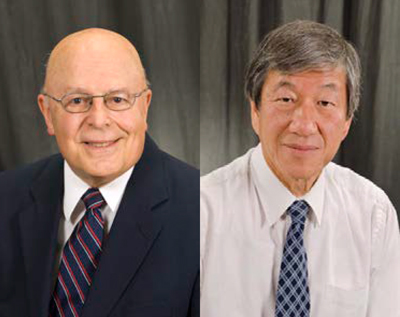
Retirements do not happen often. On June 30th, 2017 Drs.
Richard Moxley and David Wang will be retiring. They both will
become Emeritus Professors in recognition of their outstanding
contributions to the Department, School and University.
They both started in the Department in 1974, 43 years ago, Dick
as a faculty and David as a resident. And they stayed, one
practicing primarily adult neurology (Dick) and the other (David)
child neurology, but each doing a little bit of both along the way.
Free Telemedicine Program for Parkinson's Patients
Wednesday, May 31, 2017
A program called Parkinson's Disease Care New York exists to help eliminate the obstacles facing patients who need to see a neurologist. This type of doctor can mainly be found in large metropolis areas so anyone in a rural community might have a tough time getting access to healthcare.
By linking the patient to the doctor via computer, the neurologist can monitor symptoms more regularly and follow the patient more closely—even diagnose new treatments without the patient even leaving their home. Currently 109 patients are enrolled and the program can provide for 500 people statewide. To find out more, go to the PDCNY Facebook page.
Featured in The Science Times: How Alzheimer's Catches People Skimping Sleep: New Study Explains Cause Of Dementia
Wednesday, May 24, 2017

A recent scientific study shows that insufficient amount of sleep leads to the development of Alzheimer's disease. Researchers gain more evidence and are beginning to believe that lack and poor quality of sleep results to the fusion of Amyloids, proteins that bond together to form Alzheimer's plaques.
Dr. Maiken Nedergaard, the lead researcher from the University of Rochester Medical Center, explains the glymphatic system that is present in humans. She says that this system is 10 times more active when in slumber than when awake. The process allows cerebrospinal fluid to flow through spaces around the neurons of people's brains. This a method of purging unwanted proteins (Amyloids) and other wastes into the circulatory system garbage collectors and eventually flushes it out of the body.
In simple terms, Nedergaard explains that the brain has its own sanitation and public works department. It is like a network of sewer facilities mostly done during the brain's nightlife. An example of a housekeeping staff descending to building offices for a cleanup duty to avoid the lumping compound that causes Alzheimer's.
URMC’s Telemedicine Efforts Build on a Firm Foundation
Thursday, May 18, 2017
The fast-rising tide of telemedicine will transform health care nationwide. Here at URMC, dozens of faculty and departments are already ensuring our readiness to embrace the opportunities and meet the challenges of that transformation, even as we continue to help drive it forward with our innovative programs.
The recent appointment of Ray Dorsey, M.D., director of the Center for Human Experimental Therapeutics and professor of Neurology, as URMFG’s Medical Director of Telemedicine reflects our growing commitment to the technology, but the work his colleagues have been doing means he has a firm foundation to build on. We’ve been providing telemedicine in some form for well over a decade, and the already-significant number of services available here is constantly growing.
Waves of Innovation
Imagine a health care system in which a doctor can check a patient’s airway before surgery with a smartphone instead of bringing the patient in for an extra appointment, or listen to the heart and lungs of a recently discharged patient at home to help prevent readmissions.
For URMC, that’s already the reality, and in some departments it has long been routine. Pediatrics, for example, piloted telemedicine programs 15 years ago and remains a leader. Under the leadership of Kenneth McConnochie, M.D., M.P.H., professor of Pediatrics, and Neil Herendeen, M.D., M.S., medical director of the Strong Pediatric Practice, Rochester-area primary care physicians have offered pediatric telemedicine visits to students in the Rochester City School District and many childcare centers for over a decade in a highly successful effort that has provided care to thousands of children.
“A clearly demonstrated benefit for patients and their families is convenience,” said McConnochie, a nationally recognized expert who has appeared before Congress. “An important question has always been whether anything is lost when you gain that convenience. If telemedicine is done right—and that’s the challenge— our evaluations indicate that nothing is lost in diagnostic accuracy or in quality of communication with family. You get all the convenience of care when and where you need it, and equivalent quality of care.”
The benefits go beyond that. Parents get the peace of mind of having a quickly scheduled visit and the convenience of not needing to leave work to bring their children to the doctor. Childcares and schools get just-in-time physician guidance in addressing health issues. All of that leads to satisfaction for the providers involved.
“The impact ripples across all stakeholders in the care and education of children,” McConnochie said.
No wonder, then, that telemedicine is rippling across our institution and our service area. VNS monitors patients remotely, and primary care began piloting telemedicine visits this past July at their Manhattan Square Family Medicine and LeRoy Medical Associates locations. But those programs are only part of our effort.
We have nearly two dozen programs at various stages of implementation. Along with coordinating our telemedicine efforts, Dorsey works with Parkinson disease patients worldwide. Other faculty members offer genetic counseling, pediatric dental consultations for oral surgery, and mental health consultation and liaison services for primary care doctors, rural hospitals and long-term care facilities.
“Telemedicine means our highly skilled specialists can provide care to more people and make those interactions more convenient,” Dorsey said. “Our ultimate vision for URMC telemedicine is to enable any New Yorker to receive care from our faculty. We want to bring care to the patient, rather than the patient to care.”
Introducing the Center for NeuroTherapeutics Discovery
Tuesday, May 16, 2017
The Center for Neural Development and Disease, led by Harris A. (Handy) Gelbard, M.D., Ph.D., since 2008, will now be the Center for NeuroTherapeutics Discovery, reflecting an increased emphasis on translation and the creation of intellectual property that will lead to new therapies for nervous system disorders.
Gelbard, professor of Neurology, Pediatrics, Neuroscience and Microbiology & Immunology, will continue as director. His research, coupled with the work of Charles Thornton, M.D., professor of Neurology and Neuroscience, and Marc Halterman, M.D., Ph.D., associate professor of Neurology, Neuroscience and Pediatrics, will serve as the anchor of the new center. The trio has a strong track record of grants, publications, and patents, as well as academic and commercial relationships that they are actively pursuing to bring new treatments to the public.
“The Center for NeuroTherapeutics Discovery was developed out of the Center for Neural Development and Disease to create more visibility for academic and commercial partnerships as a necessary bridge for bringing new therapeutics forward,” said Gelbard. “This represents a way to do the best and most cutting edge science possible in a time when the traditional avenues towards funding academic research are changing rapidly.”
The center will bring together many investigators from across the Medical Center and River Campus to identify the mechanisms that lead to various neurological disorders, including HIV-associated neurocognitive disorder (Gelbard lab), myotonic dystrophy (Thornton lab) and stroke (Halterman lab). The center remains committed to its members that investigate the molecular signaling events that lead to nervous system disease during development and aging. Industry partnerships and resources will be sought to fast-track existing therapies or create new molecules that affect these disease mechanisms.
Treatments that harness the immune system to help regenerate damaged cells will be a major focus at the center; the team believes that this approach is broadly applicable to a range of acute and chronic neurodegenerative disorders, such as Parkinson’s disease, multiple sclerosis and Alzheimer’s disease.
Kayson Honored for Improving Care for Huntington’s Patients and Families
Thursday, May 4, 2017
 Elise Kayson, M.S., R.N.C., A.N.P., has been recognized by the Huntington Study Group with its Lifetime Achievement Award for her dedication to seeking treatments that make a difference and improving the quality of life and outcomes for families affected by the disease.
Elise Kayson, M.S., R.N.C., A.N.P., has been recognized by the Huntington Study Group with its Lifetime Achievement Award for her dedication to seeking treatments that make a difference and improving the quality of life and outcomes for families affected by the disease.
The Huntington Study Group (HSG) is a network of more than 400 investigators, coordinators, scientists, and Huntington's disease experts spread across more than 100 research sites across the globe. HSG brings together patients, families, academic and industry researchers, foundations, and government agencies to seek new treatments that improve the life of individuals with the disease.
Elise continues to be an essential ingredient and role model for the success of the HSG, the many patients and families who we serve, and is a real prize that we celebrate and emulate," said Ira Shoulson, M.D., the founder of the HSG, a former professor of Neurology at URMC, and currently a professor of Neurology at Georgetown University.
Elise's tireless commitment to Huntington's patients and their families and her 20 plus years of experience in pharmaceutical research has been essential to our efforts to develop new ways to treat this devastating disease," said URMC neurologist Ray Dorsey, M.D., M.B.A., chair of the HSG. This award recognizes her dedication and critical role she plays in managing the complex research necessary to bring new drugs to market."
Here’s What Your Future Doctor Visits Could Look Like
Wednesday, May 3, 2017
Today’s office visit to a doctor involves a patient, a family member, and a physician 97% of the time. Tomorrow’s visit will engage nurse practitioners, nutritionists, genetic counselors, pharmacists, therapists, social workers, mental health professionals, and exercise coaches. The Internet enables clinicians to connect patients at different times based on need, not travel burden. Just as more clinicians will contact patients, more caregivers including children living in different cities and countries will participate remotely in visits through video conferencing.
The nature of visits will also change. Patient-generated data creates the opportunity for the visit to be a true data exchange. Tomorrow’s visit will include objective, high frequency and real-time streaming data, including blood pressure, glucose levels, activity levels, diet, and social engagement metrics. Patients will control the data from novel sensors and grant clinicians access at the patients’ direction.
URMC Plays Key Role in New Huntington’s Drug
Thursday, April 6, 2017
University of Rochester Medical Center (URMC) researchers were instrumental in the U.S. Food and Drug Administration's (FDA) recent approval of SD-809 (deutetrabenazine) to treat Huntington's disease. Deutetrabenazine is the only the second drug authorized by the agency to treat this rare, inherited neurodegenerative disorder.
The FDA approval was based on results from the First-HD study, a Phase 3 clinical trial which was conducted through the Huntington Study Group (HSG) via a consortium of 34 sites across the U.S. and Canada on behalf of Teva Pharmaceuticals. The study results were published last July in Journal of the American Medical Association.
The URMC Clinical Trials Coordination Center (CTCC) and Department of Biostatistics and Computational Biology -- under the leadership of Elise Kayson, M.S., A.N.P., and David Oakes Ph.D. -- provided scientific, technical, logistical, and analytical support for the First-HD study The CTCC is part of the Center for Human Experimental Therapeutics (CHET) and is a unique academic-based research organization with decades of experience working with industry, foundations, and governmental researchers in bringing new therapies to market for neurological disorders.
URMC to Host Technology & Rare Neurological Diseases Symposium
Thursday, April 6, 2017
The Technology & Rare Neurological Diseases Symposium (TRNDS), taking place Friday, May 12, aims to spark a national discussion among patients, researchers, and policy experts on how to accelerate clinical trials for rare diseases that attack the nervous system. New technologies may ease the burden of traveling to research sites for patients and increase the flow of information about these diseases for researchers and healthcare providers.
Finding enough patients to conduct clinical studies on rare diseases can be very difficult. Patients are spread far and wide and are often required to travel long distances or even move to access care and participate in clinical trials. And patients with rare neurological diseases often have physical and/or mental disabilities that make travel even more burdensome.
These difficulties lead to a lack of "natural history" knowledge about these diseases -- what they are, who they impact, how symptoms unfold over time.
UR Medicine Opens Neuromedicine and Behavioral Health Center for Pediatric Patients
Friday, March 31, 2017

UR Medicine’s Neuromedicine and Behavioral Health Center celebrates its opening on March 29. The center brings together Developmental and Behavioral Pediatrics, Child Neurology, and Child Psychiatry to collaborate on care for pediatric patients, and is
home to the new William and Mildred Levine Autism Clinic that provides specialized care for patients with autism spectrum disorder.
This is the region’s first stand-alone center to integrate care of autism with pediatric neuromedicine and child and adolescent psychiatry services, and will serve more than 25,000 patients each year.
UR Medicine’s new 90,000-square-foot, three-story building, located at 200 East River Road, has created space to relocate outpatient imaging, interventional radiology clinics as well as autism/neuromedicine/behavioral health pediatric programs from the
University of Rochester Medical Center campus to an easily accessible location along the I-390 corridor. The site will be a regional destination for patients and families seeking
specialized pediatric services.
Protein Key to Nerve Health Hitches a Ride on Brain’s Garbage Truck
Thursday, March 9, 2017
 A new study shows that the brain’s waste removal system serves as both trash collector and delivery service, providing neurons with a protein important to maintaining cognitive function while simultaneously cleaning brain tissue. The research may help explain why different genetic varieties of the protein, called apolipoprotein E (apoE), can indicate risk for Alzheimer’s disease or promote longevity.
A new study shows that the brain’s waste removal system serves as both trash collector and delivery service, providing neurons with a protein important to maintaining cognitive function while simultaneously cleaning brain tissue. The research may help explain why different genetic varieties of the protein, called apolipoprotein E (apoE), can indicate risk for Alzheimer’s disease or promote longevity.
The study was led by Rashid Deane, B.Sc., Ph.D., a research professor in the University of Rochester Medical Center Department of Neurosurgery and member of the Center for Translational Neuromedicine, and appears in the journal Molecular Neurodegeneration.
ApoE is responsible for delivering cholesterol to nerve cells in the brain and plays a key role in synaptic plasticity, the process by which neurons build new connections in order to learn and store memories.
Protein Key to Nerve Health Hitches a Ride on Brain’s Garbage Truck
Wednesday, March 8, 2017
A new study shows that the brain's waste removal system serves as both trash collector and delivery service, providing neurons with a protein important to maintaining cognitive function while simultaneously cleaning brain tissue. The research may help explain why different genetic varieties of the protein, called apolipoprotein E (apoE), can indicate risk for Alzheimer's disease or promote longevity.
The study was led by Rashid Deane, B.Sc., Ph.D., a research professor in the University of Rochester Medical Center Department of Neurosurgery and member of the Center for Translational Neuromedicine, and appears in the journal Molecular Neurodegeneration.
Study: Home Care Improves Stroke Outcomes
Thursday, March 2, 2017

Stroke patients who are paired with caregivers that help them transition back to their homes are significantly less likely to be readmitted to the hospital. The results of the pilot study, which showed a 39 percent reduction in the readmission rates of stroke patients at Strong Memorial Hospital, were presented last week at the International Stroke Conference in Texas.
The study was authored by Ann M. Leonhardt Caprio, M.S., R.N., A.N.P. and Curtis G. Benesch, M.D., M.P.H. with the UR Medicine Comprehensive Stroke Center, and Denise Burgen, M.B.A., M.S.N., F.N.P, R.N. with UR Medicine Home Care.
The study focused on one of the measures used by the Centers for Medicare and Medicaid Services to determine quality of stroke care -- whether or not a patient is readmitted to the hospital within 30 days of being discharged after suffering a stroke.
Schor to Receive Child Neurology Society's Highest Honor
Tuesday, February 21, 2017

Nina Schor, M.D., Ph.D., William H. Eilinger Chair of Pediatrics and the pediatrician-in-chief at UR Medicine’s Golisano Children’s Hospital, has been named the recipient of the Child Neurology Society’s 2017 Hower Award, the organization’s highest honor.
The award is given annually to a child neurologist for being an outstanding teacher, scholar, and for making high levels of contributions to the field and to the Child Neurology Society. Schor, who has spent much of her career researching neuroblastoma, one of the most common childhood cancers, will be recognized at the society’s annual meeting in October, in Kansas City, Mo. She will also have the honor of giving the annual Hower lecture.
“I am so honored and excited to accept this award and present the associated lecture to an audience comprised of my colleagues, friends, mentors, and trainees,” said Schor.
The Child Neurology Society is the preeminent non-profit professional association of pediatric neurologists in the United States, Canada, and worldwide. Schor, the University of Rochester Medical Center’s seventh Chair of the Department of Pediatrics, joined the university in 2006.
Faculty Reflect on SMH Stroke Center Highlighted in Super Bowl Ad
Wednesday, February 1, 2017
A new ad that will premiere during the Super Bowl focuses on Strong Memorial Hospital’s Comprehensive Stroke Center. You can watch it here. We asked neurologist Curtis Benesch, M.D., M.P.H., and neurosurgeon Tarun Bhalla, M.D., Ph.D., about UR Medicine’s stroke care and what is being done to improve access for patients across the region.
What does SMH’s designation by the Joint Commission and American Heart Association/American Stroke Association as a Comprehensive Stroke Center mean?
Benesch: Designation as a Comprehensive Stroke Center indicates that our center either meets or exceeds the highest standards of care required to provide timely and comprehensive care to patients with complex cerebrovascular disease. Our site has undergone rigorous site visits and annual reviews by the Joint Commission to ensure that we satisfy all the requirements for this designation, including metrics for primary stroke care, surgical stroke care, endovascular care, critical care, longitudinal outpatient care, research, education and outreach.
How does this designation differentiate the hospital from other stroke centers?
Bhalla: All Comprehensive Stroke Centers must provide neurosurgical care, endovascular care, and neuro-critical care. These efforts are enabled in part by a well-established interdisciplinary infrastructure of exemplary stroke care (EMS, emergency medicine, nursing, therapy, and rehabilitation). Although other sites in the region may provide some of these aspects of care, UR Medicine is the only certified Comprehensive Stroke Center in Rochester, reflecting our willingness to submit to the scrutiny of external review to ensure we meet those high standards. It is not just a label but rather a public affirmation of the breadth and depth of a large multidisciplinary team of providers working together.
What is being done to extend stroke care across the health system? For example, if you are a stroke patient and you arrive at a regional hospital supported by UR Medicine, what does that mean for the care you receive?
Benesch: We support all of our regional partners with immediate availability of consultations with experts in Cerebrovascular Neurosurgery, Stroke Neurology, and Neurocritical care. These experts can help in acute treatment decisions and, with our transfer center, can facilitate transfer of patients to Strong Memorial Hospital as needed. Furthermore, we have developed a coverage model to provide 24/7 telestroke consultation to hospitals across the region in an effort to enhance acute stroke care.
Providing timely, appropriate, and comprehensive care for stroke patients requires a high level of coordination and collaboration among caregivers. What is necessary to facilitate communication, coordination, and continuity of care across the team?
Bhalla: First and foremost, the team has to believe in the concept that the more of a difference that we can make up front, the better a stroke patient will fare in the long run. The care they receive from the first 911 call to when they arrive at the hospital is only the beginning of a journey that continues through operating room, neurocritical care, and rehabilitation and is one that will determine how much function a stroke victim will ultimately recover. We all play a part, but everyone must share the same vision. Internally, it means that all the groups that represent the continuum of care must continually focus on ways to improve communication and coordination. But this also requires building awareness and education within the community. People need know how to identify the signs of stroke and EMS providers need to know what to do and where to take patients.
What does the future hold for stroke care?
Bhalla: We are committed to continuing to find creative ways to deliver the highest level of stoke care to patients where and when they need it. This includes working with community providers and partnering with EMS to leverage the resources of our Comprehensive Stroke Center to diagnose and potentially begin treatment for stroke patients even before they reach the hospital.
URMC Drug Extends Effectiveness of HIV Therapy
Monday, January 30, 2017
Major Step toward Longer-Lasting HIV Treatment
A drug developed at the University of Rochester Medical Center extends the effectiveness of multiple HIV therapies by unleashing a cell’s own protective machinery on the virus. The finding, published today in the Journal of Clinical Investigation, is an important step toward the creation of long-acting HIV drugs that could be administered once or twice per year, in contrast to current HIV treatments that must be taken daily.
The drug, called URMC-099, was developed in the laboratory of UR scientist Harris A. (“Handy”) Gelbard, M.D., Ph.D. When combined with “nanoformulated” versions of two commonly used anti-HIV drugs (also called antiretroviral drugs), URMC-099 lifts the brakes on a process called autophagy.
Normally, autophagy allows cells to get rid of intracellular “trash,” including invading viruses. In HIV infection, the virus prevents cells from turning on autophagy; one of the many tricks it uses to survive. When the brake on autophagy is lifted, cells are able to digest any virus that remains after treatment with antiretroviral therapy, leaving cells free of virus for extended periods of time.

Harris A. (“Handy”) Gelbard, M.D., Ph.D.
“This study shows that URMC-099 has the potential to reduce the frequency of HIV therapy, which would eliminate the burden of daily treatment, greatly increase compliance and help people better manage the disease,” said Gelbard, professor and director of UR’s Center for Neural Development and Disease, who has studied HIV/AIDS for the past 25 years. The finding builds on previous research that Gelbard conducted with Howard E. Gendelman, M.D., professor and chair of the Department of Pharmacology/Experimental Neuroscience at the University of Nebraska Medical Center.
The House Call of the Digital Age: Ray Dorsey to Lead URMFG’s Telemedicine Efforts
Thursday, January 19, 2017
Neither telemedicine’s increasing prominence nor URMFG’s growing commitment to it comes as a
surprise to Ray Dorsey,
M.D.
After all, he, like many other URMC faculty members, has spent the last decade building
expertise in the field. He knows its potential, believes in its future, and is ready to help us capitalize on
existing programs to ensure our group practice is embracing this technology as it increasingly transforms the
national health care landscape.
And now, he will be applying his knowledge and skills as URMFG’s Medical Director of
Telemedicine.
“This appointment reflects our commitment to new technologies and care modalities, as well as to
faculty leadership,” said Michael F. Rotondo, M.D., F.A.C.S., CEO of URMFG. “Ray and many of his colleagues have
long been on telemedicine’s cutting edge. His new role will provide a focal point for those efforts and help us
further define our telemedicine strategy, leading to better access and increased convenience for our patients,
and to an improved experience for providers.”
UR Medicine is not actively pursuing a retail telemedicine strategy—that is,
providers virtually caring for consumers through a website such as MD Live or Doc-on-Demand—for its
primary care network, Rotondo noted. However, it does want to offer telemedicine visits for existing patients
and ensure access to specialists. Like other URMC faculty, Dorsey does exactly that, providing digital
Parkinson’s care to patients worldwide—a knowledge base he can now put to work across our organization.
“For patients, it can be incredible,” said Dorsey, director of the Center for Human Experimental
Therapeutics and professor of Neurology. “They love the fact that a doctor is coming to them. It’s the house
call of the digital age. In a traditional visit, we the healthy ask the sick to come to us on our terms, whereas
telemedicine allows us to connect with the sick on their terms.”
Benefits for Patients – and Providers, Too
The impetus to develop our telemedicine presence comes from many sources, including national
trends. Some experts predict that fully 25 percent of patient care will be delivered digitally by 2020.
Meanwhile, reimbursement changes are likely to hasten telemedicine’s growth and make it more attractive to
providers.
But Dorsey articulates the main reason behind our efforts: Telemedicine is all about the
patient.
It can bring our expert care to rural areas where specialists are scarce. It can meet the
growing demand for convenient care, eliminating long drives or even allowing patients to see their doctors from
home. And it can enhance the doctor-patient relationship by allowing providers to see patients in their own
environments.
That means telemedicine serves many of our strategic goals, from becoming the
local health system of choice to improving access to care.
But telemedicine also brings concrete benefits to providers, and to our health system as a
whole. The easy access to care that it facilitates will help us as reimbursement models shift toward
outcome-based payments and population health. Digital visits can cut down on drive time for providers, as they
did for Imran Chaudhary, M.D., assistant professor of clinical medicine. He exchanged his once-a-week,
hour-and-a-half trip to Jones Memorial Hospital in Wellsville for monthly telemedicine visits, during which he
listens to patients’ hearts remotely.
Dorsey himself became involved in telemedicine when a nursing home in New Hartford asked him and
another URMC doctor to help treat 50 residents with Parkinson’s who would find it difficult or impossible to
travel for specialty care. The program—and Dorsey’s interest—grew from there.
“Our vision is to enable any New Yorker to receive care from UR Medicine,” he said. “We’ll see
what we can do to fulfill it.”
While telemedicine’s impact and effectiveness are still under study and debates on when it’s
appropriate to use are ongoing, patients consistently report higher satisfaction when we treat them on their
terms. Overcoming the barriers that prevent that from happening, from discomfort with technology to limited
Internet and broadband access, will be a big part of Dorsey’s task.
“We need to find simple solutions,” he said. “The key is to do things that have never been done
– something that’s integral to the spirit of Meliora.”
New Trial Innovation Network Offers More Opportunities for Clinical Trials
Wednesday, January 11, 2017
URMC researchers will soon be able to take advantage of a new clinical trial network offering expertise on trial design and development as well as participant recruitment and retention. Researchers can propose a clinical trial for inclusion in the Trial Innovation Network, become a participating investigator in an existing multi-site trial or request consultation on clinical trial design through the network.
The Trial Innovation Network is the result of a major new national initiative to improve the nation's research infrastructure to make clinical trials faster, better, and more efficient. According to recent estimates, it can take 12 or more years to get a new therapy from discovery, through clinical trials, and onto the market. That's a very long time -- especially for patients who could benefit from these drugs.
"The Trial Innovation Network will increase research opportunities for patients in all areas," said Robert Holloway, M.D., M.P.H., chair of Neurology and medical/faculty director of the Trial Innovation Network Hub Liaison Team at URMC. "We don't know how many trials the network will host, but there will be many - from neonatal to geriatric trials and various conditions from rare to common diseases."
Building off previous clinical trial network models that are devoted to specific diseases, the Trial Innovation Network speeds the process by connecting institutions across the U.S. to share resources, recruit more trial sites, and maximize the number and diversity of trial participants. The Trial Innovation Network is part of the Clinical and Translational Science Award (CTSA) Program and will redefine the 64 CTSA hub institutions as clinical trial expert sites.
Brain Protein Predicts Recovery Time Following Concussion
Monday, January 9, 2017
Elevated levels of the brain protein tau following a sport-related concussion are associated with a longer recovery period and delayed return to play for athletes, according to a study published in the January 6, 2017 issue of Neurology®, the medical journal of the American Academy of Neurology. The findings suggest that tau, which can be measured in the blood, may serve as a marker to help physicians determine an athlete’s readiness to return to the game.
Despite the 3.8 million sports-related concussions that occur annually in the United States, there are no objective tools to confirm when an athlete is ready to resume play. Returning to play too early, before the brain has healed, increases an athlete’s risk of long-term physical and cognitive problems, especially if he or she sustains another concussion. Currently, physicians and trainers must make return-to-play decisions based on an athlete’s subjective, self-reported symptoms and their performance on standardized tests of memory and attention.
A team led by Jessica Gill, R.N., Ph.D. of the National Institute of Nursing Research at the National Institutes of Health and Jeffrey Bazarian, M.D., M.P.H. of the University of Rochester Medical Center evaluated changes in tau in 46 Division I and III college athletes who experienced a concussion. Tau, which plays a role in the development of chronic traumatic encephalopathy or CTE, frontotemporal dementia and Alzheimer’s disease was measured in preseason blood samples and again within 6 hours following concussion using an ultra-sensitive technology that allows researchers to detect single protein molecules.
Yurcheshen receives ASMF award for sleep telemedicine
Sunday, January 8, 2017
Michael E. Yurcheshen MD, associate professor of neurology and medicine, has been granted a 2017 Focused Projects Award by the American Sleep Medicine Foundation. The award will fund a clinical trial aimed at exploring the reliability of telemedicine in evaluating patients with sleep apnea. The $20,000 award will allow Dr. Yurcheshen along with neurology, internal medicine, and psychiatry colleagues to study telemedicine for a medical condition that is both under recognized and undertreated. The results of this clinical trial are expected to lay the groundwork for a regional clinical program, and additional longitudinal sleep-telemedicine trials. Additional investigators on the grant include E. Ray Dorsey MD MBA, Carolina Marcus MD, Jonathan Marcus MD, and Wilfred Pigeon PhD.
Challenges Remain in HIV Care in Africa
Wednesday, December 21, 2016
Barriers to diagnosis and lack of access to modern medications have combined to place caregivers and HIV-positive patients in sub-Saharan Africa between a rock and a hard place. A new study shows that physicians are often forced to choose between controlling seizures, which can occur if the disease goes undiagnosed for too long, or treating the underlying HIV infection.
The study was led by Gretchen Birbeck, M.D., M.P.H., the Edward A. and Alma Vollertson Rykenboer Professor in Neurology at University of Rochester Medical Center (URMC). Birbeck also serves as director of the Epilepsy Care Team at Chikankata Hospital in rural Zambia and is an honorary lecturer at the University of Zambia.
While the study, which appears in the journal Neurology, was undertaken for the purpose of identifying risk factors for seizures in HIV-positive patients and thereby providing physicians with a blueprint for care, it has instead highlighted the difficult decisions that providers and patients must confront.
Dorsey Gives Insight to Neurology Today on Growing Support For Telemedicine
Thursday, December 8, 2016
Neurologists involved in telemedicine programs say that, despite the challenges with reimbursement, credentialing, and turf issues, they have observed more support for the approach — increasing their ability to provide care for neurologic patients who find it difficult to travel and/or who live in rural and remote areas of the country without access to specialists.
The most formidable barrier has been the federal government — the biggest single payer for health care services, neurologist Raymond Dorsey, MD, FAAN, director of the Center for Human Experimental Therapeutics at the University of Rochester Medical Center (URMC) told Neurology Today. Its Medicare payment policy does not support patient-centered care, he said.
Dr. Dorsey works with many patients with chronic, degenerative conditions that make it difficult to travel for specialty care, including Parkinson's disease and Alzheimer's disease.
Birbeck Appointed to NIH Post on Global Health
Tuesday, December 6, 2016

Dr. Gretchen Birbeck
University of Rochester Medical Center neurologist Gretchen Birbeck, M.D., M.P.H., has been chosen to serve on the Advisory Board of the National Institutes of Health's Fogarty International Center, which supports basic, clinical, and applied medical research and training for U.S. and foreign investigators working in the developing world.
Birbeck, the Edward A. and Alma Vollertsen Rykenboer Professor in Neurology, has spent the last 20 plus years studying the burden of neurological disorders and the effectiveness of health care delivery in sub-Saharan Africa. She divides her time between Rochester and projects in Africa.
Birbeck's specific interest is epilepsy and seizure disorders -- which are far more common in Africa due to higher rates of parasitic and viral infection and constitute a significant public health problem -- and the creation of scalable interventions to prevent seizures and provide better care to vulnerable populations on the continent. She is also collaborating with local academic institutions, hospitals, and government officials in Zambia, Malawi, and Uganda to develop the networks necessary to conduct clinical trials and create education and training programs for health care providers and researchers.
The Fogarty International Center funds some 400 research and training projects involving more than 100 U.S. universities. These U.S. scientists, in turn, collaborate with colleagues in numerous foreign countries, most of them in the developing world. Fogarty also convenes the best scientific minds around the world to address critical global health research problems and guide national and international global health policies.
With humor and exercise, Lawler fights Huntington's
Tuesday, October 25, 2016
Bill Lawler is behind the bar at Caverly's Irish Pub.
A retired Rochester police investigator, Lawler pours drinks as some of his former colleagues — and some current cops — wander in.
Lawler is well known here, where he proudly wears the nickname "Three-quarters." There's a reason for the nickname: Stricken with Huntington's disease, Lawler suffers from tremors that are obvious as he pours a draft from a tap or hands a glass to a customer. Often, as his hand quavers, some of the brew sloshes over the edge. Rarely does one get a beer filled to the top; hence, the nickname "Three-quarters."
There is also the nickname "Lefty," a reference to Lawler's off-balance gait. "It's not because of my politics but because I kept walking to the left," Lawler said.
Some may find the nicknames of questionable taste, but not Lawler. This is the kind of humor he was accustomed to on the police force. Sure, Lawler may have a disability, but that does not mean he is disabled by Huntington's. At Caverly's on South Avenue, where a friend has him bartend on Wednesday afternoons, Lawler gives as well as he gets when his cop buddies give him grief.
"I refuse to be pitied," Lawler said in an interview. "If anybody ever pitied me I would bite off their nose."
A former marathoner, Lawler still runs regularly, accompanied by his guide dog, Kermit, and friends or family. Winter weather does not stop him. He keeps in touch with many of his friends, and often joins them for breakfast or lunch. He accepts any new experimental treatment offered for Huntington's, even one that left him with terrible abdominal pains.
He is, for many, a lesson about how to live a life — a life slowed by a disease with no known cure, a disease that may ultimately bring his life to an end.
But that day is, for Lawler, a distant future and not one worth imagining. And his willingness to push ahead with a life of some normalcy, and to exercise almost as vigorously as he once did, seems to have its benefits: The disease is not progressing as quickly as it does with some who settle into a sedentary lifestyle.
"The fact that he continues to get out there and run, kudos to him," said Dr. Kevin Biglan, a neurologist at University of Rochester Medical Center who works closely with Lawler. "But I also think it helps" combat the disease's effects, he said.
"He does not let the disease impact him or get him down," Biglan said. "He's just going to do his thing."
Research Will Explore New Therapies for Huntington’s Disease
Wednesday, October 12, 2016
A new award from the CHDI Foundation will advance promising research that aims to slow the progression of Huntington's disease. The funding, anticipated to total more than $10.5 million over next five years, will help University of Rochester Medical Center (URMC) scientists develop a stem cell-based therapy that swaps sick brain cells for healthy ones.
The new award will go to the lab of Steve Goldman, M.D., Ph.D., the co-director of the URMC Center for Translational Neuromedicine, which has research operations in both Rochester and at the University of Copenhagen.
Huntington's is a hereditary neurodegenerative disease characterized by the loss of medium spiny neurons, a nerve cell in the brain that plays a critical role in motor control. As the disease progresses over time and more of these cells die, the result is involuntary movements, problems with coordination, and cognitive decline, depression, and often psychosis. There is currently no way to slow or modify this fatal disease.
The new award will support research that builds upon findings published by Goldman earlier this year in the journal Nature Communications showing that researchers were able to slow the progression of the disease in mice by transplanting healthy human support cells, called glial progenitor cells, into the animals' brains.
New Grants Explore Role of Brain’s “Garbage Truck” in Mini-Stokes and Trauma
Wednesday, October 5, 2016

Maiken Nedergaard, M.D., D.M.Sc.
More than $4.5 million in new grants to the lab of University of Rochester Medical Center scientist Maiken Nedergaard, M.D., D.M.Sc., underscore the important role the brain's waste disposal system may play in a range of neurological disorders. The new awards will advance understanding of how small vessel disease and traumatic brain injury can give rise to cognitive and behavioral problems.
Nedergaard and her colleagues first unveiled the brain's unique method of removing waste -- dubbed the glymphatic system -- in a paper in Science Translational Medicine in 2012. The research revealed that the brain possesses a circulation network that piggybacks on blood vessels and uses cerebral spinal fluid to flush away waste products from brain tissue. Since that time, the team has gone on to show that the glymphatic system works primarily while we sleep, could be a key player in diseases like Alzheimer's, and is disrupted after traumatic brain injury.
Burack on Panel of Experts on WXXI's Connections with Evan Dawson
Wednesday, September 28, 2016
Michelle A. Burack, M.D., Ph.D., sat in with a panel of experts on WXXI's Connections with Evan Dawson (Sept. 28) examining how—from diagnosis to research and resources—Rochester has become more welcoming to those living with Parkinson's Disease.
Neurology Celebrates 50 Years of Leadership in Research, Care, and Education
Wednesday, September 21, 2016
The University of Rochester Medical Center (URMC) Department of Neurology is honoring the 50th anniversary of its founding. The occasion will be marked with four day-long celebration of the department’s history, achievements, alumni, and vision for the future.
“The history of the department is ultimately a human story of relationships, inspiring leadership, and how a rare combination of great intellect, common sense, humility, wit, and charm can move the neurological needle on a global scale,” said Robert Holloway, M.D., M.P.H., the chair of the Department of Neurology. “From its humble beginnings 50 years ago, this department has shaped the careers of hundreds of caregivers and, through its care and research, impacted the lives of millions of patients.”
The URMC Department of Neurology was founded by Bob Joynt, M.D. in 1966 who served as its chair until 1986. The department has been subsequently led by Robert Griggs (1986-2008) Steve Goldman (2008-2012), and Holloway (2012-present).
Study Could Herald New Treatment for Muscular Dystrophy
Thursday, September 8, 2016
New research has shown that the corticosteroid deflazacort is a safe and effective treatment for Duchenne muscular dystrophy. The findings, which appear this month in the journal Neurology, could pave the way for first U.S.-approved treatment for the disease.
"Duchenne muscular dystrophy patients have limited treatment options and a desperate need for effective therapies," said University of Rochester Medical Center (URMC) neurologist Robert Griggs, M.D., lead author of the study. "This study shows that deflazacort may provide an important treatment for delaying the progression of the disease."
Duchenne muscular dystrophy (DMD) is a condition found almost exclusively in boys. The disease is characterized by muscle weakness which begins to appear at a young age and progresses rapidly leading to significant disability. Boys with the disease often end up in a wheelchair by age 9 or 10 because of weakness in their legs. The symptoms eventually spread to other parts of the body, including the heart and muscles responsible for breathing, and the disease is often fatal by the time the individual reaches his late teens. An estimated 28,000 people in the U.S. suffer from the disease.
DOD Grant Explores New Drugs to Thwart Impact of Trauma, Stroke, and Cardiac Arrest
Wednesday, September 7, 2016
A $2.3 million Department of Defense grant will help neuroscientists develop new treatments for the emergency room and the battlefield. The research will focus on the development of new therapies that could help protect brain and other at risk organs following a trauma, heart attack, or stroke.
“While we have made significant progress in our ability to restore blood flow after stroke or cardiac arrest, the medical community does not have drugs at its disposal to prevent the secondary damage that occurs after these events,” said University of Rochester Medical Center neurologist Marc Halterman, M.D., Ph.D., the principal investigator of the study. “This grant will further our research on a promising class of drugs that possess both anti-inflammatory and cytoprotective properties that we believe will be suitable for use in both military and emergency conditions.”
Jonathan W. Mink Elected President of Child Neurology Society
Tuesday, August 30, 2016
Jonathan W. Mink, M.D., Ph.D., chief of Child Neurology at Golisano Children's Hospital, will lead the nation's largest organization of child neurologists.
Mink, who is also Frederick A. Horner, MD Endowed Professor in Pediatric Neurology, was voted president of the organization by fellow pediatric neurologists from around the U.S. He will assume the position of president-elect following the annual meeting of the Child Neurology Society in November.
Mink will succeed Golisano Children’s Hospital’s pediatrician-in-chief, Nina F. Schor, Ph.D., William H. Eilinger Chair of Pediatrics.
The Child Neurology Society is a non-profit professional association of 1,300 pediatric neurologists in the United States, Canada, and worldwide who are devoted to fostering the discipline of child neurology and promoting the optimal care and welfare of children with neurological and neurodevelopmental disorders.
“It’s a tremendous honor to be elected,” Mink said. “Child neurology is a changing field. There is a real opportunity to leverage our increasing diversity to reach out to students, trainees and patients in a way that we couldn’t before.”
In addition to Mink’s clinical practice and research, he directs the Division of Child Neurology in the Department of Neurology and is associate director of the Child Neurology Residency Program. He also serves on the executive board of the International Child Neurology Association, on the board of directors of the American Neurological Association, and the executive committee of the American Academy of Pediatrics Section on Neurology. He is a member of the National Advisory Neurological Disorders and Stroke Council of the NIH, a medical advisory to the Batten Disease Support and Research Association, and is also an associate editor of Neurology. He served as chair of the Child Neurology Society’s Scientific Program Committee from 2013 to 2015, where he and Schor collaborated to plan the 2014 and 2015 Annual Meetings.
“Nina was a terrific president of the Child Neurology Society. She’s a born leader, and I have learned some lessons on how she fulfilled her duties,” Mink said. “I think it’s tremendous for the University of Rochester. When I started here, there were four child neurologists. Now there are 15, and our residency program is one of the top-rated programs nationally.”
Mink trained in Pediatrics Neurology at St. Louis Children’s Hospital. He received his M.D. and Ph.D. from Washington University.
Mink is nationally recognized as a movement disorders specialist. He’s known for his research on Tourette syndrome and understanding brain mechanisms involved in the control of movement, along with disorders that cause involuntary movement. His research also includes clinical trials that impact the function of children with movement disorders.
Mink will serve one year as president-elect, two as president, and one as past president.
Neurosurgeon Bhalla Joins Stroke Team
Tuesday, August 30, 2016
Tarun Bhalla, M.D., Ph.D., has been named director of Stroke and Cerebrovascular Services in the Department of Neurosurgery and director of Inpatient Stroke and Cerebrovascular Services at UR Medicine. Bhalla, who was also appointed assistant professor in the Departments of Neurosurgery, Neurology, and Imaging Sciences, began his position on August 1, 2016.
“Dr. Bhalla is a tremendously skilled endovascular neurosurgeon who will build upon an already strong foundation of stroke and cerebrovascular services and help guide efforts to expand and improve care across the region,” said Web Pilcher, M.D., Ph.D., chair of the Department of Neurosurgery. “We are delighted that he has agreed to join the Medical Center and our team.”
“I am honored to join UR Medicine and look forward to contributing to a team of providers that is already providing the highest level of care for victims of stroke and cerebrovascular diseases,” said Bhalla. “In stroke, time is brain, so we need to continue to focus on new ways to accelerate the process of getting patients to where they need to be and receiving the level of care necessary to achieve good outcomes.”
Bhalla joins URMC from Geisinger Medical Center in Danville, PA where he served for three years as the director of Cerebrovascular and Endovascular Neurosurgery. He received his M.D. and Ph.D. from the University of Connecticut and did his residency training, as well as a fellowship in surgical endovascular neuroradiology, at the Cleveland Clinic. His specialties include cerebrovascular and endovascular treatment for stroke, aneurysms, arteriovenous malformations (AVM), carotid/vertebral artery disease, and a chronic facial pain called trigeminal neuralgia.
Bhalla will join the UR Medicine’s Comprehensive Stroke Center. Strong Memorial Hospital is the only institution in the region designated by the Joint Commission and the American Heart Association/American Stroke Association as a Comprehensive Stroke Center. His appointment will expand the Center’s team of endovascular surgeons. In recent years, stroke care undergone a shift in care with studies showing that endovascular procedures – during which surgeons remove clots in the brain via a catheter fed through blood vessels – may result in better outcomes for some patients compared to care involving only clot busting drugs.
His appointment comes on the heels of several new investments in stroke and cerebrovascular care at Strong Memorial Hospital, including a new Hybrid Operating Room and Angio Suite designed to offer minimally invasive neurosurgical procedures, a new surgical technology to treat hemorrhages deep inside the brain, and a dedicated Neuromedicine Intensive Care Unit.
Bhalla will help lead efforts to expand stroke care, including working with community providers and emergency medical technicians to diagnose and potentially begin treatment for stroke patients before they reach the hospital.
Paciorkowski Recognized for Research in Pediatric Neurologic Disorders
Monday, August 29, 2016
 Neurologist Alexander R. Paciorkowski, M.D. is being honored by the American Neurological Association (ANA) for his research in developmental disorders. The award will be presented at the ANA's annual meeting in October 2016.
Neurologist Alexander R. Paciorkowski, M.D. is being honored by the American Neurological Association (ANA) for his research in developmental disorders. The award will be presented at the ANA's annual meeting in October 2016.
Paciorkowski 's research focuses on early life epilepsies and his research has shed new light on mechanisms of a severe form of seizure disorders -- early myoclonic encephalopathy, Ohtahara syndrome, and infantile spasms -- collectively referred to as developmental epilepsies. Specifically, Paciorkowski has identified a mutation in a gene called salt-inducible kinase 1 (SIK1), a gene previously unidentified with the disease and one which researchers believe plays a role in a chain reaction of gene and protein interactions in neurons that contribute to seizures.
"Alex is a rising star in neurogenetics and child neurology who, just four years out of fellowship, has already made major contributions to our knowledge about human neurodevelopment genetics and disorders," said Jonathon Mink, M.D., Ph.D., chief of the Division of Child Neurology and vice chair of the Department of Neurology at University of Rochester Medical Center (URMC).
Study Reveals Brain’s Finely Tuned System of Energy Supply
Monday, August 8, 2016
New research in the journal Neuron reveals how the brain is able to meet its massive energy demands with a "just in time" system that delivers oxygen that fuels nerve cells. The findings could shed light on diseases like Alzheimer's and help explain the cognitive decline that accompanies the disease.
"Our brains require a tremendous amount of energy and in order to meet this demand the flow of blood must be precisely choreographed to ensure that oxygen is being delivered where it is needed and when it is needed," said Maiken Nedergaard, M.D., D.M.Sc., co-director of the University of Rochester Center for Translational Neuromedicine and lead author of the study. "This study demonstrates that microvessels in the brain play a key role in reacting to spikes in demand and accelerating the flow of blood to respond to neuronal activity."
Steven Goldman reappointed as codirector of Center for Translational Neuromedicine, Dean Zutes Chair
Thursday, June 30, 2016
Steven Goldman, professor of neurology, has been reappointed as codirector of the Center for Translational Neuromedicine and as the Dean Zutes Chair in Biology of the Aging Brain—both through June 30, 2020. Goldman also retains his joint appointments as professor of neurosurgery and as Distinguished Professor in Neurosciences.
Goldman is interested in cell genesis and neural regeneration in the adult brain. His lab focuses on the use of stem and progenitor cells for the treatment of neurodegenerative disorders such as Huntington’s Disease, as well as for the treatment of glial diseases such as the pediatric leukodystrophies and multiple sclerosis. He has published more than 250 papers in his field—more than 100 as first or senior author—as well as 20 issued patents with more pending.
The Sleep Hack Neuroscience Says Gives Your Brain Optimal Rest
Thursday, June 30, 2016
Sleep is critical for rest and rejuvenation. A human being will actually die of sleep deprivation before starvation--it takes about two weeks to starve, but only 10 days to die if you go without sleep.
The CDC has also classified insufficient sleep as a public health concern. Those who don't get enough sleep are more likely to suffer from chronic diseases that include hypertension, diabetes, depression, obesity, and cancer.
It's thus vital to get enough shuteye, but it turns out your sleep position also has a significant impact on the quality of rest you get.
Now, a neuroscience study suggests that of all sleep positions, one is most helpful when it comes to efficiently cleaning out waste from the brain: sleeping on your side.
The study, published in the Journal of Neuroscience, used dynamic contrast-enhanced MRI to image the brain's "glymphatic pathway." This is the system by which cerebrospinal fluid filters through the brain and swaps with interstitial fluid (the fluid around all other cells in the body).
"It is interesting that the lateral [side] sleep position is already the most popular in humans and most animals--even in the wild," said University of Rochester's Maiken Nedergaard. "It appears that we have adapted the lateral sleep position to most efficiently clear our brain of the metabolic waste products that build up while we are awake."
Telemedicine Program Will Extend Parkinson’s Care across the State
Tuesday, June 14, 2016
A new program launched by neurologists at UR Medicine will expand access to care and serve as a national model for the management of Parkinson’s disease and other chronic illnesses. The Parkinson’s Disease Care, New York (PDCNY) program will be a largely virtual network providing free care to as many as 500 underserved patients across New York State.
“Providing coordinated, ongoing care to Parkinson’s patients in the traditional settings of a doctor’s office requires these individuals and their caregivers and families to travel, often long distances, and is expensive for payers and patients alike,” said URMC neurologist Kevin Biglan, M.D. M.P.H., the director of the PDCNY program. “The PDCNY program will break down the barriers of geography and deliver care directly to patients who have never seen a specialist and in the comfort of their own homes.”
Swapping Sick for Healthy Brain Cells Slows Huntington’s Disease
Tuesday, June 7, 2016

Researchers have successfully reduced the symptoms and slowed the progression of Huntington’s disease in mice using healthy human brain cells. The findings, which were published today in the journal Nature Communications, could ultimately point to a new method to treat the disease.
The research entailed implanting the animals with human glia cells derived from stem cells. One of the roles of glia, an important support cell found in the brain, is to tend to the health of neurons and the study’s findings show that replacing sick mouse glia with healthy human cells blunted the progress of the disease and rescued nerve cells at risk of death.
“The role that glia cells play in the progression of Huntington’s disease has never really been explored,” said Steve Goldman, M.D., Ph.D., co-director of the University of Rochester Center for Translational Neuromedicine. “This study shows that these cells are not only important actors in the disease, but may also hold the key to new treatment strategies.”
Neurologist confronts seizure disorders in sub-Saharan Africa
Tuesday, May 31, 2016

Birbeck has provided care for more than 3,000 patients with seizure disorders in Africa during two decades of work there. (photo courtesy of Gretchen Birkeck)
Gretchen Birbeck’s first trip to Zambia came in 1994, when she was a University of Chicago medical student completing an elective at the remote Chikankata Mission Hospital, about 75 miles south of the capital city, Lusaka.
More than two decades later, she spends half her year in sub-Saharan Africa, working to improve care for people with seizure disorders.
The Edward A. and Alma Vollertsen Rykenboer Professor in Neurology at Rochester, Birbeck is the director for Chikankata’s Epilepsy Care Team. She’s also an adjunct faculty member at the University of Zambia.
Seizure disorders can be caused by many medical conditions, and they’re more common in the developing world. Neurological and psychological disorders account “for about a quarter of the global burden of disease, and much of that is in developing countries,” says Birbeck.
“There’s a disconnect between where disease is and where experts are,” she says.
She works to redress that disconnection, providing clinical care and conducting research. As a result, more than 3,000 patients have received treatment they otherwise wouldn’t have. And she has helped make changes to Zambia’s national policy that could help many more.
She’s also working to build up the resources and networks necessary to conduct clinical trials in Africa, and to create education and training programs for health care providers and researchers. She’s involved in cerebral malaria research in Malawi and Uganda, and mentors postgraduates and junior faculty carrying out research in Zambia, Malawi, Kenya, and South Africa.
Living in the shadow of Huntington's disease
Thursday, May 26, 2016
On May 15, 2012, Manzone called his mother, Debbie Franczek, with exciting news. His wife, Danielle, was pregnant again. The joy was short-lived. Later that day, Franczek was diagnosed with Huntington's disease. It is slowly killing her.
A year before, the family started noticing changes in Franczek's mood, behaviors, speech and gait. She'd slur words as she was speaking and jerk uncontrollably. Her moods were unpredictable at best.
"We knew exactly what it was," says Manzone, who lives in upstate New York. The symptoms of Huntington's disease can be similar to those of amyotrophic lateral sclerosis, Alzheimer's and Parkinson's simultaneously. The Huntington's Disease Society of America reports that there are about 30,000 symptomatic Americans and more than 200,000 at risk of inheriting the disease today.
Kevin Biglan, professor of neurology at the University of Rochester and director of the Huntington's society's Center of Excellence, has treated patients with Huntington's disease for much of his career.
"It varies dramatically across individuals," Biglan says of the neurodegenerative disease. "Brain cells dysfunction and progressively die over a period of decades."
According to Biglan, patients with the fatal disease experience a slow progression of symptoms over a 10- to 25-year period. "You can imagine if you are 25 years old, you may not have symptoms for 25 to 30 years," Biglan says. "It can create quite a bit of anxiety among individuals. It doesn't give you much predicted value."
UR Medicine Gets Top Honors for Cardiac, Stroke Programs
Tuesday, May 24, 2016
The American Heart Association/American Stroke Association has once again honored UR Medicine’s Strong Memorial Hospital with its highest awards for heart failure, stroke and resuscitation care. Strong Memorial is the only Rochester-area hospital to earn the highest levels of recognition for these categories of care.
Strong Memorial earned Get With the Guidelines Heart Failure Gold Plus and Target Heart Failure Honor Roll Award, Stroke Gold Plus and Target Elite Plus Honor Roll Award and Resuscitation Gold Award in the AHA/ASA’s hospital-based quality improvement program.
Each year in the U.S., approximately 735,000 people suffer heart attacks, 5.7 million people endure heart failure and nearly 800,000 people suffer a stroke, according to the American Heart Association/American Stroke Association. The GWTG program is designed to measure outcomes and adherence to treatment guidelines to ensure high quality care at hospitals across the nation.
“We strive to provide the most comprehensive, leading-edge care for our patients,” said neurologist Curtis G. Benesch, M.D., M.P.H., medical director of the UR Medicine Comprehensive Stroke Center. “This award acknowledges the commitment of many individuals to the goals of advancing acute stroke care and improving stroke prevention.”
Subtle Chemical Changes in Brain Can Alter Sleep-Wake Cycle
Friday, April 29, 2016
A study out today in the journal Science sheds new light on the biological mechanisms that control the sleep-wake cycle. Specifically, it shows that a simple shift in the balance of chemicals found in the fluid that bathes and surrounds brain cells can alter the state of consciousness of animals.
The study, which focuses on a collection of ions that reside in the cerebral spinal fluid (CSF), found that not only do these changes play a key role in stimulating or dampening the activity of nerve cells, but they also appear to alter cell volume causing brain cells to shrink while we sleep, a process that facilitates the removal of waste.
"Understanding what drives arousal is essential to deciphering consciousness and the lack thereof during sleep," said Maiken Nedergaard, M.D., D.M.Sc., co-director of the University of Rochester Center for Translational Neuromedicine and lead author of the study. "We found that the transition from wakefulness to sleep is accompanied by a marked and sustained change in the concentration of key extracellular ions and the volume of the extracellular space."
The current scientific consensus is that the brain is "woken up" by a set of neurotransmitters -- which include compounds such as acetylcholine, hypocretin, histamine, serotonin, noradrenaline, and dopamine -- that originate from structures deep within the brain and the brain stem. This cocktail of chemical messengers serve to activate -- or arouse -- a set of neurons in the cerebral cortex and other parts of the brain responsible for memory, thinking, and learning, placing the brain in a state of wakefulness.
URMC Chosen for Movement Disorders Fellowship
Wednesday, April 6, 2016
URMC has been selected by The Michael J. Fox Foundation for Parkinson’s Research (MJFF) as one of six academic medical centers to host the second class of the Edmond J. Safra Fellowship in Movement Disorders.
 By increasing resources for specialized training for clinician-researcher neurologists, the program—made possible by the Edmond J. Safra Foundation—aims to grow the global base of movement disorder specialists treating people with Parkinson’s and contributing to research toward breakthrough treatments for the disease.
By increasing resources for specialized training for clinician-researcher neurologists, the program—made possible by the Edmond J. Safra Foundation—aims to grow the global base of movement disorder specialists treating people with Parkinson’s and contributing to research toward breakthrough treatments for the disease.
“There is a growing need for neurologists with additional training in movement disorders,” said Irene Richard, M.D., professor of Neurology and fellowship director at URMC. “We are honored to have been selected by The Michael J. Fox Foundation to help increase the ranks of clinician-researchers that are equipped to provide both optimal care to Parkinson’s patients and conduct the urgent work to learn more about this disease and to develop new therapies.”
URMC is one of the nation’s largest centers for Parkinson’s care and research and serves as the hub of an international network of academic, government and industry researchers searching for new ways to treat the disease.
The Medical Center is one of six centers named by MJFF to participate in the fellowship program. The others are the Icahn School of Medicine at Mount Sinai, the University of California, San Francisco, Rush University in Chicago, the University of Pennsylvania in Philadelphia; and the University of Tübingen in Germany. URMC is now recruiting a neurology resident for the 2017-2019 Edmond J. Safra Fellowship in Movement Disorders class.
“This program is designed to give people with Parkinson’s the best possible care,” said Mrs. Lily Safra, chairwoman of the Edmond J. Safra Foundation. “These prestigious institutions provide fellows with expert training in the field of movement disorders, thus increasing the number of specialty physicians available to people with Parkinson’s disease.”
MJFF and the Edmond J. Safra Foundation launched the program in late 2014 with the goal of improving the landscape of Parkinson’s care at both an individual and a population level. The clinicians trained through the Edmond J. Safra Fellowship in Movement Disorders will design and conduct studies with their patients’ unmet needs in mind. From the front lines, they are poised to observe trends and nuances of the patient experience that can lead to investigations toward greater understanding of disease and open new avenues to better therapies.
No Joke: N.J. Hospital Uses Laughing Gas To Cut Down On Opioid Use
Friday, April 1, 2016
There's a new tool for battling the opioid epidemic, compressed inside long, metal tanks at an emergency room in Paterson, N.J.
It's laughing gas, also known as nitrous oxide.
If you think this is a joke, spend a few hours with Alexis LaPietra, medical director of pain management at St. Joseph's Regional Medical Center's emergency department. She's developed an opioid-alternative program that's trying out unusual ways to help patients through their pain without using prescription painkillers in the ER, where the road to addiction began for many patients.
"The point here is not to be for or against opioids any more than it makes sense to be for or against antibiotics," says John Markman, a neurologist at the University of Rochester who specializes in pain management.
He says any ER's pain management program still has to keep opioids as an option.
"The goal is to learn to use them skillfully to minimize the public health risks because the public health risks are significant," says Markman, who's conducted research on opioids, some of which was funded by pharmaceutical companies. "There are many patients in the right context and in the right hands who can benefit."
Researchers using iPhones to collect data on Parkinson's, asthma, other ills
Sunday, March 27, 2016
Apple launched its ResearchKit program in March with five apps to investigate Parkinson's, asthma, heart disease, diabetes and breast cancer. A sixth app was released last month to collect information for a long-term health study of gays and lesbians by the University of California, San Francisco.
For scientists, a smartphone app is a relatively inexpensive way to reach thousands of people living in different settings and geographic areas. Traditional studies may only draw a few hundred participants, said Dr. Ray Dorsey, a University of Rochester neurologist who's leading the Parkinson's app study called mPower.
"Participating in clinical studies is often a burden," he explained. "You have to live near where the study's being conducted. You have to be able to take time off work and go in for frequent assessments."
Smartphones also offer the ability to collect precise readings, Dorsey added. One test in the Parkinson's study measures the speed at which participants tap their fingers in a particular sequence on the iPhone's touchscreen. Dorsey said that's more objective than a process still used in clinics, where doctors watch patients tap their fingers and assign them a numerical score.
Department of Neurology Welcomes New Residents
Wednesday, March 23, 2016
We are extremely pleased to announce the results of the 2016 neurology match. We matched another outstanding group of six individuals for adult neurology and two for child neurology as follows:
Adult Neurology – 2016 Match

Melanie Braun – University of Rochester

Ryan Canissario – SUNY Downstate Medical Center

Dimitrios (Jim) Manou – University of Rochester

Kristen McCartney – University of North Carolina

Tyler Rehbein – University of Minnesota

Nicholas Taylor – Ohio State University
Child Neurology – 2016 Match (to start in 2018)

Emily Krainer – Vanderbilt University

Justin Rosati – Hofstra North Shore – LIJ School of Medicine
Eleven UR medical students had an equally outstanding match for neurology, as follows:
Adult Neurology – 2016 Match
- Melanie Braun – University of Rochester
- Kathryn Cooper – Stony Brook Hospital
- Spencer Craven – Wake Forest Medical Center
- Robert Fuino – University of Vermont
- Adrian Hadiono – University of Texas Southwestern
- David Ivanick – University of Washington
- Dimitrios (Jim) Manou – University of Rochester
- Lauren Patrick – University of California, San Francisco
- Jason Poon – University of Utah
Child Neurology – 2016 Match
- Danielle DeCampo – Johns Hopkins Hospital
- Krista Grande – Cincinnati Children’s Hospital
New funding matchmaker will cater to NIH rejects
Wednesday, March 23, 2016
Now, a new program aims to play matchmaker between these researchers and second-chance funders. The Online Partnership to Accelerate Research (OnPAR), a collaboration between NIH and the defense, engineering, and health contractor Leidos, lets researchers upload rejected NIH proposals to an online portal where potential funders can review the scores received from reviewers, and decide whether to put up cash.
Parkinson’s App Celebrates Milestone, Featured by Apple
Monday, March 21, 2016
A Parkinson’s iPhone app developed by Sage Bionetworks and University of Rochester Medical Center (URMC) neurologists marks the first anniversary of its release. The app was also highlighted by Apple today during its semi-annual product launch event.
Sage Bionetworks, a Seattle-based nonprofit biomedical research organization, today released an updated version of its mPower (Mobile Parkinson’s Observatory for Worldwide, Evidence-based Research) app that includes an improved user interface and functionality developed in response to feedback by users. Sage also announced that mPower would be the first app incorporated into a new Apple platform called CareKit, which will turn the app into a valuable tool to help better inform patients about their symptoms and care.
The mPower app – which was created by Sage in collaboration with URMC neurologists Ray Dorsey, M.D., M.B.A., and Karl Kieburtz, M.D., M.P.H., and with the support of the Robert Wood Johnson Foundation – was first unveiled in March 2015 during Apple’s “Spring Forward” product launch event.
New Award Will Advance Muscular Dystrophy Research
Tuesday, March 8, 2016
University of Rochester Medical Center (URMC) neurologist Charles Thornton, M.D. has received a Javits Neuroscience Investigator Award from the National Institutes of Health to further his research on muscular dystrophy. The unique award provides exceptional
researchers with seven years of uninterrupted funding.
The Javits Neuroscience Investigator Award was created by the U.S. Congress in 1983 and is named in honor of former U.S. Senator Jacob Javits (NY), who was the victim of amyotrophic lateral sclerosis, a degenerative neurological disorder commonly known as Lou Gehrig's disease. The $2.3 million grant is administered by the National Institute of Neurological Disorders and Stroke and is given to scientists who have demonstrated exceptional scientific excellence and productivity
in their field.
Making progress on treating paralytic diseases is difficult and requires a dedicated team of clinicians and researchers,
said Thornton, the Saunders Family Distinguished Professor in Neuromuscular Research. To bring a team together and keep it together over the long run, you need a stable stream of financial support. This award will help us continue our work through a very important stage when new therapies are being tested and others are on the horizon.
Hope, Hype, and Wishful Thinking
Monday, February 22, 2016
In a perspective piece appearing in the journal Cell Stem Cell, URMC neurologist Steve Goldman, M.D., Ph.D., lays out the current state of affairs with respect to stem cell medicine and how close we are to new therapies for neurological disorders.
The dawn of stem cell medicine some 25 years ago was greeted with great enthusiasm, particularly by scientists who study diseases in the central nervous system (CNS). Many of the diseases found in the brain and spinal cord are degenerative in nature; meaning that over time populations of cells are lost due to genetic factors, infection, or injury. Because stem cell medicine holds the potential to repair or replace damaged or destroyed cells, scientists have considered these diseases as promising candidates for new therapies.
However, as with other emerging fields of medicine, the race to cures has turned out to be more of marathon than a sprint. While scientists have become very adept at manipulating stem and progenitor cells and understanding the complex choreography of genetic and chemical signals that instruct these cells to divide, differentiate, and proliferate, researchers are still grappling with the challenges of how to integrate new cells into the complex network of connections that comprise the human brain.
Goldman, co-director of the URMC Center for Translational Neuromedicine, takes a sweeping view of where we stand and which CNS diseases may or may not ultimately benefit from future stem cell-based therapies.
Study Details Source of Mental Problems Associated with MS
Tuesday, January 26, 2016
study out today sheds new light on multiple sclerosis (MS), specifically damage in the brain caused by the disease
that may explain the slow and continuous cognitive decline that many patients experience. The findings, which
appear in the Journal of Neuroscience, show that the brain’s immune
system is responsible for disrupting communication between nerve cells, even in parts of the brain that are not normally
considered to be primary targets of the disease.
“This study identifies for the first time a new disease mechanism in MS which causes damage to neurons independent of
the loss of white matter and demyelination that is the hallmark of the disease,” said the lead author, neurologist
Matthew Bellizzi, M.D., Ph.D., with
the Center for Neural Development and Disease at the University of
Rochester Medical Center (URMC). “This damage represents another component of the disease and one that is not
prevented by the current immunosuppressive drugs employed to treat MS.”
Strong Memorial Hospital Participating in Cannabis-Based Drug Trials
Monday, January 25, 2016
Researchers at Strong Memorial Hospital are involved in clinical trials with a drug derived from cannabis.
The Investigational New Drug is called Epidiolex, and it's different from medical marijuana available through the state's dispensaries. It's almost pure Cannabidiol, which is a chemical compound in cannabis thought to help reduce seizures.
Currently, URMC is involved in an FDA-approved double blind study to test the effectiveness of the drug, the results of which should be available in about a year.
Researchers are now planning for another study, called a Compassionate Use Study, to test the side effects of Epidiolex, and how it reacts with other medications. This study will involved children and young adults.
Doctor David Wang is leading the research at URMC, where he's an Associate Professor of Neurology and Pediatrics. He says patients age one-to-21 with severe, treatment-resistant epilepsy will be eligible to participate.
Immune System Cells Key to Maintaining Blood-Brain Barrier
Monday, January 11, 2016
New research shows that the cells responsible for protecting the brain from infection and inflammation are also responsible for repairing the system of defenses that separates the brain from the rest of the body. These findings have significant clinical implications because certain cardiovascular drugs could possibly impede the brain’s ability to repair itself after a stroke or other injury.
“This study shows that the resident immune cells of the central nervous system play a critical and previously unappreciated role in maintaining the integrity of the blood-brain barrier,” said Maiken Nedergaard, M.D., D.M.Sc., co-director of the Center for Translational Neuromedicine at the University of Rochester Medical Center (URMC) and lead author of the study. “When this barrier is breached it must be rapidly repaired in order to maintain the health of the brain and aid in recovery after an injury – a process that could be impaired by drugs that are intended to prevent this damage in the first place.”
New Drug for Periodic Paralysis has Roots in URMC Research
Monday, December 7, 2015

Robert “Berch” Griggs, M.D.
More than 15 years of research led by neurologists at the University of Rochester Medical Center (URMC) has culminated in the first approved treatment for individuals with a rare neuromuscular disorder called periodic paralysis. The U.S. Food and Drug Administration (FDA) recently approved dichlorphenamide, which is being marketed under the brand name Keveyis by Taro Pharmaceuticals, for individuals with the disease.
Periodic paralysis is extremely rare – an estimated 5,000 people in the U.S. suffer from the disease – and the condition is generally neither fatal nor life shortening, but can have a significant impact on quality of life depending upon the frequency and severity of the paralytic “attacks” that are the hallmark of the disease. Some patients can go months without an attack and may only experience limited movement in an extremity, while others experience attacks daily and can be immobilized for several hours at a time. Over time, many patients become weaker.
“This is one of the most dramatic diseases in medicine,” said Robert “Berch” Griggs, M.D., a professor in the University of Rochester Medical Center Department of Neurology and principal investigator of the clinical studies that led to the drug’s approval. “A patient can wake up in the morning and be completely paralyzed from the neck down. Over the course of hours they regain mobility so by the time they get the doctor’s office they are often completely normal.”
Griggs is an internationally recognized expert in periodic paralysis and is sought out by patients from around the world. Almost 45 years ago, Griggs first demonstrated that the drug acetazolamide was partially effective in treating periodic paralysis and, more recently, was part of a team of researchers that discovered the genetic cause of periodic paralysis. In 2003, the National Institutes of Health tapped Griggs to head a national network of physicians and scientists that are focusing on rare neurological disorders such as periodic paralysis.
URMC’s role in bringing dichlorphenamide to market began in 2000, when Griggs and his colleague Rabi Tawil, M.D. showed in a small study that dichlorphenamide was highly effective in preventing the attacks and keeping patients’ muscles strong.
Study Identifies Patients' Priorities in Treating Rare Muscular Dystrophy
Wednesday, November 18, 2015

Chad Heatwole, M.D.
A new study of individuals with myotonic dystrophy type 2 (DM2) -- a rare form of muscular dystrophy --has helped pinpoint the symptoms of the disease that are most important to patients. These findings, published today in the journal Neurology, could help create a roadmap for physicians to prioritize treatment of this complex, multi-system disease.
"This study represents the first large-scale attempt to obtain direct patient input to identify the most prevalent and life-altering symptoms of myotonic dystrophy type 2," said University of Rochester Medical Center (URMC) neurologist Chad Heatwole, M.D., the lead author of the study.
Birbeck Holds Family Feedback Meeting in Malawi
Sunday, November 1, 2015
Dr. Birbeck recently held a Family Feedback Meeting for the Family’s of Children who participated in our clinical trial of LVT for seizure control in acute cerebral malaria. The families of over 40 children came together to learn about the results of the study and our plans for future work.
Experimental Treatment Regimen Effective Against HIV
Monday, October 19, 2015
Protease inhibitors are a class of antiviral drugs that are commonly used to treat HIV, the virus that causes AIDS. Scientists at the University of Nebraska Medical Center designed a new delivery system for these drugs that, when coupled with a drug developed at the University of Rochester School of Medicine and Dentistry, rid immune cells of HIV and kept the virus in check for long periods. The results appear in the journal Nanomedicine: Nanotechnology, Biology and Medicine.
While current HIV treatments involve pills that are taken daily, the new regimens' long-lasting effects suggest that HIV treatment could be administered perhaps once or twice per year.
Nebraska researcher Howard E. Gendelman designed the investigational drug delivery system--a so--called nanoformulated
protease inhibitor. The nanoformulation process takes a drug and makes it into a crystal, like an ice cube does to water. Next, the crystal drug is placed into a fat and protein coat, similar to what is done in making a coated ice--cream bar. The coating protects the drug from being degraded by the liver and removed by the kidney.
When tested together with URMC--099, a new drug discovered in the laboratory of UR scientist Harris A. (Handy
) Gelbard M.D., Ph.D., the nanoformulated protease inhibitor completely eliminated measurable quantities of HIV. URMC--099 boosted the concentration of the nanoformulated drug in immune cells and slowed the rate at which it was eliminated, thereby prolonging its therapeutic effect.
Patients Prefer Relief from Lower Back Pain Over Improved Mobility
Friday, September 11, 2015
A new study out today in the journal Neurology examines the question of quality of life for individuals with a common form of lower back pain called lumbar spinal stenosis. The findings show that, when asked to choose between treatments that reduced pain or would help them stand or walk, patients overwhelmingly chose pain relief.
There has long been a debate in the medical community over striking the right balance between pain relief and physical function,
said John Markman, M.D., director of the Translational Pain Research Program in the University of Rochester Department of Neurosurgery and lead author of the study. While physicians have leaned toward the need to increase mobility, this study shows that patients have a clear preference for pain relief.
Menopause Infographic: Brain Fog
Tuesday, August 11, 2015
You’re in the middle of a conversation with a colleague, and lose your thought halfway through a sentence. You call your children by the dog’s name. (If you name your dog after your first born, you might save yourself some embarrassment!). Your desk is plastered with sticky note reminders. You find yourself asking your significant other, Honey, can you call my phone? I can’t find it.
You wish you could do the same with your keys and wallet.
It’s not in your head: Menopausal memory loss is real.
If a woman approaching menopause feels she is having memory problems, no one should brush it off or attribute it to a jam-packed schedule. She can find comfort in knowing that there are new research findings that support her experience. She can view her experience as normal,
lead researcher Miriam Weber, Ph.D., said in a statement. Between one-third and two-thirds of women report forgetfulness and other memory difficulties during perimenopause and menopause, according to Weber.
FDA Approves Tool for Diagnosing Dementia in a Doctor's Office
Monday, August 10, 2015

Dr. Charles Duffy
A small company started by a neuroscientist at the University of Rochester has moved closer to providing doctors with what he says is a simple,
computer-based tool to help detect early signs of Alzheimer's disease or other forms of dementia.
Cerebral Assessment Systems has received marketing approval from the
U.S. Food and Drug Administration for Cognivue, a cognitive-assessment tool that functions somewhat like a video game. A patient can perform the
inexpensive and simple test while a time-strapped primary-care physician tends to other patients. The 10-minute, non--invasive examination can detect
subtle lapses in the brain’s perceptual ability that may signal the early stages of mental decline caused by dementia.
The federal government's approval to market the device comes as Alzheimer's researchers everywhere step up the pursuit for easier and more
inexpensive ways to identify dementia in its earliest stages.
Look, there is a late-life tsunami of late-life cognitive decline coming at us, and health-care providers are standing on the beach,
said Charles J. Duffy, a neurology professor at the University of Rochester Medical Center who
founded the company. What we are all about is making cognitive care part of primary care.
Read the article from the Washington Post.
UR Medicine Honored for Stroke Care
Friday, July 24, 2015
UR Medicine’s Strong Memorial Hospital has received the American Heart Association/American Stroke Association’s (AHA/ASA) highest award for stroke care, including a new designation that recognizes excellence in rapid care that can save lives and improve the quality of life of stroke victims.
In stroke care, time equals brain,
said Curtis Benesch, M.D., medical director of the UR Medicine’s Comprehensive Stroke Center. This award recognizes the discipline and training that is required to provide appropriate and timely care to stroke patients and our team strives each and every day to provide the most comprehensive, cutting-edge care for patients from across upstate New York.
This award reflects the commitment of our team to providing the highest level of care possible for our patients who’ve suffered a stroke,
said Babak Jahromi, M.D., surgical director of the Comprehensive Stroke Center. The outstanding group of nurses, therapists, and physicians that we have assembled are dedicated to this common goal.
Strong has been named a Get With The Guidelines Stroke Gold Plus Achievement Award with Target: Stroke Honor Roll Elite Plus. The award recognizes the hospitals commitment and success ensuring that stroke patients received the most appropriate treatment according to nationally recognized, research-based guidelines based on the latest scientific evidence.
To receive the Gold Plus Quality Achievement Award, hospitals must achieve 85 percent or higher adherence to all Get With The Guidelines-Stroke achievement indicators for two or more consecutive 12-month periods and achieved 75 percent or higher compliance with five of eight Get With The Guidelines-Stroke Quality measures.
Study: Virtual Research Studies Feasible
Thursday, July 16, 2015
A new pilot study in Parkinson’s disease suggests a new era of clinical research which removes the barrier of distance for both scientists and volunteers. The research, which appears in the journal Digital Health, could also enable researchers to leverage the rapid growth in personal genetic testing to better diagnose, and potentially treat, a wide range of diseases.
These findings demonstrate that remote recruitment and conduct of research visits is feasible and well-received by participants,
said Ray Dorsey, M.D., M.B.A., a neurologist at the University of Rochester and lead author of the study. Direct-to-consumer genetic testing, when paired with telemedicine, has the potential to involve more people in clinical research and accelerate the process of identifying the genetic causes and variations in chronic diseases such as Parkinson’s.
Flaum Eye Institute Scientist Gets Funding to Study Vision Loss in Batten Disease
Thursday, July 2, 2015

Ruchira Singh, Ph.D.
University of Rochester Medical Center scientist Ruchira Singh, Ph.D., received a grant from the
Knights Templar Eye Foundation to investigate how neurodegenerative diseases,
such as juvenile Batten disease, cause blindness.
Singh, assistant professor of Ophthalmology and Biomedical Genetics, will use the $60,000
grant to create a human model of Batten disease (CNL3) using patient’s own cells. The project may lead to better understand the disease mechanisms, aiding in the
development of drug therapies to preserve vision in affected patients.
For the complete article, visit the URMC newsroom.
Mink Receives First Ever Tourette’s Association of America Award
Wednesday, July 1, 2015

Dr. Jonathan Mink
Jonathan Mink, M.D., Ph.D., chief of Child Neurology at Golisano Children’s Hospital, is the first recipient of
the Tourette Association of America’s Oliver Sacks Award for Excellence. The award, named for the famous British
neurologist, was to be presented at the First World Congress on Tourette Syndrome and Tic Disorders, but due to
a scheduling conflict, representatives from TAA instead traveled to Rochester to present him with the award in a
surprise ceremony.
The award is in recognition of his many years of leadership, mentorship, research, and care on behalf of all people
touched by Tourette syndrome and tic disorders around the world.
10th Annual Steven R. Schwid, M.D. Neurology/Neurosurgery Resident,
Fellow and Student Research Symposium
Wednesday, June 10, 2015
The Annual Steven R. Schwid Neurology/Neurosurgery Resident, Fellow and Student Research Symposium will be held this Friday, June 12th, 2015 from 9 AM – 12 pm in the Flaum Atrium. This symposium is celebrating its 10th year and the memory of former Neurology faculty member Dr. Schwid, who was a dedicated mentor for trainees and respected clinician and researcher.
The session will begin with Neurology Grand Rounds given by Dr. Benjamin Crane, MD, PhD from the Department of Otolaryngology held in the Class of 62’ auditorium. Following rounds there will be a poster session showcasing the work of the residents, and lab-based trainees from the Departments of Neurology and Neurosurgery. As in years past, we ask that faculty cast their vote for their top picks in each of two categories including Case Reports and Basic/Clinical Research. We have included a PDF version of all abstracts submitted for consideration below and paper ballots will be available at the poster session. Refreshments will be available during the poster viewing session followed by lunch served beginning at 11AM.
Please join us in recognizing the work of our trainees and departmental colleagues.
Foxe Appointed to Head Neuromedicine Research at URMC
Tuesday, June 9, 2015
 John J. Foxe, Ph.D., a
nationally-regarded scientist in the field of neurobiology, has been named the research director of the DelMonte
Neuromedicine Institute (DNI) and the Kilian J. and Caroline F. Schmitt Chair of the Department of Neurobiology and Anatomy at the University of Rochester School of Medicine and
Dentistry.
John J. Foxe, Ph.D., a
nationally-regarded scientist in the field of neurobiology, has been named the research director of the DelMonte
Neuromedicine Institute (DNI) and the Kilian J. and Caroline F. Schmitt Chair of the Department of Neurobiology and Anatomy at the University of Rochester School of Medicine and
Dentistry.
The University of Rochester has long been home to some of the nation’s most innovative and groundbreaking research
in the field of neuroscience and neuromedicine,
said Joel Seligman, president of the University of
Rochester. John’s appointment signals our determination to make this field a centerpiece of our progress as a
University and Medical Center.
I am honored to be taking the helm of the DNI at this incredibly exciting time in modern neuroscience
research,
said Foxe. The University of Rochester is already world-renowned for its superb work in this
field and we now have the opportunity to build an even stronger presence. Tens of millions of Americans suffer
from a major mental illness each year, be it depression or anxiety, a major psychotic disorder, or Alzheimer’s
disease, stroke, or addiction. And the list goes on. The National Institutes of Health estimates that only about
half of these people ever receive treatment. We can and we must do better. It is only through research that we
can develop new effective treatments and I am committed to placing the DNI and the University of Rochester at
the very forefront of these efforts.
Memorial Service Held for Neurologist Richard Satran
Thursday, May 14, 2015

Dr. Richard Satran, M.D.
A memorial service was held Thursday May 7th, at the Rochester Academy of Medicine in honor of neurologist, Dr. Richard Satran who died September 20, 2014 at the age of 86. Please view the video of the service, above.
Dr. Satran was a founding member of the department of Neurology arriving in Rochester in 1962 under the leadership of Paul Garvey. He never left and built his formidable career around patient care, teaching, and the history of neurology. He became Professor Emeritus in 1997.
From the first week I moved to Rochester in 1990 when he was my attending in resident clinic, to the very last discussions we had about health care and teaching, Dr. Satran was always a mentor to me and to many others,
said chair of Neurology, Robert G. Holloway, M.D., M.P.H.
He was a neurologist's neurologist and his passion, integrity and approach to neurology lives on in all of us. He was from the biopyschosocial era of the Medical School and was always a fierce advocate for patients and their quality of life - he taught many to always think about the broader context within which a patient's disease occurs, lessons that are more relevant today than ever
, continued Holloway.
Dr. Laurie Seltzer, D.O. and Dr. Ruth Schneider Receive 2015-2016 Pilot Project Grant
Monday, May 11, 2015

Dr. Laurie Seltzer, D.O.
The Department of Neurology is pleased to announce that Dr. Laurie Seltzer, D.O., Senior Instructor in Child Neurology and Epilepsy, and Dr. Ruth Schneider, MD, Fellow in Movement Disorders are the recipients of the 2015-2016 Department of Neurology Pilot Project Grant Program.
Dr. Seltzer's project is titled, EEG Spectral Analysis and Developmental Outcomes in Infantile Spasms
. Infantile spasms (ISS) is a devastating epileptic syndrome that affects children under 1 year of age. There are multiple and diverse genetic and extrinsic etiologies of ISS, and the syndrome is characterized by resistance to treatment and risk of poor neurodevelopmental outcome. Dr. Seltzer will study novel technologies, including EEG spectral analysis, in the evaluation of electrophysiological data in patients with infantile spasms. Her research aims are to: establish a database of infantile spasms subjects, characterize the spectral definition of hypsarrhythmia, and determine associations between these spectral patterns and response to treatment and developmental outcome. Improving EEG interpretation and diagnosis of ISS could improve rapid and effective treatment of ISS, which may meaningfully improve neurodevelopmental outcome for affected children. Dr. Seltzer's work will involve an ongoing collaboration with and mentorship by Dr. Behnaz Ghoraani, PhD, in the Department of Biomedical Engineering at Rochester Institute of Technology, and her mentors in the Department of Neurology at the University of Rochester, Dr. Gretchen Birbeck, MD and Dr. Alex Paciorkowski, MD.

Dr. Ruth Schneider, MD
Dr. Schneider's project is titled, The Impact of Telemedicine-Delivered Movement Disorder Specialist Care for Nursing Home Residents with Parkinsonism
. Patients with parkinsonism who reside in nursing homes require access to movement disorder specialists, but this may be difficult to achieve for all patients through in-person visits. Dr. Schneider's study will focus on evaluating whether access to movement disorder specialist care through telemedicine will have an effect upon short-term patient outcomes, in particular the rate of falls. The research aims are to evaluate the efficacy of telemedicine movement disorder specialist care by assessing change in fall rate and falls with major injuries; assessing change in hospitalizations; and change in functional and mental status. In this study, nursing home patients with parkinsonism will be randomly assigned to receive immediate telemedicine care or to receive it after 6 months (delayed start group); Dr. Schneider will compare outcomes between these two groups, hypothesizing that the immediate access group will demonstrate improvements in these outcome measures in comparison to the control (delayed start) group. Dr. Schneider's work will include a collaboration with two nursing homes within the Samaritan Medical Center in Watertown, NY, and her mentor in the Department of Neurology at the University of Rochester, Dr. Kevin Biglan, MD.
The Department of Neurology Pilot Project Grant Program is designed to allow junior faculty, fellows and residents the opportunity to develop and conduct pilot clinical and basic science research projects, educational programs with an evaluative component or clinical program evaluations.. The projects should allow for future development in an area of academic interest for the recipient, be integrated into a larger career development plan, and lead to future funding opportunities.
Understanding the Enemy Within that Causes Brain Damage after Cardiac Arrest
Thursday, May 7, 2015
A new $1.7 million grant will bring together a team of researchers to study – an ultimately thwart – the chain reaction that occurs in the body after cardiac arrest that can ultimately lead to brain damage and death.
“While the biological sequence of events is triggered by cardiac arrest, the death and disability associated with this event is the result of a broader systemic injury caused the initial loss of blood flow and subsequent tissue inflammation once blood circulation is restored,” said University of Rochester Medical Center neurologist Marc Halterman, M.D., Ph.D., the principal investigator of the study. In fact, it is the cumulative effect of this systemic injury on the brain, and not the heart – that ultimately leads to mortality in the disorder.
Investigating Batten Disease
Saturday, May 2, 2015
Dr. Jonathan Mink discusses Batten Disease in a recently published Research Media article.
International Innovation, published by Research Media, is the leading global dissemination resource for the wider scientific, technology and research communities, dedicated to disseminating the latest science, research and technological innovations on a global level.
URMC Start-up Takes Aim at Memory and Cognitive Problems
Thursday, April 30, 2015
Medications are available to treat many of the symptoms of neurodegenerative diseases like multiple sclerosis and Parkinson’s disease, but there is no drug or other therapy that improves the memory and cognitive problems that often plague patients. A new start-up company, built around research conducted at the University of Rochester School of Medicine and Dentistry, hopes to change that.
Camber NeuroTherapeutics Inc., founded based on discoveries made in the laboratories of Harris "Handy" A. Gelbard, M.D., Ph.D. and Stephen Dewhurst, Ph.D., plans to attack the cognitive component of neurodegenerative diseases using a completely new approach: stopping the inflammation in the brain, so-called neuroinflammation, that impairs the function of nerve cells and the vast networks they create. These neural networks allow us to store and recall memories, plan and prioritize, focus on particular tasks, and process sensory information.
Study Sheds New Light on Brain’s Source of Power
Friday, April 24, 2015
New research published today in the journal Nature Communications represents a potentially fundamental shift in our understanding of how nerve cells in the brain generate the energy needed to function. The study shows neurons are more independent than previously believed and this research has implications for a range of neurological disorders.
These findings suggest that we need to rethink the way we look at brain metabolism,
said Maiken Nedergaard, M.D., D.M.Sc., co-director of the University of Rochester Center for Translational Neuromedicine and lead author of the study. Neurons, and not the brain’s support cells, are the primary consumers of glucose and this consumption appears to correlate with brain activity.
Study Finds New Genetic Clues to Pediatric Seizure Disorders
Friday, April 3, 2015
Researchers have identified a new genetic mutation at the heart of a severe and potentially deadly seizure disorder found in infants and young children. The finding, which was reported today in the American Journal of Human Genetics, may help scientists unravel the complex biological mechanism behind these diseases.
These findings allow us to open up what was, up to this point, a black box and more fully understand the biological pathways associated with these disorders and why some individuals do not respond to treatment,
said Alex Paciorkowski, M.D., an assistant professor of Neurology at the University of Rochester Medical Center (URMC) and lead author of the study.
Once the mutation was identified, the researchers worked with neurobiologists in the lab of Marc Halterman, M.D., Ph.D. in the URMC Center for Neural Development and Disease, and were able to identify the downstream impact of the mutation, namely that it regulated another gene that has been associated with severe seizures called myocyte-specific enhancer factor 2C (MEF2C).
Ray Dorsey Honored at White House
Monday, March 23, 2015
URMC neurologist Ray Dorsey, M.D., M.P.H. was honored today at the White House as one of seven Champions of Change
who are doing extraordinary work to advocate for better treatments and a cure for individuals with Parkinson’s disease.
Dorsey, who also is director of the Center for Human Experimental Therapeutics, has been a pioneer in the application of technology to improve access to specialized care for people with Parkinson’s disease.
Dorsey has also recently worked with Sage Bionetworks to develop a new iPhone app to help researchers better understand how Parkinson’s impacts people’s daily lives. The app was highlighted by Apple when it announced its ResearchKit platform on March 9.
Read more on the White House website.
Brain Swelling Source of Malaria's Fatal Grip
Friday, March 20, 2015
Malaria is one of the world’s deadliest diseases, claiming a child’s life every minute. New research, published today in the New England Journal of Medicine, reveals why this preventable and treatable disease is often fatal.
The key to the new discovery was a technology that most people in the developed world take for granted: an MRI. In 2008, GE Healthcare provided an MRI to Queen Elizabeth Hospital in Blantyre, Malawi. Previously, the closest MRI was more than a thousand miles away.
Researchers, including URMC neuroradiologist Michael Potchen, M.D., and neurologist Gretchen Birbeck, M.D., M.P.H., studied the brain images of hundreds of children with cerebral malaria, which is fatal in 15-20 percent of cases. Birbeck divides her time between Rochester and health projects in Africa.
Talk: 'Using Technology to Transform Care'
Friday, March 20, 2015
Ray Dorsey, the David M. Levy Professor in neurology and codirector of the Center for Human Experimental Therapeutics, will present a talk on Using Technology to Transform Care
at today's Public Health Grand Rounds. The lecture runs from noon to 1 p.m. in Whipple Auditorium (2-6424), Medical Center. Assorted wraps will be available while supplies last; bring your own beverage.
Apple Highlights App with Medical Center Ties
Monday, March 9, 2015
A new iPhone mobile app which allows patients with Parkinson’s disease to track their symptoms in real time and share this information with researchers was featured by Apple executives today during the company’s semi-annual product launch event.
There is unmet demand for tools by which individuals can measure the course of their disease and receive feedback on how they’re doing,
said University of Rochester neurologist Ray Dorsey, M.D., M.B.A. To have a dedicated Parkinson’s disease app backed by research that will allow patients to engage with their care and receive feedback on their condition is amazing. To make that data in the aggregate available for research is heartening. Five years ago this would have been inconceivable.
The app, dubbed Parkinson mPower (Mobile Parkinson Observatory for Worldwide, Evidenced-based Research), was developed by Sage Bionetworks, non-profit research organization based in Seattle, in partnership with Dorsey and Karl Kieburtz, M.D., M.P.H. from the University of Rochester, and Max Little, Ph.D., a mathematician and lecturer at Aston University in the United Kingdom. mPower is available to download immediately at the Apple App Store.
Mouse Model Helps Researchers Target Deadly Brain Disease
Friday, February 13, 2015

When University researchers Steven Goldman and Maiken Nedergaard created a mouse model whose brains consisted of both animal neurons and human glia cells, their study initially focused on findings that the human cells essentially made the mice smarter.
However, they also created a powerful new platform for researchers to study human glial cells in experimental animals. And that is providing new insights into Progressive multifocal leukoencephalopathy (PML).
The study, out today in the journal Cell Stem Cell, suggests that the evolution of a subset of glia called astrocytes -- which are larger and more complex in humans than other species -- may have been one of the key events that led to the higher cognitive functions that distinguish us from other species.
For more information please visit the URMC Newsroom article.
Neuroprotection for Parkinson’s Remains Elusive
Friday, February 13, 2015
A new study appearing today in the Journal of the American Medical Association shows that creatine does not slow the progression of Parkinson’s disease. However, researchers are still committed to pursuing therapies that may help patients manage the symptoms of the disease for a longer period of time.
The study, which was led by Karl Kieburtz, M.D., director of the University of Rochester Clinical and Translational Science Institute, was halted in 2013 when it became apparent that creatine was not providing a benefit to Parkinson’s patients. While the findings are a setback, efforts are ongoing to identify a therapy that may slow the disease’s progress. Most notably STEADY-PD 3, a $23 million Phase 3 clinical trial co-led by the University of Rochester and Northwestern University, is currently underway to evaluate isradipine, a drug currently used to treat high blood pressure.
MSTP Announces 40th Anniversary Celebration!
Sunday, February 1, 2015
Edward M. Eddy
Rubin
The Medical Scientist Training Program (MSTP) is excited to announce a celebration of the 40th anniversary of the MSTP NIH training grant on Friday, October 9, 2015.
The keynote speaker will be an MSTP alumni from the Class of 1980: Edward Rubin, MD, PhD, Director, DOE Joint Genome Institute.
Edward M. Eddy
Rubin is an internationally-known geneticist and medical researcher at the Lawrence Berkeley National Laboratory in Berkeley, California, where he became head of the Genomic Sciences Division in 1998. In 2002 he assumed the directorship of the DOE Joint Genome Institute (JGI) to lead the JGI's involvement in the Human Genome Project (HGP).
For more information and schedule of events for the day, please visit the MSTP 40th Anniversary page.
Neuromedicine Intensive Care Unit Team Wins Award for Excellence
Thursday, January 29, 2015

URMC Board Chair George Hamlin presided over the recognition of the 2014 Excellence Award Winners at the Board meeting on Jan. 20. The awards, presented annually, laud the extraordinary efforts of our physicians, nurses, clinicians, and support staff. This year individuals and teams in 13 categories were recognized. Among them was the Neuromedicine Intensive Care Unit.
Implementation of nurse-led daily rounds is making a significant impact on patient care thanks to the Board Excellence Award-winning team, the Neuromedicine Intensive Care Unit. Introduced by Manjunath Markandaya, M.D., and created by nurse Catherine Gargan, RN, CNRN, the switch from physician-led rounds in the Neuromedicine ICU seemed like a natural transition. This change puts nurses, who are front-line caregivers, with the most up-to-date information on their patients in the lead during rounding. The nurse presents the patient to the residents, fellows, and physicians who are involved and often includes the pharmacist, respiratory therapist, and dietitian as well. Families are also welcome on rounds and they are grateful to be part of the process where they learn more about the care of loved ones and have an opportunity to ask questions of the entire care team. Rounds are more efficient under this new team approach and satisfaction scores for this critical care setting are higher.
The team was nominated by Associate Director of Adult Critical Care Nursing Kate Valcin and nurse leader LaShaunda Bradley. The departments of Neurology and Neurosurgery would like to extend their congratulations on this well-deserved award!
New Study Probes Link Between HIV Drugs and Vascular Disease
Monday, January 5, 2015
A new $3.8 million grant will bring together clinical and bench researchers to better understand why individuals who receive anti-retroviral treatment for HIV are at greater risk for heart disease and stroke.
“The good news is that the drugs being used to fight HIV are increasing life expectancy to normal levels,” said University of Rochester neurologist Giovanni Schifitto, M.D., one of the co-leaders of the study. “However, one of the long-term complications is that these treatments, the infection itself, or a combination of the two are increasing risk for cardiovascular and cerebrovascular disease in this population.”
Talk: Treatment Options for Headache Sufferers
Wednesday, December 17, 2014
The next Got Health?
talk Headaches: When to Get Help,
presented by Ann Ford Fricke, nurse practitioner at the Medical Center, will be held from 12:10 to 12:50 p.m. on Thursday, Dec. 18, in the Kate Gleason Auditorium of the Central Library's Bausch and Lomb Building, 115 South Ave. She will discuss headache causes, management, and treatments. The lecture is sponsored by the Center for Community Health. Parking is available in the Court Street garage, which is connected to the library.
Mice injected with human brain cells get smarter, scientists say
Tuesday, December 9, 2014
What would Stuart Little make of it? Mice have been created whose brains are half-human. As a result, the animals are smarter than their siblings. The idea is not to mimic fiction but to advance understanding of human brain diseases by studying them in whole mouse brains rather than in laboratory dishes.
The altered mice still have mouse neurons - the thinking
cells that make up around half of all their brain cells. But practically all their glial cells, the ones that support the neurons, are human.
It’s still a mouse brain, not a human brain,
says Steve Goldman of the University of Rochester Medical Center in New York. But all the non-neuronal cells are human.
Blows to Head Damage Brain's 'Garbage Truck', Accelerate Dementia
Tuesday, December 2, 2014
A new study out today in the Journal of Neuroscience shows that traumatic brain injury can disrupt the function of the brain's waste removal system. When this occurs, toxic proteins may accumulate in the brain, setting the stage for the onset of neurodegenerative diseases such as Alzheimer’s and chronic traumatic encephalopathy.
We know that traumatic brain injury early in life is a risk factor for the early development of dementia in the decades that follow,
said Maiken Nedergaard, M.D., D.M.Sc., co-director of the University of Rochester Center for Translational Neuromedicine and senior author of the article. This study shows that these injuries set into motion a cascading series of events that impair the brain's ability to clear waste, allowing proteins like tau to spread throughout the brain and eventually reach toxic levels.
The findings are the latest in a series of new insights that are fundamentally changing the way scientists understand neurological disorders. These discoveries are possible due to a study published in 2012 in which Nedergaard and her colleagues described a previously unknown system of waste removal that is unique to the brain which researchers have dubbed the glymphatic system.
2014 Shields Research Grant Recipient: Joana Osorio, MD
Friday, November 21, 2014

Joana Osorio, MD
Department of Neurology Instructor, Joana Osorio, MD has been chosen by the Child Neurology Foundation as the 2014 Shields Research Grant Recipient for her project, Cell-based therapy for Pelizaeus-Merzbacher disease
.
This research project aims to develop a cell-based treatment strategy for Pelizaeus-Merzbacher disease (PMD), a severe pediatric disorder of myelin caused by mutations in the proteolipid protein gene (PLP1). By transplanting genetically corrected cells from affected patients in a murine model of PMD, we will test their ability to rescue the phenotype and produce normal myelin. We will use induced pluripotent stem cells from patients with duplications and missense mutations in the PLP1 gene, correct the mutations by using gene-editing techniques and subsequently differentiate those to oligodendroglial fate. After intracerebral transplantation in a murine model of PMD, we will evaluate their motor performance and posteriorly the histology of engrafted cells. If this study is successful, this study will provide a proof of principle that autologous cell transplantation can be a feasible strategy for treatment of congenital disorders of myelin.
Researchers Using New Tools to Fight Brain Infection
Monday, November 17, 2014
Researchers have developed new insight into a rare but deadly brain infection, called progressive multifocal leukoencephalopathy (PML). This disease – which is caused by the JC virus – is most frequently found in people with suppressed immune systems and, until now, scientists have had no effective way to study it or test new treatments.
The JC virus is an example of an infection that specifically targets glia, the brain’s support cells,
said neurologist Steve Goldman, M.D., Ph.D., co-director of University of Rochester Center for Translational Neuromedicine and senior author of the paper. Because this virus only infects human glia and not brain cells in other species, it has eluded our efforts to better understand this disease. To get around this problem, we have developed a new mouse model that allows us to study human glia in live animals.
The new discovery – which appears today in the Journal of Clinical Investigation – was the result of research using a new tool developed at the University of Rochester. Last year, Goldman and Maiken Nedergaard, M.D., D.M.Sc., reported that they had created a mouse model whose brains consisted of both animal neurons and human glia cells. While the previous study focused on the fact that the human cells essentially made the mice smarter, at the same time it created a powerful new platform for researchers to study human glial cells in live adult animals, including diseases that impact these cells.
New Neurovascular Ultrasound Laboratory a Success
Saturday, November 8, 2014

Christina Clary and Dr. Holmquist
Through determination and teamwork with Neurosurgery and Imaging Sciences, the Department of Neurology’s vision of
having a dedicated Neurovascular Laboratory has been realized. The laboratory performs carotid ultrasounds on
patient's with suspected cerebrovascular disease. Since opening this past July, we have already performed over fifty
studies. The neurovascular laboratory will play an integral role in our department's mission of providing
comprehensive neurovascular care to our region and ultrasound education to our residents, students and fellows. Our
upcoming plans involve performing transcranial dopplers. I would like to take this time to especially thank Christy
Clary, Christy Miller, and Dr. Benesch for their time and effort to help make this happen.
The neurovascular laboratory is located at 2180 South Clinton Avenue, the site of the Comprehensive Stroke Center
clinic. Studies can be ordered through eRecord and by contacting Melissa Mack or Christina Holloway at 275-2530.
- Todd Holmquist, M.D.
PharmAdva Joins START-UP NY
Wednesday, October 22, 2014
PharmAdva, a medical device manufacturer, has been approved to participate in the START-UP NY economic development program. The company, which will locate in High Tech Rochester's Lennox Tech Enterprise Center in Henrietta, is commercializing a technology developed at the Medical Center by Michel Berg, associate professor of neurology and medical director of the Strong Epilepsy Center.
Józefowicz Honored for Serving Polish University
Thursday, October 16, 2014

Ralph Józefowicz, M.D. (left)
Ralph Józefowicz, professor of neurology, received the Merentibus Medal from Jagiellonian University, central Europe's second-oldest university, on Wednesday, Oct. 1, in Krakow, Poland. The medal is awarded each year for great services rendered to the Jagiellonian University.
Józefowicz established a medical exchange program between Jagiellonian University Medical College and the School of Medicine and Dentistry. Since the program’s inception in 1995, 111 Rochester medical students and 58 neurology residents have taught neurology in Krakow, and 170 Jagiellonian students have participated in clinical electives at Rochester.
A Reflection on the Increasing Importance of Private Capital in Medical Research
Wednesday, October 15, 2014
Private philanthropic foundations are emerging as a revolutionary source of innovative medical research and development funds. Though the amount of private philanthropic donations as a percentage of medical research spending, is still at a nascent stage, the reality of stagnating federal and state contributions to research and development enterprises is indicative of the future impact that private dollars may have on the field.
Funding for a disease is often scarce when the condition only affects a small portion of the population, or is considered to be less severe than other diseases in its class. Philanthropic medical research donations can target and drive medical advancements in these fields or with these diseases which are relatively neglected.
For example, Michael Goldberg, founding partner at the personal injury law firm Goldberg Weisman Cairo, and his family started the Goldberg Nathan Myotonic Dystrophy Type 2 Fund to encourage medical research into myotonic dystrophy type 2 (a rare genetic disorder characterized by muscular dystrophy).
The Goldberg endowment donated $1.25 million gift to the University of Rochester School of Medicine and Dentistry. The gift will be used to establish a center that will specifically study myotonic dystrophy type 2. Donations from private individuals who have loved ones or family members afflicted with rare genetic conditions are invaluable.
read more ...
URMC Tourette Center Named Tourette Syndrome Association Center of Excellence
Wednesday, October 8, 2014
The national Tourette Syndrome Association today announced the designation of 10 Tourette Syndrome Association
Centers of Excellence
at premier healthcare facilities, research centers and academic institutions located
across the United States.
Among them was the Tourette Center (affiliated with the Child Neurology division) here at URMC, headed by
unit chief, Jonathan Mink, M.D., Ph.D.
The designation of Tourette Syndrome Association Centers of Excellence in communities across the country,
particularly in underserved areas, is crucial to our mission,
said Annetta Hewko, President of the Tourette
Syndrome Association. Today, there is no standard model of care for Tourette's or Tic Disorders. Our aim is to
partner with the Centers of Excellence to set these standards and increase access to informed, evidence-based
treatment, compassionate care and guidance. We are genuinely excited to launch this initiative. It can significantly
impact our mission to serve to all people affected by Tourette’s and Tic Disorders.
The newly designated Centers will be the catalysts for cutting-edge scientific and clinical research aimed at
decreasing diagnostic variability, deciphering the cause(s) and improving treatment of both tic and non-tic
features. The Centers will also lead the way in training the next generation of experts in TS and Tic Disorders,
said Dr. Kevin St.P. McNaught, the Tourette Syndrome Association's Vice President for Medical and Scientific Programs.
read the
entire press release ...
Research Seeks to Break New Ground in Understanding of Schizophrenia
Tuesday, September 30, 2014
More than $6 million in funding from the National Institute of Mental Health (NIMH) is supporting new research that
could fundamentally alter the way we comprehend and, perhaps ultimately, treat schizophrenia.
The research - which is being led by University of Rochester Center for Translational
Neuromedicine co-directors Steve Goldman, M.D., Ph.D., and Maiken Nedergaard, M.D., D.M.Sc. - will explore
the role that support cells found in the brain, called glia, play in the disease.
The new research is possible because of findings published by Goldman and
Nedergaard last year that showed that glial cells play an important role in the complex signaling activity that
is unique to the human brain. In these experiments the researchers showed that when human glial cells were implanted
into the brains of newborn mice the human cells influenced communication within the animals' brains, allowing the mice
to learn more rapidly.
Moxley and Thornton Honored for Myotonic Dystrophy Research
Monday, September 22, 2014

Richard Moxley

Charles Thornton
University of Rochester neurologists Richard Moxley, M.D., and Charles Thornton, M.D., have been recognized by the Myotonic Dystrophy Foundation (MDF) with an Outstanding Research Achievement Award. The event took place at the U.S. Capitol earlier this month and honored their contribution to finding new treatments for myotonic dystrophy.
"This award is in recognition of the enduring and transformative collaboration that Drs. Moxley and Thornton have carried out in myotonic dystrophy research and clinical care, and the truly outstanding progress they have made possible in the search for treatments and a cure for the disease," said Molly White, executive director of MDF.
This recognition follows on the heels of a $7 million grant from the National Institute of Neurological Disorders and Stroke (NINDS) to renew funding for the University's Senator Paul D. Wellstone Muscular Dystrophy Cooperative Research Center, a designation that dates back to 2003. The team is also preparing -- in collaboration with Isis Pharmaceuticals -- to begin testing the first targeted treatment for the disease.
This research has brought scientists to the threshold of a potential new therapy that could reverse the genetic cause of DM1. Partnering with Isis Pharmaceuticals, the Rochester team developed a synthetic molecule -- called an antisense oligonucleotide -- that mimics a segment of the genetic code. In a study appearing in the journal Nature in 2012, Thornton and his colleagues showed that, when injected into mice with myotonic dystrophy, these molecules improved function. Isis Pharmaceuticals has recently completed Phase 1 testing and will soon advance to testing in people with the disease.
Read More: Moxley and Thornton Honored for Myotonic Dystrophy ResearchDr. Richard Satran, Founding Member of the Department of Neurology Dies
Monday, September 22, 2014

Dr. Richard Satran, M.D.
It is with a sad heart the department of Neurology announces that Dr. Richard Satran died Saturday morning.
Dr. Satran was a founding member of the department of Neurology arriving in Rochester in 1962 under the leadership of Paul Garvey. He never left and built his formidable career around patient care, teaching, and the history of neurology. He became Professor Emeritus in 1997.
From the first week I moved to Rochester in 1990 when he was my attending in resident clinic, to the very last discussions we had about health care and teaching, Dr. Satran was always a mentor to me and to many others,
said chair of Neurology, Robert G. Holloway, M.D., M.P.H.
He was a neurologist's neurologist and his passion, integrity and approach to neurology lives on in all of us. He was from the biopyschosocial era of the Medical School and was always a fierce advocate for patients and their quality of life - he taught many to always think about the broader context within which a patient's disease occurs, lessons that are more relevant today than ever
, continued Holloway.
We extend our deepest condolence to Rick's wife, Hilda and his entire family. He will be deeply missed. View Dr. Satran's obituary.
Gift Will Advance Research on Myotonic Dystrophy Type 2
Tuesday, September 9, 2014
A $1.25 million gift from Lilyan (Lil) and Albert (Alfy) Nathan of Florida and Michael and Sherry Goldberg of Chicago will create a new center dedicated to research on myotonic dystrophy type 2 (DM2) at the University of Rochester School of Medicine and Dentistry. The gift will be used to support a new research program that will be led by UR Medicine neurologist Chad Heatwole, M.D.
We are deeply grateful to the Nathan and Goldberg families for their extreme generosity,
said Robert Holloway, M.D., M.P.H., the chair of Department of Neurology and the Edward A. and Alma Vollertsen Rykenboer Chair in Neurophysiology. Due to the efforts of Chad Heatwole, Richard Moxley, Charles Thornton, and many others here in Rochester, we believe that new therapies for this disease are on the horizon. This gift will help accelerate these efforts.
Myotonic dystrophy has been characterized as one of the most diverse genetic diseases with a wide range of symptoms ranging from fatigue, muscle stiffness, muscle weakness, cognitive impairment, depression, difficulty sleeping, impaired vision, pain, difficulty swallowing, and gastrointestinal problems. The severity and onset of these symptoms vary from patient to patient.
Dr. Heatwole gave us the first glimmer of hope that someone was actually interested in helping people with this disease,
said Michael Goldberg, founding partner of the Chicago firm Goldberg Weisman Cairo. While our family had never made a major donation to a charity or medical institution before, we believed in Dr. Heatwole, the University of Rochester, and in the importance of helping find a cure for DM2 for our son and for the untold number of other people afflicted with this disease.
Researchers Identify Rare Neuromuscular Disease
Thursday, September 4, 2014
An international team of researchers has identified a new inherited neuromuscular disorder. The rare condition is the result of a genetic mutation that interferes with the communication between nerves and muscles, resulting in impaired muscle control.
The new disease was diagnosed in two families -- one in the U.S. and the other in Great Britain - and afflicts multiple generations. The discovery was published today in the American Journal of Human Genetics.
This discovery gives us new insight into the mechanisms of diseases that are caused by a breakdown in neuromuscular signal transmission,
said David Herrmann, M.B.B.Ch., a professor in the Department of Neurology at the University of Rochester School of Medicine and Dentistry and co-lead author of the study. It is our hope that these findings will help identify new targets for therapies that can eventually be used to treat these diseases.
Researchers Receive $3.4 million to Study Experimental Drug Combination in HIV
Thursday, August 28, 2014
Researchers at the University of Rochester Medical Center and University of Nebraska Medical Center have received a $3.4 million grant from the National Institutes of Health to study an experimental drug combination that appears to rid white blood cells of HIV and keep the infection in check for long periods. While current HIV treatments involve pills that are taken daily, the experimental drugs’ long-lasting effects suggest the possibility of an HIV treatment that could be administered monthly, or perhaps a few times a year.
Stem Cell Therapies Hold Promise, But Obstacles Remain
Thursday, August 21, 2014
In an article appearing online today in the journal Science, a group of researchers, including University of Rochester neurologist Steve Goldman, M.D., Ph.D., review the potential and challenges facing the scientific community as therapies involving stem cells move closer to reality.
The review article focuses on pluripotent stem cells (PSCs), which are stem cells that can give rise to all cell types. These include both embryonic stem cells, and those derived from mature cells that have been reprogrammed
or induced
- a process typically involving a patient's own skin cells -- so that they possess the characteristics of stem cells found at the earliest stage of development. These cells can then be differentiated, through careful manipulation of chemical and genetic signaling, to become virtually any cell type found in the body.
The article addresses the current state of efforts to apply PSCs to treat a number of diseases, including diabetes, liver disease, and heart disease. Goldman, a distinguished professor and co-director of the University of Rochester School of Medicine and Dentistry Center for Translational Neuromedicine, reviewed the current state of therapies for neurological diseases.
Suburban Outlaw: Total (Lack of) Recall
Monday, August 18, 2014
Mark Mapstone, an associate professor of neurology, says the best thing people can do for their brains as they age is to take care of their physical health.
Mapstone explained that we remember stories from our past so well because we've practiced remembering them by calling them up over the years and sharing them with others. Recent memories aren't as sticky for a lot of reasons, including how well we pay attention in the moment and even how much stress we have in our lives. So, in addition to eating right and exercise to cultivate a better memory, Dr. Mapstone advises something simple: Pay attention. What a concept.
Dr. Jonathan Mink Appears on ABC’s 20/20 to Discuss Tourette Syndrome in Athletes
Friday, August 15, 2014
Jonathan Mink, M.D., Ph.D., Frederick A. Horner, MD Endowed Professor in Pediatric Neurology, appeared on ABC's 20/20 on August 15the to discuss Tourette Syndrome in athletes and whether it gives them an advantage. Mink, who specializes in Tourette syndrome and other movement disorders at the University of Rochester, and is the co-chair of the National Tourette Syndrome Association's scientific advisory board, is more skeptical, citing conflicting studies. He said the science isn't there yet to definitively prove that Tourette's can help give athletes with the condition superior skills or make, say, a basketball player the next Lebron James.
The studies that have been done of people where actually measuring their movements, measuring how fast their movements are and the reaction times show that on average, people with Tourette Syndrome are about the same as people without,
Mink said.
Parkinson's Disease May Worsen Depression
Friday, August 15, 2014
A push from Parkinson’s disease could have put Robin Williams at risk of a perfect storm
of depression, medical experts said Thursday.
Although the disease is best known for its deleterious effects on the nerve cells that produce dopamine, a neurotransmitter that facilitates movement, Parkinson’s also affects a host of other chemical messengers, including serotonin and norepinephrine, which may explain why patients are more likely to develop depression.
The good news is that Parkinson’s-related depression responds well to currently available antidepressants that pump up the amount of serotonin and norepinephrine circulating in the brain, said Dr. Irene Richard, a professor of neurology and psychiatry at the University of Rochester Medical Center and a science adviser to the Michael J. Fox Foundation for Parkinson’s Research.
The bad news: Often doctors and even patients themselves do not recognize the depression. It’s just too easy to say that the patient is down because of the diagnosis, Richard said. Further, Parkinson’s and depression have overlapping symptoms, such as a blank facial expression and a monotone voice, she explained.
University Doctor to Cycle Across the U.S. for ALS
Thursday, August 14, 2014
Neurology's own Carly LaVigne (URMC Headache Center) is cycling across the USA in honor of her mother, Sally Hanan Oliver, who died of ALS at the age of 42. She will start her trip on August 24th in Astoria Oregon finishing 45 days later in Portland Maine. You can follow her progress at her 'Cycling for Sally' blog that Carly will keep throughout her journey. All proceeds raised will go to patient care services and support programs for the ALS clinic within our Division of Neuromuscular Disease.
UR Medicine Opens Doors on New NeuroMedicine ICU
Monday, July 28, 2014
UR Medicine today unveiled a new state-of-the-art unit dedicated to highly specialized care for people with serious and life-threatening neurological conditions, like strokes, seizures, brain and spinal tumors, and traumatic brain injury. The Neuromedicine Intensive Care Unit (ICU), which is the only unit of its kind in the region, is located on the eighth floor of Strong Memorial Hospital.
The $5.5 million, 5,500-square-foot unit consists of 12 beds and is staffed around the clock by an extended multidisciplinary team trained to treat the most challenging and difficult neurological disorders. The neurocritical care team members include neurointensivists, neurologists, neurosurgeons, physician assistants, nurse practitioners, critical care nurses, anesthesiologists, respiratory therapists, social workers, physical therapists, speech-language pathologists, occupational therapists, nutritionists, and clinical pharmacologists.
Diseases and injuries that impact the brain and central nervous system have a unique set of challenges and require expertise that is not commonly found in a traditional ICU setting. While brain function must be continuously monitored, providers also need to be trained to recognize that these conditions can potentially lead to other problems, such as cardiovascular, kidney, and respiratory complications or infections, particularly if a patient remains in an ICU setting for a long period of time. Also, once a patient has been stabilized, there must be continuity of care as they begin the process of recovery and transition to rehabilitation.
How Do You Identify Migraine Triggers?
Sunday, June 15, 2014
Do you know when a migraine is about to happen? Some are still trying to figure out what triggers a migraine since everyone is different. There are common triggers, which could be causing your migraines. Evan Dawson talked with Dr. Catherine LaVigne about these triggers and what you can do to find out what triggers your migraines. Dr. LaVigne is the former director of the URMC Headache Center, which is dedicated to providing the highest level of care for people who suffer from chronic headache disorders.
Profile of Excellence: Bob Holloway
Friday, June 13, 2014

Robert G. Holloway, M.D., M.P.H.
The 2013 Joynt Kindness Board Excellence Award in the Physician category is presented to Robert G. Holloway, M.D., M.P.H., the Edward A. and Alma Vollertsen Rykenboer Chair in Neurophysiology and Chair of the Department of Neurology.
Mark B. Taubman, M.D., dean of the URMC School of Medicine and Dentistry, calls Holloway the epitome of the academic 'triple threat.'
For his teaching excellence, Holloway has been recognized by his colleagues and students on numerous occasions. His role with the Clinical and Translation Science Institute, leadership of a NIH-funded research network for neurological disorders, and his authorship of numerous papers in publications like the New England Journal of Medicine and JAMA are testaments to his scientific contributions.
Holloway is also a true apostle of the principles of patient- and family-centered care, and it's for these principles that he is recognized with this award. He considers himself a general neurologist with broad interests in those serious neurological disorders that can greatly impact longevity and quality of life, including stroke, Parkinson's disease, dementia, multiple sclerosis, and epilepsy.
You can read the entire article here.
University Mourns the Loss of Nancy Benjamin
Friday, June 13, 2014

Nancy Benjamin (1960-2014)
University flags will be lowered June 19 in memory of Nancy Benjamin, administrative assistant in the Department of Neurology. Nancy joined the University staff in 1996. Her obituary appeared in the Democrat and Chronicle.
Nancy Benjamin died on May 31 at the age of 54 following a courageous struggle with metastatic cancer. She was my secretary, assistant and friend since 1996. Nancy was devoted to her work in our department and at the University. She ran the neurology clerkship and was instrumental in its becoming the best clinical clerkship at URSMD. She was always available to help Clara Vigelette with any resident related issues. She loved the residents and the medical students with whom she interacted. She always had a smile and enjoyed a good laugh.
Despite her medical problems, she came to work every day with a can-do attitude and refused to give in to her disease.
Nancy loved her children, Morgan and Adam, and was always so proud of them. She was a devoted daughter and was always there for her mother. She was a friend to so many staff at the University and was always willing to help out when asked.
Nancy was a very modest person and did not like any fuss. In place of a memorial service, she was remembered by her friends and family at a Happy Hour at McGinnity's Restaurant in Rochester last Friday. Nancy would have been so happy seeing all of her friends enjoying a beer in her memory.
Nancy touched the lives of everyone with whom she interacted. She was a gem of a person with a sincere devotion to her family, her friends, and her work. She will be terribly missed.
-Ralph F Józefowicz, MD
Medical Scientist Training Program Announces Leadership Changes
Sunday, May 18, 2014
The Medical Scientist Training Program (MSTP) in the School of Medicine will be undergoing leadership changes effective 7/1/14 with Marc Halterman, MD, PhD taking on the position of Associate Director.

Marc Halterman, MD, PhD
Douglas Turner, PhD, who has served the Program in many capacities since 1989, will be stepping down from his current position as Associate Director to take a well-deserved sabbatical. MSTP Director, Kerry O'Banion, MD, PhD commented, I am deeply indebted to Doug Turner for providing support and encouragement to me when I became Co-Director in 2000, and for his continued role as a key member of the MSTP Admissions Committee, thesis advisor, grant reviewer, and a clear example of the close relationship between the College and the Medical School. Notably, Doug has mentored six MSTP students in his laboratory. I wish him much success as he ventures into new areas of research inquiry.

Douglas Turner, PhD
Stepping into the MSTP Associate Director position on 7/1/14 will be Marc Halterman, MD, PhD. Dr. Halterman graduated from the MSTP at Rochester in 2002 and went on to complete a Neurology Residency and Research Fellowship at University of Rochester. He is now Associate Professor of Neurology and Pediatrics, and Director of the Neurology Academic Research Track, a research residency training program at University of Rochester. In addition, he serves on an NIH review panel for predoctoral NRSA (F) grants. Dr. Halterman has already generously given of his time serving the MSTP in several capacities. Since September 2011 he has acted as Course Director of MSTP-specific course Scientific Reasoning in Medicine. He joined the MSTP Admissions Committee in 2013 and is thesis advisor to one MSTP trainee conducting her PhD research in his laboratory. Dr. Halterman has also provided individual training and career advice to many MSTP students. As Associate Director, he will continue to be engaged in all of these activities and take on a broader role in helping trainees consider their options for research and residency selection. He will continue to serve as a member of the MSTP Admissions Committee and assist Dr. O'Banion in running an F30 Grant Writing Workshop for MSTP students.
Dr. O'Banion continued, I very much look forward to working with Marc Halterman as we enter a new five-year funded cycle of the MSTP training grant and prepare for the 40th anniversary celebration of MSTP funding in October, 2015.
The Doctor's in-Through Webcam, Smartphone
Tuesday, May 13, 2014
Mark Matulaitis holds out his arms so the Parkinson's specialist can check his tremors. But this is no doctor's office: Matulaitis sits in his rural Maryland home as a neurologist a few hundred miles away examines him via the camera in his laptop.
Welcome to the virtual house call, the latest twist on telemedicine. It's increasingly getting attention as a way to conveniently diagnose simple maladies, such as whether that runny nose and cough is a cold or the flu. One company even offers a smartphone app that lets tech-savvy consumers connect to a doctor for $49 a visit.
Why can't we provide care to people wherever they are?
asks Dr. Ray Dorsey, a neurologist at the University of Rochester Medical Center who is leading a national study of video visits for Parkinson's patients and sees broader appeal. Think of taking your mom with Alzheimer's to a big urban medical center. Just getting through the parking lot they're disoriented,
he adds. That's the standard of care but is it what we should be doing?
Drug Improves Vision in Individuals with Neurological Disorder
Tuesday, April 22, 2014
The drug acetazolamide, combined with a low-sodium weight reduction diet, improves vision in individuals with idiopathic intracranial hypertension (IIH), a condition brought about by abnormal pressure on the brain that is not the result of a tumor or other diseases.
he study, which appears this week in the journal JAMA, was coordinated by Karl Kieburtz, M.D. and Michael McDermott, Ph.D. with the University of Rochester's Center for Human Experimental Therapeutics (CHET) and also involved Steven Feldon, M.D. with the Flaum Eye Institute.
Global Burden of Neurological Diseases Requires New Approaches
Tuesday, April 22, 2014
A perspective piece appearing today in the journal JAMA focuses on the challenges and opportunities arising from the increasing global incidence of neurological disorders. The authors advocate for new approaches that will increase access, lower costs, influence lifestyle changes, and create international research and clinical partnerships that address overlooked neurological conditions and underserved global populations.
The piece is authored by University of Rochester School of Medicine and Dentistry neurologists Gretchen Birbeck, M.D. and Robert Griggs, M.D., and Michael Hanna, M.D. with University College London. Birbeck is also member of the Epilepsy Care Team at Chikankata Hospital in Mazabuka, Zambia.
Heart/Stroke Association Honors UR Medicine for Highest Quality Care
Tuesday, April 22, 2014
The American Heart Association/American Stroke Association (AHA/ASA) has once again recognized UR Medicine and its Strong Memorial Hospital for achieving its highest standards of care for stroke, heart failure, and resuscitation.
Strong Memorial Hospital has received the AHA/ASA Get With The Guidelines program’s highest honor, the Stroke Gold Plus Quality Achievement Award for a fifth consecutive year. The hospital was also tapped for the Target: Stroke Honor Roll, which recognizes hospitals that have consistently and successfully reduced door-to-needle time – the window of time between a stroke victim’s arrival at the hospital, the diagnosis of an acute ischemic stroke, and the administration of the clot-busting drug tPA.
“We are proud to earn this recognition, however we continue to work to improve time-to-treatment for people who are suffering a stroke. Early treatment is proven to preserve brain function and enhance recovery for each patient,” said neurologist Curtis Benesch, M.D., M.P.H., medical director of the UR Medicine Comprehensive Stroke Center.
Researchers Set to Launch Phase 3 Trial for Parkinson’s
Wednesday, April 2, 2014
A $23 million grant from the National Institutes of Health will support a new Phase 3 clinical trial to evaluate the drug isradipine as a potential new treatment for Parkinson’s disease. The study is being co-lead by the University of Rochester and Northwestern University.
Isradipine has been demonstrated to be safe and tolerable in patients with Parkinson’s disease,
said University of Rochester School of Medicine and Dentistry neurologist Kevin Biglan, M.D., M.P.H., co-principal investigator of the study. This new study will determine whether the drug can be an effective tool in slowing the progression of the disease and could, thereby, complement existing symptomatic treatments and improve the quality of life of individuals with the disease.
UR Medicine Helps Forge National Stroke Care Guidelines
Friday, March 28, 2014
A new statement from the American Heart Association (AHA) recommends that people recovering from a severe stroke receive tailored and coordinated care that optimizes quality of life and minimizes suffering. The statement -- which was published today in the journal Stroke -- represents the first attempt to establish a fundamental set of recommendations that can help guide physicians, patients, and their families through the difficult decisions that arise from this condition.
The majority of stroke patients require access to some form of palliative care,
said Robert Holloway, M.D., M.P.H., the chair of the Department of Neurology at the University of Rochester School of Medicine and Dentistry. Accomplishing this requires that a hospital's system of stroke care and its team of providers place the patient and their family at the center of the decision-making process and build a plan of care that is based on their values and informed by effective and constant communication.
Stroke Survivors Deserve Team Care
Thursday, March 27, 2014
Palliative care that minimizes suffering and improves quality of life should be provided to patients who've survived
a stroke, experts say. The care should be a team effort involving patients, families, stroke specialists and health
care providers such as neurosurgeons, neurologists, primary care doctors, nurses and therapists, according to the
new scientific statement from the American Heart Association (AHA) and American Stroke Association (ASA).
The majority of stroke patients need access to some form of palliative medicine,
statement lead author Dr. Robert Holloway, chairman of the neurology department at the University of Rochester Medical Center in Rochester,
N.Y., said in an AHA/ASA news release.
The stroke team and its members can manage many of the palliative care problems themselves. It encourages
patient independence and informed choices,
he explained.
Biomarker Points to Alzheimer’s Risk
Monday, March 10, 2014
A study involving Rochester-area seniors has yielded the first accurate blood test that can predict who is at risk for developing Alzheimer’s disease. This discovery – which appears today in the journal Nature Medicine – could be the key to unlocking a new generation of treatments that seek to head off the disease before neurological damage becomes irreversible.
The biomarker – which consists of 10 specific lipids found in blood plasma – predicted with greater than 90 percent accuracy which individuals would go on to develop Alzheimer’s disease or a precursor condition known as amnestic mild cognitive impairment (aMCI). The cost of the simple blood test required to detect these lipids is a fraction of other techniques and, unlike alternatives, it identifies risk early in the disease process before cognitive symptoms appears.
The ability to identify individuals who are at risk of developing Alzheimer’s before the clinical manifestation of cognitive impairment has long been a Holy Grail of the neuromedicine community,
said Mark Mapstone, Ph.D., a neuropsychologist with the University of Rochester School of Medicine and Dentistry and lead author of the study. Current efforts to develop a treatment for this disease are coming up short because they are probably being used too late. Biomarkers that can allow us to intervene early in the course of the disease could be a game-changer.
Dr. Laurie Seltzer Receives Award from Journal of Pediatric Neurology for the 2013 Best Paper
Wednesday, February 26, 2014
The Department of Neurology is pleased and proud to announce that Dr. Laurie Seltzer, DO, Senior Instructor of Child Neurology and Epilepsy recently received an award from the editors of Pediatric Neurology for the best paper submitted in 2013 by a resident or fellow. The paper, Intraoperative EEG Predicts Postoperative Seizures in Infants with Congenital Heart Disease was published online on December 23rd 2013 and will also appear in a forthcoming print issue of the journal. The research was supported in part by a NIH Institutional Research and Academic Career Development Award (K12 NS 066098).
In this prospective, observational study, Dr. Seltzer and her co-investigators reviewed preoperative, intraoperative and postoperative EEG of 32 infants who underwent cardiac surgery. Among 17 of the children, the surgery involved deep hypothermic circulatory arrest (DHCA). Specific intraoperative EEG patterns seen in two patients undergoing prolonged DHCA were predictive of postoperative seizure within 2 days after surgery. The results suggest that the intraoperative EEG may be used not only as a tool for monitoring current status during surgery, but also as a predictive tool to determine risk for postoperative seizure in infants undergoing surgery with DHCA.
Dr. Seltzer's accomplishment will be recognized at the 2014 Child Neurology Society Meeting in Columbus, OH.
UR Medicine Recognized for Stroke Care, Launches Neurocritical Care Program
Tuesday, February 4, 2014
Strong Memorial Hospital has been recognized by The Joint Commission and the American Heart Association/American Stroke Association as a Comprehensive Stroke Center. This designation, which has only been conferred on two other hospitals in New York State, places Strong among an elite group of institutions that provide highly-specialized complex stroke care.
"We are proud that the Joint Commission has recognized our dedicated team of neurologists, neurosurgeons, radiologists, emergency department physicians, nurses, therapists, and staff," said neurologist Curtis Benesch, M.D., M.P.H., the medical director of the URMC Stroke and Cerebrovascular Center. This certification is a testament to their commitment to provide the highest and most comprehensive level of stroke care to our community.
Goodnight. Sleep Clean.
Saturday, January 11, 2014
Sleep seems like a perfectly fine waste of time. Why would our bodies evolve to spend close to one-third of our lives completely out of it, when we could instead be doing something useful or exciting? Something that would, as an added bonus, be less likely to get us killed back when we were sleeping on the savanna?
Sleep is such a dangerous thing to do, when you’re out in the wild,
Maiken Nedergaard, a Danish biologist who has been leading research into sleep function at the University of Rochester’s medical school, told me. It has to have a basic evolutional function. Otherwise it would have been eliminated
.
To read more please see the NY Times article.